In El Salvador and Beyond, an Unsolved Kidney Disease Mystery
José Lopez didn’t want to die, but the alternative — having a scalpel plunged through his abdominal wall to install a soft, silicone dialysis catheter — filled him with terror. For weeks in the fall of 2021, the then-34-year-old agricultural worker from Tierra Blanca, El Salvador, had refused the surgery, holding out instead for a miracle from God. Regional lore held that such acts of grace were possible: There was the man from Las Salinas whose invocations had restored his ailing kidneys; the boy from La Noria who was recovering swiftly after devoting himself to the gospel. Through his mounting illness, Lopez clung to the rumors and prayed for a similar deliverance.
But he was running out of time. The fluid buildup in his abdomen had grown so severe he felt like he was choking. He couldn’t stand, eat, or sleep. His legs had gone completely numb, and he felt phantom ants crawling across his palms. He had lost nearly half his body weight, and sharp knobs of bone poked through his skin like tentpoles. The primary indicator of kidney function, creatinine levels, are considered high when they reach 2 milligrams per deciliter of blood. By 6 mg/dL, they indicate severe, life-threatening kidney disease. Lopez’s were at 35.
Doctors had delivered a stark ultimatum: Begin dialysis or die. But Lopez had seen dialysis firsthand. He was the eighth man in his family to develop chronic kidney disease of unknown origin, or CKDu, a beguiling and fatal illness that was decimating entire communities across Central America and other warm, agricultural locales around the globe. Just in the last three years the disease had claimed his beloved father, Vitelio, and two uncles. The only adult Lopez men who remained were José and his two younger brothers, each of whom had the disease and were inching toward similar fates. Many of José’s relatives had spent their last months receiving dialysis treatments before eventually succumbing — José understood that the catheter was the end of the line.

Nevertheless, his then-4-year-old son, José-Vitelio, finally broke through to him. The whole family — his mother, María Luisa; his wife, Marta; his then-13-year-old son, Edwin — had gathered at his bedside and were begging him to reconsider when, Lopez recalled, the child piped up: “We don’t want to be left alone,” he said. The tiny plea nudged Lopez to seek help. The family called a car, and Lopez was driven to the San Juan de Dios National Hospital in nearby San Miguel. The catheter was installed under local anesthetic, and several days later Lopez enrolled in the Jiquilisco municipality at-home peritoneal dialysis program.
“Here I am, still fighting,” he said, seven months after the procedure.
Since the 1990s, tens of thousands of people across Central America, Sri Lanka, India, and elsewhere have been killed by CKDu in a ballooning epidemic that has baffled researchers, overwhelmed health care systems, and wiped out entire families. Agricultural communities seem particularly vulnerable, but the disease has surfaced among other workers, too. The precise number of deaths is unknown, but in locales where the disease is endemic, such as the Bajo Lempa region of El Salvador, experts estimate that up to one quarter of the male population has CKDu. (It affects men at roughly two times the rate of women, according to the International Society of Nephrology.) It cannot be cured, only treated with dialysis, and in rural communities such as Tierra Blanca, it is rare for dialysis patients to survive more than a few years. But despite its devastating toll, scientists have struggled to determine what causes the disease or how it develops.
Two competing hypotheses have emerged to explain the epidemic. The first suggests that the main cause is an unknown toxic agent — pesticides, perhaps, or heavy metals or silica. The second points to heat stress and dehydration, amplified by brutal working conditions and an increasingly warmer climate. Many researchers have accepted the possibility that the disease may emerge from the synergistic effect of two or more causes working in tandem. Yet the debate over the primary driver of the epidemic — toxins or heat stress — remains unresolved.
The lingering scientific uncertainty holds profound implications for policy, prevention, and treatment. Without a clear scientific consensus, governments, non-governmental organizations, and doctors are divided over how to best coordinate a response to the epidemic, a gridlock that has sometimes flared into outright hostility: At least two individuals involved in CKDu research and policy claim to have received death threats and violent attacks because of their positions. In recent years, however, studies from both sides of the debate have offered intriguing new clues, giving scientists renewed hope that someday the scientific stalemate may be broken, and the mystery of this deadly disease finally unlocked.
Until then, the only weapon CKDu patients like José Lopez have against the disease is dialysis. Of the two varieties of the treatment — hemodialysis, which requires an expensive machine to remove toxins from the blood, and peritoneal dialysis, in which the patient’s abdomen is flooded with a solution that leaches toxins from the abdomen’s blood vessels — Lopez can only access the latter. The treatments are relatively inexpensive and can be performed at home, but it must be done four times a day. His son Edwin administers the treatments. Lopez wants Edwin to see the disease close-up, as he had with his own father. He hopes it will encourage the boy to study hard in school, so that he might avoid the brutal agricultural labor that Lopez believes is responsible, in one way or another, for his illness.
“You have an example, right in front of your eyes,” Lopez often tells his son. “Look at what has become of me. This is how the fields left me.”
Tierra Blanca, a small agricultural community of several thousand, is nestled within the verdant coastal lowlands of El Salvador’s Bajo Lempa region. Nearby, a few squat volcanoes rise above the haze of burning sugarcane fields, and to the south the seafood-rich estuaries of the Bay of Jiquilisco give way to the open Pacific Ocean. West of town, the Lempa river braids listlessly through endless tracts of farmland, depositing the mineral-rich silt that makes this region one of the most fertile in the country.
Lopez began cultivating the land around Tierra Blanca when he was 12 years old. His father, Vitelio, and grandfather, Juan-Francisco, would load the boy into an ox cart before sunrise and go clattering down the rocky trail that led into the fields, where roads had not yet been laid. They rented a small subsistence plot from some landowners in San Marcos, and there Lopez learned how to farm — how to drive the oxen and mix an organic pesticide, measure seed depth with his thumb, and trench canals to drain the monsoon rain. Although Lopez was a good student, school supplies were expensive, and he dropped out in the seventh grade.
