Robert Suttle’s nightmare began in May 2008 when detectives from the Shreveport Police Department approached him at his job at the Louisiana Second Circuit Court of Appeals. Within a year, he was charged, convicted, sentenced to a six-month jail term, and forced to register as a sex offender under Louisiana’s broadly-written “intentional exposure to AIDS virus” law.
Suttle, who learned that he was living with HIV in October 2003, had ended a “casual but contentious” relationship with a man who later claimed Suttle had not properly disclosed his status. There was no evidence the man had actually contracted HIV. But Louisiana’s law, which is punishable by up to 10 years in prison, requires only “exposure” — not transmission or acquisition — to the human immunodeficiency virus.
“My driver’s license was stamped ‘sex offender’ in red letters. It was stigmatizing and embarrassing,” Suttle explained to me in a phone call in July from New York City, where he now lives and works as assistant director of the SERO Project, a national advocacy organization working to repeal HIV criminalization laws. “There is already so much stigma around living with HIV. This is the reality that many others are going through today.”
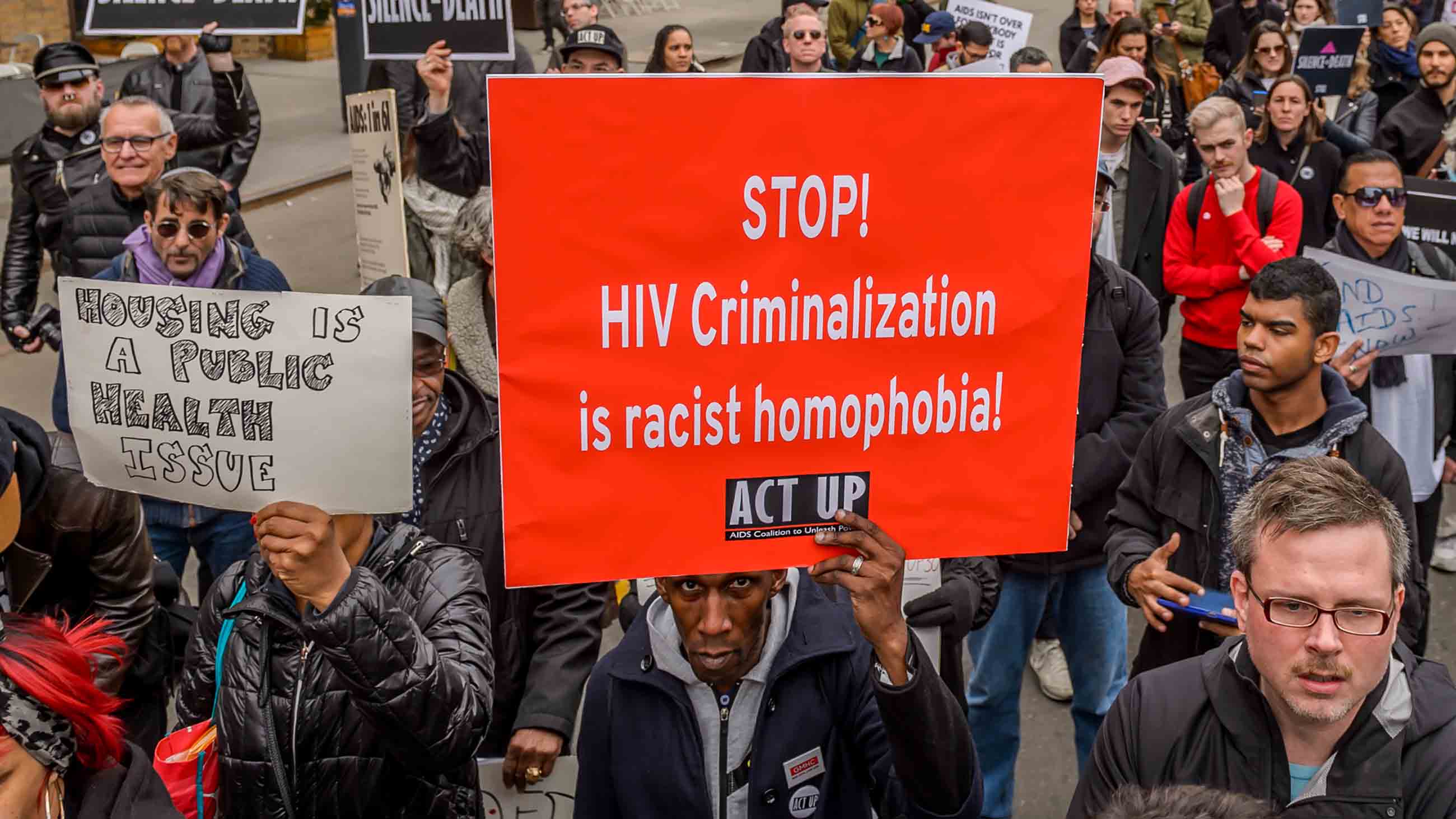
In part because of the work of the SERO Project and other advocacy organizations, these laws are beginning to face new scrutiny in states across the country. Some, like California, are already moving to decriminalize exposure to or transmission of HIV.
