Flying Blind Into a Storm of Resistance
Imagine on your next flight across the country that you pull the airline magazine out of the seatback pocket and begin leafing through it. Tucked in the back, behind the stories about cutting-edge restaurants and pet spas, you find this description of the airline’s operations:
Empiric Airlines employs the best, most skilled and most experienced pilots in the industry. That’s why we don’t bother equipping our planes with modern instrumentation. Our pilots rely on their experience, their training, their ability to memorize the landscape and recognize the symptoms of bad weather in order to get you to your destination safely. Usually. Enjoy your flight!
You might say to yourself, “Well, the pilots are experts and most people survive their flights, so I guess they are doing about as well as possible.” Or you might say, “This is unacceptable. The technology to make flying safer exists and is proven to work. There is no excuse for not using it.”

If you are (as I hope) in the latter group, then you might be surprised to learn how doctors prescribe antibiotics. The overwhelming majority of prescriptions are written in the complete absence of any microbiological testing. Instead, doctors employ a system known as empiric prescription: They rely on their experience, their training, their knowledge of the local microbiological “landscape,” and their reading of patient signs and symptoms to guess which bacteria are causing an infection.
Then, they prescribe accordingly.
The toll from this hit-or-miss nature of prescription is substantial. Studies of serious infections show that rates of suboptimal prescriptions typically range from 30 percent to 60 percent. These mistakes more than double the likelihood of death, and contribute to the 100,000 deaths per year in the U.S. from hospital-acquired infections.
This system of empiric prescription was developed during the Golden Age of Antibiotics – roughly 1950-1990 – and it worked wonderfully. Out of the millions of bacterial species on Earth, only a couple dozen are significant human pathogens, and a well-trained doctor can usually identify the most likely culprits by empiric methods.
But doctors can’t empirically distinguish antibiotic resistant strains from antibiotic susceptible ones. In the Golden Age, this was a manageable problem. Resistance rates were usually low, and when they weren’t, new generations of antibiotics emerged to replace the old ones. Antibiotics — combined with clean water and vaccines — pushed deaths from infectious disease to such low levels that microbiology lost funding and became a backwater science.
There was little perceived need for any technological innovations to improve the way that we detect infections, because we had a system that worked astonishingly well: Clean water and vaccines prevented diseases, and if they failed, antibiotics cured them.
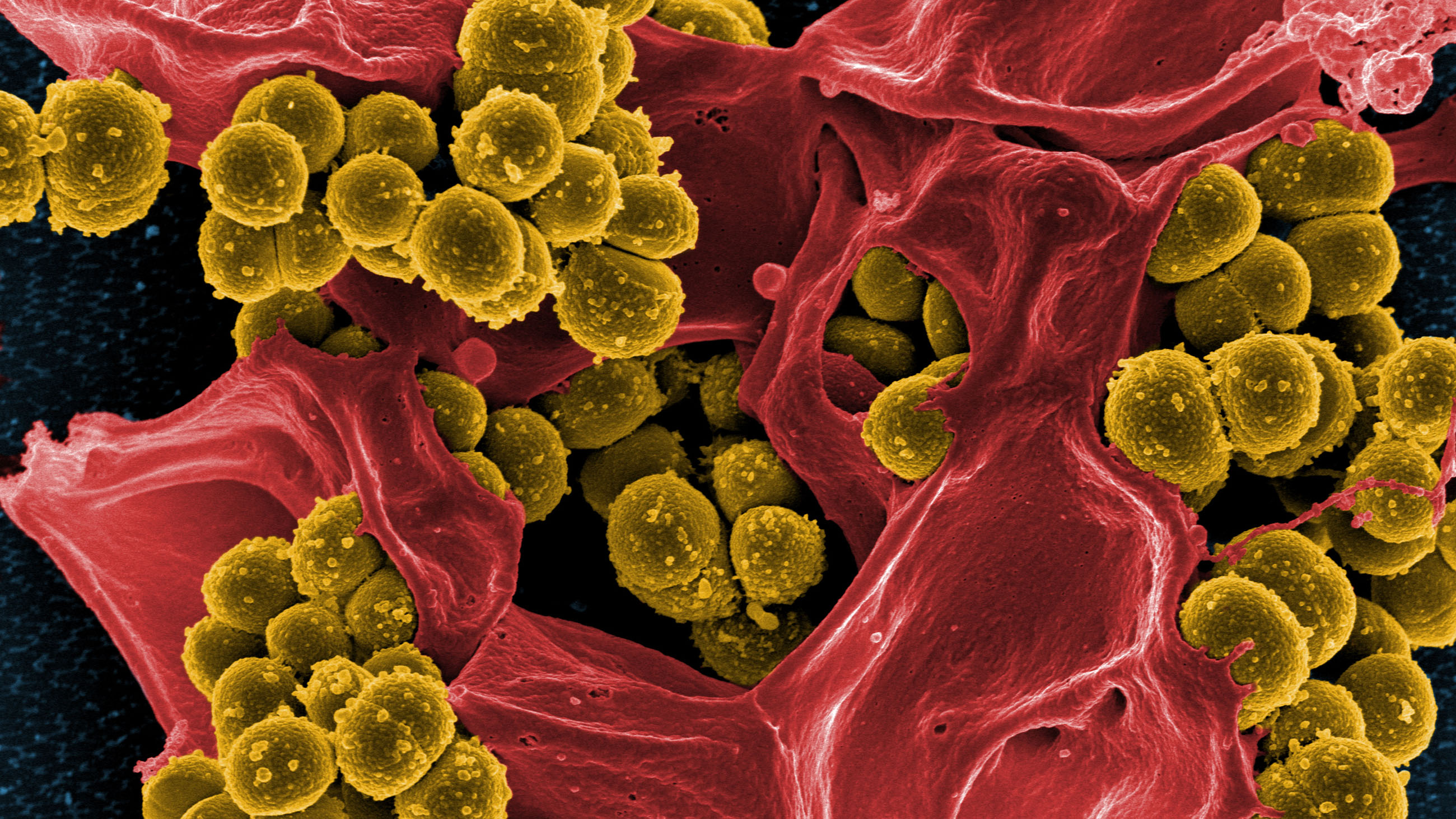
Since that time, the bacteria have evolved but doctors have not. The pathogens are now armed with resistance genes they acquired from harmless soil bacteria, courtesy of antibiotic-fed livestock. But doctors have acquired no powers to intuit when an infection is due to a resistant strain and when it is not. They can note local patterns of resistance and play the odds, but that is all they are doing. When resistance rates reach 50 percent or more, as has happened with methicillin-resistant Staphylococcus aureus (MRSA) in many parts of the world, their guesses as to the best therapy are just that: guesses. Indeed, one study of prescribing practices is subtitled “No better than a coin toss.”