Back then, in the late 1990s, kidney disease had not yet been widely identified as a killer of El Salvador’s working men and women. The country had just emerged from a brutal 12-year civil war that had claimed the lives of 75,000 people, mostly civilians. In the Bajo Lempa, the health care system — insofar as it existed at all — was privatized and costly. A common saying in the region at the time went, “you pay or you die,” and most of the men Lopez worked with in the fields simply could not afford to pay. When they died, very few people ever questioned why.
That began to change in the late 1990s, when Julio Miranda, a local community organizer and health care activist, started asking questions about the excessive number of funerals that were taking place in Tierra Blanca. “People were dying one after another,” Miranda recalled. “And without any sort of diagnosis.” But Jesus Dominguez, a Spanish doctor who had come to El Salvador to render medical care during the civil war and who worked closely with Miranda, started to recognize the shared symptoms of the deceased. “It was clear,” he said, speaking over Zoom from France, where he currently lives. “They were dying from kidney failure.”
In the early 2000s, Miranda, Dominguez, and a handful of other activists began collecting urine samples from field workers over the age of 30, looking for the elevated protein levels that often signaled kidney disease. Individuals with worrisome levels were instructed to go to a lab for blood work. Dominguez still vividly recalls the night the first batch of test results came back from the lab. The team stayed up all night in Miranda’s living room, poring over the results, checking them again and again. Finally, in the morning, Dominguez recalled turning to Miranda. “This is a massacre,” he said.
“We had the death sentences of hundreds of people in our hands,” Dominguez said in a recent interview, later adding: “I was in shock.”
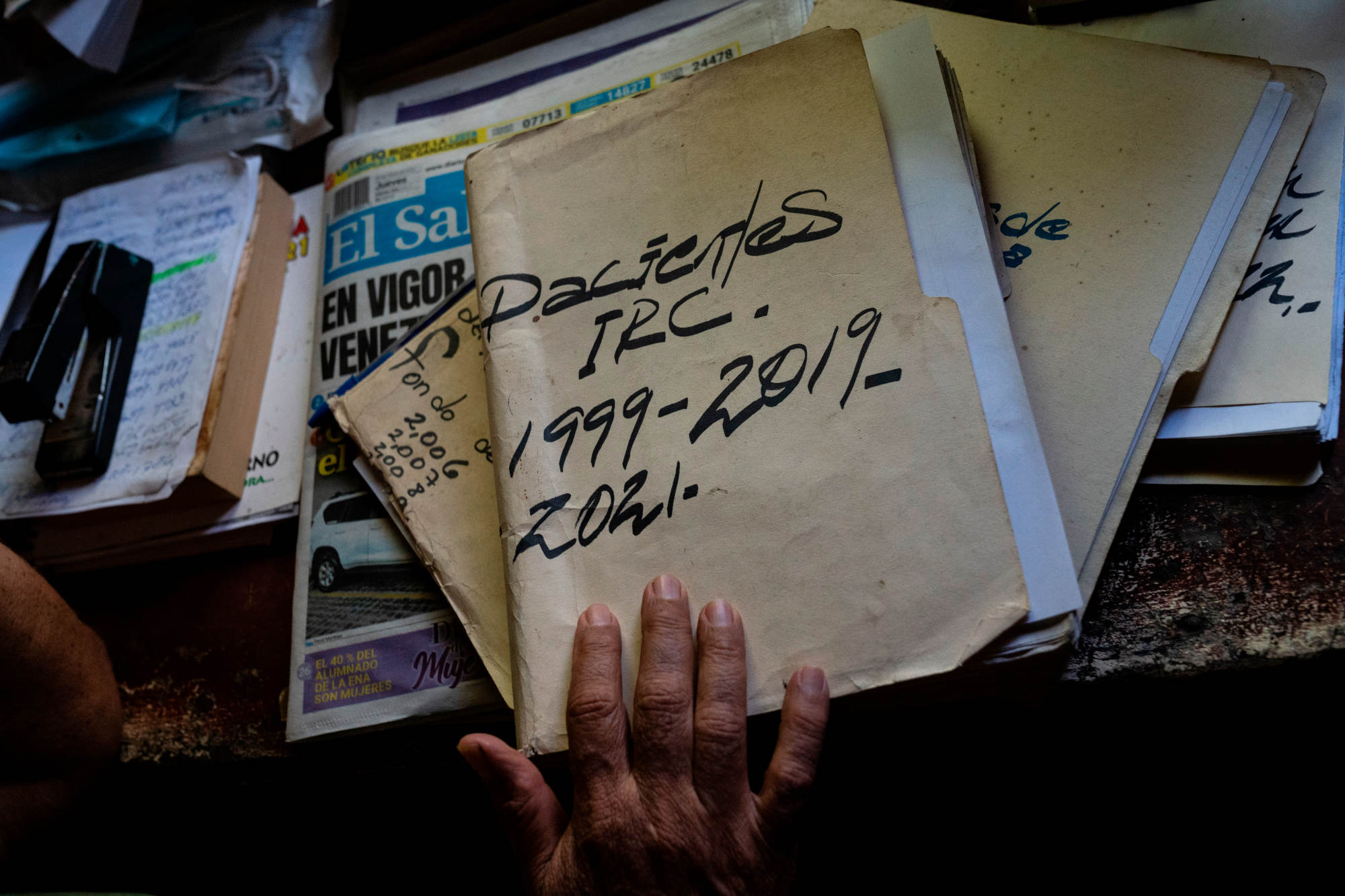
As the scope of the emerging epidemic began to dawn on the activists, Miranda immediately set about establishing a registry of everyone in the area who was showing signs of kidney disease. The data, he hoped, might galvanize the health ministry into investigating the situation. This registry — which included as much medical information as possible about each patient — was new.