The scope of the problem is vast. As of March 2017, at least 31 states had laws in place that make it a crime to potentially expose others to HIV without disclosure of status, according to the Centers for Disease Control and Prevention. Some states will prosecute regardless of whether a condom is used. As Jessica Wapner reported in detail for Undark last August, most of these laws specifically target HIV and not other serious communicable diseases.
Many were enacted during the height of the epidemic in the 1980s and early 1990s — long before the science of transmission was fully understood, and before the introduction of precious, life-saving antiretroviral therapies. These new treatments have made living with HIV a chronic but manageable condition similar to asthma or diabetes. “The science has changed but the laws have not,” says Trevor Hoppe, an assistant professor of sociology at the State University of New York at Albany and author of the forthcoming “Punishing Disease,” which traces the history of the punitive response to the HIV epidemic. The book, published by the University of California Press, is scheduled for release in November.
Modern antiretroviral therapy slows down the HIV replication process and suppresses the virus to the point that it becomes undetectable. Studies have shown that once someone living with HIV has achieved viral suppression, it becomes extremely unlikely if not impossible for them to transmit HIV to a sexual partner. This strategy, known as “treatment as prevention,” has become one of the cornerstones of global HIV prevention programs. Criminalization laws do not take this into account.
A growing body of research has also revealed the degree to which HIV criminalization laws have disproportionately targeted women and people of color. In the 1980s, almost a dozen states outlawed HIV exposure or the failure to disclose one’s HIV status as part of the era’s larger “tough on crime” initiatives, according to Hoppe’s research. New Jersey became the first state to pass an HIV criminalization bill in 1985, and others quickly followed. “HIV was very scary, because it was largely terminal and untreatable at that time,” says Hoppe. “It was swept into this broader impulse to punish.”
Hoppe’s doctoral research found that black heterosexual men are disproportionately convicted under Michigan’s HIV disclosure law. Black men also receive longer and harsher prison sentences in at least four states, according to a pioneering racial and demographic analysis of HIV-specific convictions.
At the AIDS 2016 conference in Durban, South Africa, Hoppe gave a presentation about a study examining the racial and gender disparities of HIV-specific criminal laws in five U.S. states: Arkansas, Florida, Michigan, Missouri, and Tennessee. In those five states, “307 cases were sentenced to incarceration in jail or prison while 50 were sentenced to probation,” he explained at the conference. “The average incarceration sentence was nearly seven years.” Black men were sentenced to incarceration terms that were about three years longer on average in at least four of the states, according to Hoppe’s research.
The overall average prison sentence for black men convicted under HIV criminalization was slightly more than nine years. The average sentence for white men was slightly more than six years. The greatest racial disparity was found to be in Arkansas, where the average prison term for black men convicted under the state’s HIV criminalization law is now more than 23 years, twice the average sentence for white men, which is 11.6 years.
Women and people of color are disproportionately affected by California’s HIV criminalization laws as well, according to new research by The Williams Institute, a think tank at UCLA School of Law. Forty-three percent of people criminalized under the state’s HIV laws are women, even though women make up only 13 percent of people living with HIV across the state. And while 51 percent of those living with HIV in California are black or Latino, they comprise 67 percent of those punished.
California’s laws make HIV exposure and non-disclosure a felony punishable by up to eight years in prison. “HIV is the only medical condition that can result in a felony conviction” in the state, according to Lambda Legal, a civil rights and legal advocacy group. “And individuals with HIV can be subject to a longer potential sentence than for certain types of manslaughter.”
The racial disparities in prosecutions, while mirroring the racialized history of prosecutions and mass incarceration in the United States, are also exacerbated by the demographics of the epidemic. Overall, African-Americans represent about 13 percent of the nation’s population but account for nearly half — some 45 percent — of all new HIV infections. New infections have been increasing fastest among black men who have sex with men, who are also less likely to be in treatment or achieve viral suppression, according to the CDC. They also face structural barriers that impede access to health care, including higher rates of unemployment and higher concentrations across the South, which has poor health care infrastructure.
As it stands, California is home to the largest number of people living with HIV. About 137,000 people were living with HIV in the state in 2015, and that number grows by about 4,700 people every year. California is only outpaced by Florida in the annual number of new infections.
That’s partly why advocates are now hoping to push for reform of HIV laws in California — a bellwether state where laws on everything from auto emissions and public smoking to bike helmets and renewable energy standards have helped drive change in the rest of the nation. Public health analysts and anti-criminalization advocates, who have lobbied for reform successfully in a few other states, are hopeful that efforts to modernize California’s HIV criminalization statutes will soon tip the scales toward reform nationwide.