The prevailing attitude of doctors toward the problem of antibiotic resistance is complacence.
The prevailing attitude of doctors toward the problem of antibiotic resistance is complacence. Doctors are aware of resistance as a general problem, but frequently dismiss its importance to their own practice. They consistently underestimate resistance rates, and they are slow to change their prescribing habits as the bacteria change – one study finds that rates of misprescription for viral respiratory infections increase 4 percent for every year of practice.
But in many cases, they have no option but to guess. The standard methods for identifying the bacteria in a patient sample and determining its spectrum of antibiotic susceptibilities have not changed much in decades: a sample is streaked on an agar plate to obtain a single colony, then subjected to an array of biochemical tests and a panel of antibiotics. The whole process takes about three days.
No doctor responsible for a patient with a serious infection could possibly wait that long before beginning antibiotic therapy. If the doctor guesses right, the patient will respond before the microbiology report arrives, rendering it irrelevant. If the doctor guesses wrong, the patient might well be beyond help. Clinical microbiology is mostly used for tracking outbreaks, rather than for directing patient care.
The technology to speed up clinical microbiology exists. Gene-based tests can identify bacteria and detect resistance factors within hours, rather than days. These tests have been shown to improve patient outcomes and despite their high prices, they still reduce costs to the healthcare system. Patients treated with appropriate antibiotics get better sooner.
Even so, these advanced tests have not been widely adopted. Although they may save “the system” money, the system does not make purchasing decisions. Microbiology labs are hospital cost centers, and most of their work is not reimbursed. Adoption of advanced testing technologies is an immediate and easily-identified cost, whereas the benefits are delayed and diffuse, and often accrue to third parties, like insurers – and patients.
The Federal Aviation Administration does not allow airlines to delay adopting advanced safety technologies because it would cost them money. As a result, U.S. commercial airline travel is almost unbelievably safe. If you took a 10,000 mile flight every day, it would be 39 years before your chance of death reached 1 percent. By contrast, every day you spend in a hospital increases your chance of dying from a hospital-acquired infection by 0.05 percent, meaning you’d match that 39 years’ worth of accumulated risk in just 18 days.
It is not possible to make hospital stays as safe as air travel. But the FAA would ground Empiric Airlines in a second for its complacent attitudes. It is not too much to demand that hospitals adopt the best technology available in order to base antibiotic prescription on evidence rather than guesses.
Drew Smith is a PhD molecular biologist who has held positions at several biotech and medical technology startups, most recently MicroPhage, Inc. There he led the team that developed the first FDA-cleared same-day antibiotic susceptibility test for S. aureus bloodstream infections. The test was a commercial failure and MicroPhage declared bankruptcy in 2012. The views expressed in this op-ed are his own.