But in a separate notebook, Miranda had already begun to list the dead.

One morning in June of 2005, José Lopez entered the bedroom of his grandfather, Juan-Francisco, to rouse the older man for work. Although Juan-Francisco had seemed perfectly healthy just the day before, Lopez now found him gravely ill. He was too weak to stand, and after several failed attempts to get out of bed he simply hung his head and began to cry. “The man upstairs is calling me,” Lopez recalled his grandfather saying.
Juan-Francisco died three weeks later. The family paid for a modest funeral service that included chicken tamales and black coffee, and a hearse to lead the funeral procession to the Tierra Blanca cemetery. While mourners sang religious hymns, the body of Juan-Francisco was interred in an unadorned cement tomb with ample space surrounding it — the family plot was sparsely populated then. He was the first Lopez man to die of CKDu, and the first from their family to be added to Julio Miranda’s list of the dead: Number 62.
The campus of Rosales National Hospital, the centerpiece of El Salvador’s public health care system, sprawls across several city blocks in the heart of the nation’s capital, San Salvador. Throngs of patients, staff, and students jostle between the tall, hangar-like buildings, while shotgun-toting security guards stand at each of the hospital’s entrances. Rosales was built in the late 19th century with money from a public lottery, and a spirit of chance still lingers: Patients complain of erratic care and long waits, doctors of chronic underfunding and insufficient personnel. And nowhere on the campus is more teeming with fringed nerves than the kidney ward, which according to the head of nephrology, accounts for some 60 percent of the hospital’s admissions.
If Rosales is chaotic now, it was far worse in 1995, when Ramón García-Trabanino arrived as a seventh-year medical student, ready to begin his hospital internship. Back then, there was no dedicated nephrology ward, only an internal medicine wing that housed a few old hemodialysis machines. When he started at Rosales, the young doctor supposed he would be treating the full range of conditions he had studied in school — strokes, neurological disorders, pneumonia. Instead, the unit was flooded with kidney patients, wave after wave of them, many on the brink of death.
“The amount of patients was just overwhelming,” recalled García-Trabanino, who now, at 51, directs a private dialysis clinic in San Salvador. “It was like an erupting volcano.”
In medical school, García-Trabanino had learned the textbook profile of a kidney disease patient: old, diabetic, hypertensive, equally male and female. He quickly noticed that the influx of sick people arriving at Rosales did not conform to that profile at all.
“They weren’t diabetic. They didn’t have high blood pressure,” said García-Trabanino. “They were in their 20s, 30s, 40s — they were young. They attended once, twice, and then they died.”




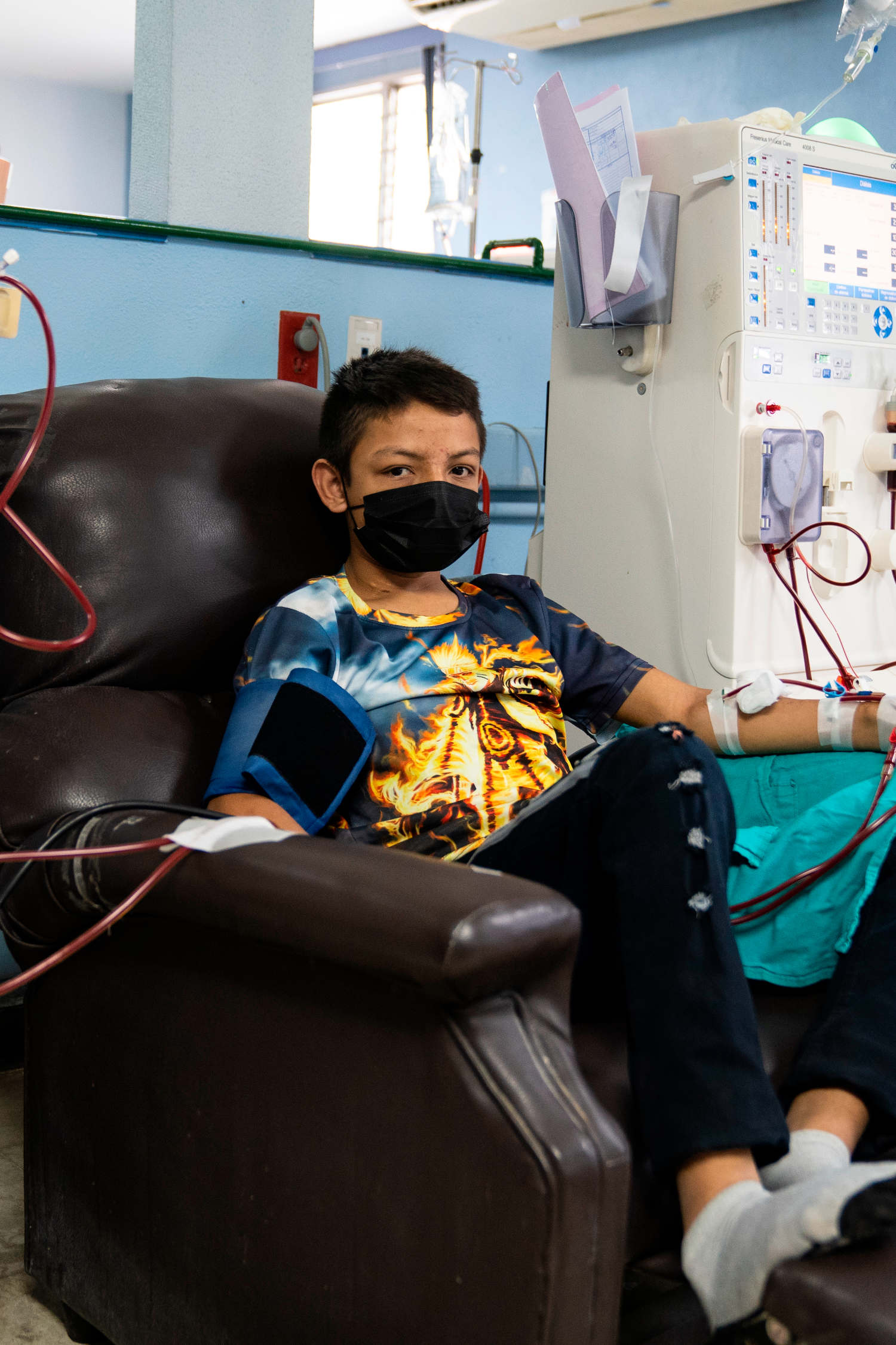

The patients were treated with an antiquated technique called rigid-catheter peritoneal dialysis. A stiff tube was inserted into their abdomens and their peritoneal cavities flooded with a toxin-absorbing fluid, a process that, to be effective, should have been performed daily. Because of the overwhelming demand, patients at Rosales only received one treatment per week, and each time they returned a new catheter would have to be installed. This alone was dangerous — if doctors accidentally nicked the patient’s bowels or liver during the process they could die, and frequently they did. García-Trabanino, who says he still has nightmares from this time, vividly remembers the first patient he lost. His name was Ramón, just like him.