In June 2014, Iowa became the first state to reform its HIV criminalization statute — which mandated up to 25 years in prison for any exposure to the virus and was once described as “one of the most draconian laws in the country.” The change came after an intense, five-year campaign by national groups like the SERO Project, the Center for HIV Law and Policy, and Lambda Legal, which worked alongside local advocates, legislators, and public health officials to raise awareness of modern HIV science and antiretroviral therapies among prosecutors, law enforcement, and legislators. The decision was also bipartisan: Iowa’s Republican Governor Terry Branstad signed the decriminalization bill three summers ago — 16 years after he signed the original, harsher bill as a first-term governor.
To be sure, not everyone thinks Iowa’s reforms go far enough, but a series of national and regional conferences focused on repealing HIV criminalization laws followed quickly on the heels of the state’s decision, and Colorado became the second state to modernize its HIV criminalization policies two years later, in 2016.
Thanks to these efforts, legislators in California are now poised to modernize that state’s HIV criminalization law. In February, State Senator Scott Wiener introduced legislation that would repeal the felony provisions and make deliberate intent to expose — which very rarely happens, according to most public health and policy experts — a simple misdemeanor. The new legislation would incorporate the current science concerning the disease, and it notes that using a condom or receiving treatment indicates a lack of intent to transmit HIV. The legislation passed the California Senate at the end of May by a 26-to-13 vote and is now making its way through the Assembly.
Legislators in Florida have also expressed interest in reviewing that state’s HIV criminalization statutes, and similar reconsideration efforts are underway in Georgia, Idaho, Mississippi, Missouri, and Ohio. The Ohio Supreme Court is also considering the constitutionality of that state’s laws, which mandate disclosure of a “positive” HIV status. The court heard oral arguments in May and is expected to rule soon.
Advocates welcome the drift toward reform, but they emphasize that change comes slowly — and far too slowly for those who are still being convicted or are currently serving absurdly long prison sentences based largely on fear and ignorance, rather than dispassionate research and understanding.
“The problem is most people don’t know the science,” said the SERO Project’s Robert Suttle. “Criminal reform is just a slow-moving process. So many moving parts. But I’m very proud of what we have accomplished so far.”
Rod McCullom reports on the intersection of science, medicine, race, sexuality, and poverty. He has written for The Atlantic, The Nation, and Scientific American, among other publications.










Comments are automatically closed one year after article publication. Archived comments are below.
Great advocating
I think the laws should stand. If people are consenting there should be no problem and they should be in a trusting relationship. TO NOT disclose could still place a person in harms way regardless of precautions made. Systems fail, Viruses mutate. If they have nothing to fear then why not tell the person you intend to be intimate with the truth? Again TRUTH. A very simple word, the laws were established because people were not being honest or telling the truth. The little matter seems to have been left out of the discussion. No, you change the laws people will come in contact with HIV that would not have if disclosure were required and done. What about the rights of the person having sex with someone with HIV? Where are their rights? Again, one sided article, the author already knew where they wanted to take the discussion before they started to write it,
But why only HIV should be persecuted? there are other STDs that cannot be cured and impair the quality of life (hepatitis C) but there is no law persecuting non-disclosure of this disease. HIV is exclusively targeted and the question is, whether it is still necessary, considering current treatment options.
“TO NOT disclose could still place a person in harms way regardless of precautions made.”
This is completely false. If you take precautions (be on effective treatment, condom use, or both), you will not put anyone in harm’s way.
“Systems fail, Viruses mutate.”
If you are on effective ART, your virus is very unlikely to mutate because the viral replication process is kept in check. In the rare instance it does mutate, however, current medications have strong genetic barriers that are able to keep the new strains under control.
“If they have nothing to fear then why not tell the person you intend to be intimate with the truth?”
Unfortunately, stigma and discrimination based on someone’s HIV status are real and some people DO have many things to fear about disclosing. We’re not necessarily talking about fear of rejection, but fear of being socially ostracized, losing a job, etc. This is confidential medical information for a reason. I agree with you, however, that you deserve to know the truth if you directly ask the person about his/her status.
“the laws were established because people were not being honest or telling the truth.”
Absolutely false. Laws were established in the 80s and 90s because, at the time, HIV/AIDS was a death sentence and the science regarding transmission was not well understood. Now we know that being virally suppressed means effectively zero risk of transmission.
“What about the rights of the person having sex with someone with HIV? Where are their rights?”
Fair point. But if you’re going to have sex with anybody, regardless of HIV status, then you should ask and have a right to obtain a truthful response (we probably agree on that). But to give the full weight of the responsibility to the HIV+ person to disclose and take precautions for you, that is simply absurd. People who engage in sex have shared responsibility for their actions. If you rely on other people’s words to make decisions regarding your own sexual health and behavior, then you’re certainly more likely to contract either HIV or any other STI.
A very thoughtful examination of an issue that touches the lives of many of us, either directly or indirectly, but never knew it was this systemic. Rod McCullom gives it a name and a face! Well-written and researched. Bravo