Perhaps most frustrating of all for the young doctor, was that nobody could explain what was happening. Even Ricardo Leiva, the chief nephrologist, was dumbfounded. “We kept asking ourselves, ‘where are they coming from?’” recalled Leiva. “It was overwhelming the hospital. So that’s why we did the first research.”
In the fall of 1999, García-Trabanino, Leiva, and a few others began to investigate. They conducted interviews with 202 patients, collecting demographic, occupational, geographical, and clinical data. They found that only one-third of the interviewees had known risk factors for kidney disease such as diabetes or hypertension. The rest had “unusual characteristics that were not associated with the known risk factors,” according to the resulting study. Of this latter group the majority were men, worked in agriculture, and had been exposed to pesticides. They also came from hot coastal areas like the Bajo Lempa region, where Tierra Blanca is located.
Published in 2002, the study concluded that a novel group of end-stage kidney patients had been identified, who seemed to “lack a cause for their disease.” The researchers suspected a relationship with occupational exposure to agrochemicals, but stated that further research was needed. It was the first description of the emerging epidemic in the scientific literature, and for his efforts García-Trabanino was awarded the National Medical Investigation Prize, the country’s top honor for medical research.
In the years preceding the disease’s identification, pesticide use had been on the rise in Central America. According to the Pan American Health Organization, or PAHO, which serves as the World Health Organization affiliate for the Americas, by the end of the 20th century, the region had the highest per-capita use of pesticides of anywhere in the world. Between 1994 and 2000, imports of pesticides to Central America rose by 32 percent. The average agricultural worker in Central America in 1992 used 9.9 pounds of pesticides per year. By 2000, that number had risen to 14.8 pounds. The most commonly sold pesticide in El Salvador, paraquat, has been banned by dozens of countries because of its acute toxicity to the lungs, liver, and kidneys. And although a link has not been conclusively established between paraquat and CKDu, it remains one of the prime suspects the toxic-exposure researchers are investigating.
Nevertheless, the pesticide hypothesis encountered an early stumbling block. In 2005, García-Trabanino’s team published a study that compared CKDu prevalence in a population of men (mostly agricultural workers) in the Bajo Lempa, which is near sea level, with men in Sesori, which is farther north and higher in altitude. The findings perplexed the researchers. Although the two populations cultivated the same crops, using the same pesticides, the men at sea level were eight times more likely to have CKDu. It was a serious blow to their initial hypothesis. “It was not related, at least not to pesticides,” said García-Trabanino. “It was related to the region. So, we had to come up with new ideas.”
Meanwhile, other hotspots were gaining attention. In neighboring Nicaragua, Catharina Wesseling, an epidemiologist who then directed an occupational health and safety initiative called the Program on Work and Health in Central America, began hearing reports of a fatal kidney disease impacting workers at a sugar mill near the town of Chichigalpa. In Sri Lanka, doctors in Anuradhapura District, in the North Central Province, were beginning to notice an alarming uptick in kidney patients arriving at their hospitals. In the state of Andhra Pradesh in India, and in the El-Minia Governorate in Egypt, similarly worrisome trends were coming into focus. Locales where the disease appeared endemic generally shared two conspicuous features: They were heavily agricultural, and they were hot.
The government in El Salvador, despite having awarded García-Trabanino the National Medical Investigation Prize in 2000, had largely ignored the epidemic in the decade following its emergence. That began to change, however, when in 2009 the country elected its first leftist president, the Farabundo Martí Liberation Front candidate, Mauricio Funes, putting an end to decades of conservative rule. Among the new president’s priorities was a reboot of El Salvador’s public health care system, which had atrophied under years of neoliberal policies designed to encourage privatization. To oversee the reforms, Funes appointed a new health minister, María Isabel Rodríguez, a doctor who had worked for PAHO and was keenly aware of the unfolding health crisis. Under Rodríguez’s leadership, a young nephrologist named Carlos Orantes began to spearhead the first official government investigation into the illness.
In the fall of 2009, Orantes and his team conducted the largest CKDu study undertaken up to that date, surveying 775 individuals in the Bajo Lempa region in order to better understand the disease’s prevalence and associated risk factors. Many of Orantes’s findings — such as the conspicuous absence of traditional risk factors, the higher burden among men than women, and the preponderance of the disease in agricultural communities — dovetailed closely with those of García-Trabanino and others from previous years. Unlike García-Trabanino and Wesseling, however, who by then had begun exploring other possible causes, Orantes determined that toxins, especially pesticides, deserved renewed scrutiny. Of the men that responded to his survey, 82.5 percent reported contact with agrochemicals, the highest percentage of any potential risk factor screened for by the study. The report noted that field researchers involved in gathering data had observed dangerous agrochemical handling practices and had become aware of a long history of indiscriminate aerial crop dusting in the Bajo Lempa region. The study concluded that certain risk factors “may act synergistically” and that although the specific etiology remained elusive, the hypothesis of an environmental toxin “cannot be ruled out.”


The study, with its renewed suspicions of a toxin-based etiology, formed the basis of the new health minister’s stance on CKDu. “The evidence suggests agrochemicals and pesticides as possible associated factors and this has to be investigated,” said Rodríguez in a 2013 interview with MEDICC Review, a Latin American health journal. Press coverage of the issue around this time tended to follow the government’s lead, suggesting in article after article that there was a potential link between pesticides and the epidemic. During this time, researchers like García-Trabanino and Wesseling say they began to worry the public was being served a convenient narrative, one that provided an easy answer — but wasn’t supported by the science.
In April of 2013, El Salvador hosted a meeting of the Council of Ministers of Health of Central America and the Dominican Republic, which culminated in the signing of the Declaration of San Salvador, which recognized CKDu as “a major public health problem,” and signaled a willingness to tackle the epidemic on a regional level. Before the document was signed, however, a vigorous debate broke out amongst the attendees over whether the role of pesticides was being overstated. According to an account of the meeting by the Center for Public Integrity, representatives of El Salvador’s ministry of health asserted that the most compelling data suggested a high association between CKDu and agrochemical exposure, while other researchers, including García-Trabanino, argued that a definitive link had never been established in the scientific literature. Rodríguez put an end to the debate by declaring, “What has been presented here is scientific fact, and I will defend it with my nails!” She showed the crowd a set of brightly painted red nails, the room erupted with laughter, and the document was signed.
But the debate over the role of pesticides did not end there. In the summer of 2013, Rodríguez and Salvador Menendez, the mayor of a municipality called San Luis Talpa that had been devastated by the epidemic, launched a campaign to prohibit the use of 53 agrochemicals that were suspected of being deleterious to workers’ health. The proposal ignited a fierce public discourse, whose fault lines hewed closely to what had been argued by each side in the Council of Ministers meeting. But as the scientific debate entered the public realm — through press coverage and word of mouth — the conversation quickly soured, before finally exploding into outright acrimony and accusation.
The mudslinging went in all directions: García-Trabanino accused the health ministry of distorting science in order to score a tidy political victory. The powerful agricultural sector, according to a newspaper article at the time, made sensational claims that El Salvador’s agricultural output would plummet by 80 percent if the ban went through. Orantes says he was maligned as an “eco-fanatic” who was “obsessed with agrochemicals.” In turn, García-Trabanino says he was publicly disparaged as being a shill for the agricultural sector (he insists he never took money from agricultural groups) and was so widely vilified that Julio Miranda had to warn him against returning to Tierra Blanca, where he had been conducting research. The fieldworkers whose health had been the focus of his career were now a threat to his safety. García-Trabanino says he received a death threat during this time. For Mayor Menendez it was even worse: He claims that on three separate occasions, the armored car he was riding in was fired upon by unknown assailants. Each time, he notes, he escaped without injury.
On September 5, 2013, El Salvador’s legislative assembly voted to approve the agrochemical ban. But in a move that surprised many, President Funes himself declined to sign the prohibition into law, instead returning it to the legislative assembly where it entered a state of legal limbo, neither vetoed nor approved. (In 2016, Funes was embroiled in a corruption scandal that prompted him to flee to Nicaragua, where he was granted asylum. He maintains that he is the victim of political persecution.) The degeneration of the public debate and the failure of the agrochemical ban to become law marked the end of what many had hoped would be a high-water mark for CKDu research and action. After that, in 2014, a new administration took power, and Rodríguez, who was over 90 years old, retired from her role as health minister. Orantes’s investigative unit was dissolved, and he was reassigned to a different department. An effort to revive the agrochemical ban foundered, a national action plan that Orantes had developed was cast aside, and the stipulations of the Declaration of San Salvador — which many believed had offered the brightest hope for regional action to combat the epidemic — went largely ignored. It was a “regression that left us in an even worse state than when we started,” recalled Orantes.
When his grandfather died of kidney failure in 2005, José Lopez, like most people in Tierra Blanca, had never heard of CKDu. But in the years that followed, insuficiencia renal, as it became known, grew into a dominant feature of life in the Bajo Lempa. Billboards sprung up along the highway connecting the region to San Salvador, advertising private dialysis clinics that few could afford. Local funeral homes began catering almost exclusively to victims of CKDu. (“It’s very rare for someone to die from a different disease,” one mortician said in an interview with Undark.) Nearly everyone was touched, directly or indirectly, by the epidemic. Many field laborers were diagnosed but continued working — compelled to by the grinding poverty endemic to the region. Doctors often dispensed paradoxical advice: Reduce work hours and purchase costly medication.
By the 2010s, the disease was ravaging the Lopez family. One of Lopez’s uncles had succumbed in 2009 and now rested beside Juan-Francisco in the Tierra Blanca cemetery. Two more uncles were sick, as was Lopez’s father, Vitelio. Worst of all, though, was that both of Lopez’s younger brothers had developed the disease — Francisco at the age of 10.

Up to that point, however, Lopez himself had managed to avoid the fate of the other men. His kidneys remained healthy, and he had fallen easily into his role as the family’s main breadwinner. Back in 2008, he had married his wife, Marta, and shortly afterwards they had Edwin. Lopez continued to work the fields, and sometimes his ailing father would visit him there, nostalgic for the years they had labored together. The two men would sit together and admire the crops, breathing in the sweet earthy scent of the sprouting sugarcane. “This produce is beautiful,” Lopez recalled his father saying. “Perhaps it’s even better than when I grew it.”
But Lopez’s luck eventually ran out. In 2015, blood tests revealed that his creatinine levels were slightly elevated. He showed no symptoms, but doctors nevertheless prescribed medication and told him to reduce his work hours. He tried to follow their orders, but his family’s diminishing resources soon made it impossible. Within months, he was back in the fields, working full time.
Lopez’s father passed away on April 13, 2019. As with the previous deaths, the family held a two-day vigil and a service with chicken tamales and black coffee. There were religious hymns and a solemn procession to the graveyard. Then Vitelio was laid to rest in the family plot beside his father and brother.
For Lopez’s mother, María Luisa, the hardest part of losing her husband was the sense that his death foreshadowed the fate of her boys, all of whom now had CKDu. “There is going to come a day where my kids are going to go,” she said one afternoon. “It’s a lie to say that they are going to get cured.”
Nobody was ever cured. Shortly after Vitelio’s death, both of Lopez’s remaining uncles followed. There were more tamales and coffee and religious songs. In just over two years the Lopez family plot filled with three fresh graves. And elsewhere in the cemetery, other fresh graves were appearing, too. All across the region, hundreds of families were suffering the same fate.


As the debate over agrochemicals was ramping up in El Salvador in the early 2010s, a competing hypothesis was simultaneously gaining traction within CKDu research circles. Championed by toxic-exposure skeptics like Wesseling, the epidemiologist from the Program on Work and Health in Central America, the theory proposed that heat stress and dehydration, not toxins, were the primary drivers of the CKDu epidemic. The heat stress hypothesis has since garnered widespread support, emerging as the chief competitor to the toxic-exposure theory.
A substantial body of research supports the heat stress hypothesis. In 2012, Wesseling and Sandra Peraza, a chemist at the University of El Salvador, published a study that compared creatinine levels in various communities across the country. Two of the communities cultivated sugarcane as their main economic activity, although one was at sea level while the other was higher in elevation and significantly cooler. The findings echoed the 2005 analysis spearheaded by García-Trabanino, the nephrologist who had first identified the epidemic in the late 90s: Despite employing similar agricultural practices — including the use of pesticides — the high-elevation community only had a 3.6 percent rate of elevated creatinine levels among men. On the rural coast, however, the rate was 28.3 percent. “The major difference,” the team wrote, “seems to be ambient temperature in combination with strenuous work.”
In 2014, García-Trabanino, Wesseling, and a handful of other researchers conducted a study that further bolstered the heat stress hypothesis. The team tested biomarkers of renal function, such as creatinine and uric acid, in sugarcane workers both before and after a day’s shift in the fields. Just one shift, the team found, was enough to substantially increase the prevalence of heightened creatinine levels among the participants, from 20 percent to 25 percent. Similarly, the prevalence of elevated uric acid rose from 26 percent to 43 percent over the course of a shift. Furthermore, the researchers found an association between heat and creatinine levels, observing a 2 percent increase in creatinine for every one degree increase in temperature. The study provided some of the first detailed data linking heat stress to decreased renal function and stated in its conclusion that “work practices must be improved with more frequent breaks, access to shade during breaks, larger intake of water, and probably also salt.”
Based on findings such as these, La Isla Network, or LIN, a non-governmental organization that focuses on CKDu research and advocacy, began designing and implementing intervention studies in 2015 at El Ángel sugar mill in El Salvador. By introducing a simple program they called “water, rest, and shade” (provision of clean drinking water and electrolyte powder, enforcement of frequent and mandatory work breaks, and the offering of a mobile shade structure) the LIN researchers hoped to do two things: confirm that certain elements of the heat stress theory were correct and determine whether the interventions could reduce workers’ risk.
In 2018, the LIN team, which had by then hired Wesseling as chief epidemiologist, published its results in the Scandinavian Journal of Work, Environment, and Health, a highly cited international occupational health journal. The paper observed two groups of workers, one on the coast and one farther inland. A measurement of kidney function based on creatinine levels was calculated for each worker at the beginning of the harvest, as well as just before the interventions began and again at the end of the season. The interventions, which were implemented two months into the five-month cane cutting season, were shown to slow the rate of kidney decline over the course of the harvest. Amongst the inland group, kidney decline leveled out completely following the intervention. Although the sample size was small, owing to logistical difficulties, with just 40 people in the coastal group and 40 in the inland group, the researchers were encouraged by what they claimed was the first objective dataset demonstrating the efficacy of LIN’s occupational interventions.
“In El Salvador, we got the first evidence that heat stress as such can produce incident kidney injury during the harvest,” said Wesseling, talking over Zoom from her home in Costa Rica. Subsequent studies at Ingenio San Antonio, a large sugar mill in Nicaragua, have provided further evidence that the interventions are effective — and that the heat stress hypothesis is strong.
Although Wesseling doesn’t discount the possibility of other contributing factors, such as toxins, she nevertheless believes that heat stress and dehydration alone are sufficient to explain the epidemic. She and her colleagues at La Isla Network have even developed a hypothesis for a heat-related pathogenesis of CKDu, describing in a 2020 paper how “the release of pro-inflammatory substances from a leaky gut and/or injured muscle” could induce kidney inflammation, which is associated with kidney injury.



Other researchers aren’t so convinced. Despite widespread acceptance that heat stress may play a role in the disease’s advancement, Marc E. De Broe, the former head of the department of nephrology at the University of Antwerp in Belgium, and Channa Jayasumana, the former health minister of Sri Lanka, believe that something else must be causing the disease to take root in the first place. How could heat alone, they argue, explain the sudden emergence of CKDu in the 1990s, when temperatures in Central America and Sri Lanka were relatively stable over the 20th century? Or the patchwork distribution of CKDu-endemic areas in Sri Lanka, despite a fairly uniform climate and similar work practices? Or the existence of kidney-injury biomarkers in Central American adolescents who had never worked? Wesseling argues against many of these points on the basis of insufficient or flawed research, yet many researchers remain unconvinced that heat alone can explain the totality of the epidemic’s features. As García-Trabanino put it: “Heat stress seems to be the trigger. But the bullet is already loaded.”
A recent study from Sri Lanka seemed to confirm the doubts of many heat stress skeptics. A team from the University of Ruhana compared three occupational groups — rice paddy farmers, tea-plantation workers, and fishers — who labored under varying levels of heat exposure. The team found that the group that worked the longest hours in the hottest weather, fishers, demonstrated the lowest CKDu burden, at 5.36 percent. Meanwhile, paddy farmers, who labored at comparatively low to moderate temperatures, reported a higher incidence of susceptibility, at 13.33 percent. “Our findings indicate that heat stress and dehydration are unlikely to be the leading drivers of CKDu in Sri Lanka,” the study concluded, adding, “Heat exposure may act synergistically with other risk factors in causation and progression of CKDu.”
The scientific uncertainty has spurred researchers to continue the hunt for García-Trabanino’s elusive “bullet.” Richard Johnson, a nephrologist at the University of Colorado, is investigating the potentially toxic impact of silica, which is released when sugarcane fields are burned before the harvest. Sandra Peraza, an advocate of heat stress as a major driver of CKDu, is nevertheless curious about the role that genetics may play in predisposing certain populations to the illness. In Sri Lanka, however, the majority of research has focused on toxins, and how various toxic substances may interact with each other to produce the disease.
That each of the two major hypotheses — heat stress and toxins — can be so easily associated with a particular geographical hotspot raises a simple but crucially important question: Are researchers in Central America and South Asia even studying the same disease?
Most believe so, but it cannot yet be definitively proven. One shortcoming that has dogged CKDu research over the years is the absence of a universally accepted definition of the disease. CKDu patients are generally diagnosed clinically, when they present with indicators such as elevated creatinine levels or symptoms of chronic kidney disease in the absence of classic risk factors such as diabetes or hypertension. Pathologically, the disease is generally described as tubulointerstitial nephritis, meaning it causes damage to a certain part of the kidney’s filtering units, the tubules, as well as the tissue that surrounds them. But tubulointerstitial nephritis is too common a type of kidney damage to be useful as a diagnostic criterion for CKDu. Still, a 2018 biopsy study led by Julia Wijkström, a Swedish renal pathologist who works closely with LIN, concluded that there were “many similarities in the biochemical and morphological profile of the CKDu endemics in Central America and Sri Lanka, supporting a common etiology.” Wijkström’s team, however, also noted some differences, and suggested that larger biopsy studies were needed.
In an effort to gain a better understanding of the disease’s pathology, a team in 2018 led by Marc E. De Broe (and that included Orantes, the nephrologist who had led El Salvador’s CKDu investigative unit before the pesticide debate of 2013) conducted a kidney biopsy study that resulted in a discovery that intrigued the scientists. The cells of all complex organisms contain tiny garbage collectors called lysosomes, which are responsible for breaking down and eliminating waste from the cell. In the specific kidney cells targeted by CKDu, those lysosomes are supposed to be round or oval-shaped, and of a certain minuscule size. De Broe’s team, however, found that in CKDu patients, the lysosomes of those cells were enlarged and oddly shaped, like amoebas. That type of lysosomal disfigurement was commonly seen in another group of patients — those who had ingested known nephrotoxic medications. The team then conducted a rat study where they were able to recreate the same lysosomal abnormalities by feeding the rats a drug that is toxic to kidneys called cyclosporine. Another group of rats who were not fed cyclosporine — but who were dehydrated — did not develop the misshapen lysosomes. It was enough for the team to conclude that they had found hard evidence that toxins could cause CKDu.
Additionally, within the aberrant lysosomes the team observed mysterious clumps — or aggregates, as the scientists called them — of an unknown substance, visible under electron microscopy. Cynthia Nast, a renal pathologist who worked on the study, said that the aggregates could be a number of things — the remnants of damaged cell proteins, for example, or the breakdown product of a toxic substance. They might also be, however, the toxic substance itself — minuscule accumulations of whatever agent is causing the disease. But Nast cautions against getting ahead of the science. “Can it maybe at some point inform about causality? Maybe. But we don’t know that yet,” she said. In the meantime, Nast remains satisfied that her team’s research has provided the most compelling evidence yet for a toxic etiology. “I am completely a believer that this lesion is a marker of a toxic nephropathy,” she said.
But the study, which was published in the prestigious nephrology journal Kidney International, proved controversial. Wijkström, the Swedish pathologist, and a handful of other researchers published a letter to the editor of the journal that claimed they had found the same aberrant lysosomes in five randomly selected healthy kidney donors. In response to the letter, the authors of the original paper replied that the scientists had misunderstood the diagnostic criteria for the lysosomes, and that the lysosomes they had found were not the same as the ones described in the original paper. Within the CKDu research community, attitudes toward the Kidney International paper seemed to follow the general contour of the wider CKDu debate: The heat stress people, like Wesseling, viewed Wijkström’s letter as a convincing debunking of the lysosomal findings. Meanwhile, the toxic-exposure supporters, such as Nast, viewed the author’s reply to Wijkström and the others as proof that their claims had little merit. To this day, even the editor of Kidney International, Pierre Ronco, remains torn. “The arguments are well balanced, and the question of the cause remains quite open,” he wrote in an email to Undark.
If there’s anyone who can be said to straddle the divide between the heat stress camp and the toxic-exposure camp, it might be Johnson, the University of Colorado nephrologist. Johnson worked closely with LIN and the heat stress advocates in the first part of the decade, but his research has now shifted toward toxins. For Johnson, however, neither side has decisively proven its case. “If you hear anyone who says it has got to be a toxin, or it has got to be heat stress,” he said during a call in July of this year, “you have to realize that they’ve been convinced when we haven’t totally proven it.” Johnson acknowledges the significant contributions of scientists from each side of the debate and says that there simply has to be more research. “The lysosomal changes favor a toxin, but there’s a lot that favors heat stress,” he said. “You keep going until you have absolutely definitive evidence.”
And so, the researchers keep going. La Isla Network plans to expand its occupational interventions to more workers through an initiative called Prevention, Resilience, Efficiency, and Protection, or PREP 4 Change. The Belgian team that first identified the strange lysosomes is conducting further research to buttress their claims. And perhaps most significantly, in 2020 the U.S. National Institutes of Health announced a $4 million grant for the future study of CKDu. The project, called the CURE consortium, will be by far the largest effort yet to understand the disease, and researchers from both sides of the debate are hopeful for what it may discover. “This one is getting big and really interesting,” said García-Trabanino. “We hope to finally untangle the mystery and stop the massacre.”
Just beyond the western edge of town, tucked serenely within a dense grove of mango, cashew, and guanacaste trees, lies the Tierra Blanca cemetery. Its brightly painted tombs suit the wild tangle of the encroaching flora, like enormous tropical flowers. Overhead, the canopy teems with squawking songbirds, but otherwise the cemetery is still. A two-track road weaves delicately through the headstones, just wide enough for a car to pass, and near the far southern edge, beneath the spindly bough of a Morro tree, is the Lopez family plot with its six modest graves.
On a bright afternoon in late March of this year, Lopez’s son, Edwin, and mother, María Luisa, headed to the cemetery. The number of graves in the Lopez plot had doubled in the previous three years, and their grief was still raw. When María Luisa reached the light-blue cement tomb of her husband, Vitelio, she fell silent, her eyes welling with tears. “All I remember is the sadness,” she said, recalling the day the family buried Vitelio. She scanned the six graves with a look of disbelief. “It’s not easy knowing that your entire family died from the same disease,” she said. “It’s like a chain that’s tied to them.”
Edwin kneeled beside his grandfather’s grave and began to sweep it clean with a fallen tree branch. The deaths of his family members have left him feeling abandoned, he explained. Those who remain are forced to struggle forward with whatever resources are left, and must grow up and live without parents, or uncles, or grandparents. “Almost all of them are dead,” he said. But for him, the worst has not yet happened. “What I’m really scared of is one day losing my father.”


Lopez, who was far too ill to accompany the others to the cemetery that afternoon, shares his son’s fear. “I am scared, I will tell you that,” he said, speaking of the prospect of leaving his family behind. To temper the worry, Lopez has again turned to his faith. But he no longer asks for miracles. Now, his prayers are only for his family. “I just ask God that whenever the day comes, he gives them strength. He gives them strength to persevere.”
For those left behind, however, perseverance is more than a matter of faith. Edwin tries to channel his fear and sadness into motivation for his studies, because it’s something tangible he can do to resist the deadly march of the disease. As his father often tells him, his education may be the only way to escape their family’s generational cycle of poverty, illness, and death. But it can be hard to concentrate when everything seems so precarious. Francisco, Edwin’s uncle, may soon begin dialysis too, and with each of the family’s income-earners falling ill, Edwin’s chances of avoiding the fields grows slimmer. And regardless of the physiological cause of CKDu, he understands the implications of fieldwork here, in this place. “Agriculture kills you,” he said. “That’s where the kidney disease comes from.”
UPDATE: A previous version of this story incorrectly cited the value of a National Institutes of Health grant to study CKDu. The grant was for $4 million, not $4 billion.
Note: Numerous interviews for this story were conducted originally in Spanish, and subsequently translated to English.
Fletcher Reveley is a freelance writer based in Tucson, Arizona.
Kitra Cahana is a freelance documentary photographer and videographer, and a contributing photographer for National Geographic Magazine.












Comments are automatically closed one year after article publication. Archived comments are below.
Is there any study about kidney decease within the Untied States’ Central American immigrant population? I’ve known a few cases of renal illness among relatively young immigrant men on Long Island, NY.
I am not a doctor, but like to follow these type of issues.
It will be good that you check the effects of drinking too many energy drinks.
In Honduras, we are seeing many cases of people working in the construction industry that are drinking many energy drinks per day and also eating instant noodles which are high in sodium or MSG.
I would volunteer to, find a cure for that.
that sickness is killed a lot of ppl I know
and I’m marked as well. before dying I would like to help find a cure…
for a kidney transplant there is no money plus not enough kidneys for the many reciepients…
Why are none of these end-stage kidney patients being considered for kidney transplant? Is it because they lack the financial resources necessary to consider transplant as a possible solution?
I have first time, experience with the desease, an agricultural drinks water from the creek, same place where the pumpif filled up with residue of the chemical already everywhere, in the sugar cane field whateever chemical is used on it, as the worker sweats dyhidration sets in. NO bathrooms available so you avoid drinking water, as a worker you get up 3am
and tried to finish your labor before the sun burns you alive.. the contaminated waters untreated for human consumption and the chemicals used in the fields plus the gruelling working cond add up..the sickness might be gotten..
I am so thankfull for UNDARKandto the freelance article writer for putting this
article so the world can learn about this silent killer..
keep the focus on this deasease El Salvador thanks you and look forward to more on this topic
We drown in an ocean of chemicals and have them introduced to our bodies, through medications and vaccinations. These synthetic chemicals must affect the kidneys because humans have never evolved to deal with them. Never before have humans had to face such a toxic onslaught from vaccinations in particular, but also from medications and from agriculture and industry.
You sound like an anti-vaxxer. We are exposed to more chemicals in our daily lives from foods – both plant and meats – then from medicines and vaccinations