Modern industrial robots are masterpieces of engineering that move with marvelous speed and precision. As one example, the popular Epson industrial robots complete their tasks in one-third of a second, and have a repeatability — the ability to return to the same position over and over — of just five microns, or one-fifteenth the thickness of a human hair. This incredible level of precision was not one of the early selling points of robots, but it has emerged as a major advantage, and one that has been applied in surprising ways.
The accompanying article is excerpted and lightly edited from “The Heart and the Chip: Our Bright Future With Robots,” by Daniela Rus and Gregory Mone. (W.W. Norton, 260 pages.)
When I was working toward my Ph.D., writing algorithms capable of guiding and controlling a robotic gripper, the best mechanical hand in the world had been built by my friend, engineer and inventor Ken Salisbury. He’d already been in the robotic hand business for decades at that point; he built a robotic finger when he was just 6 years old.
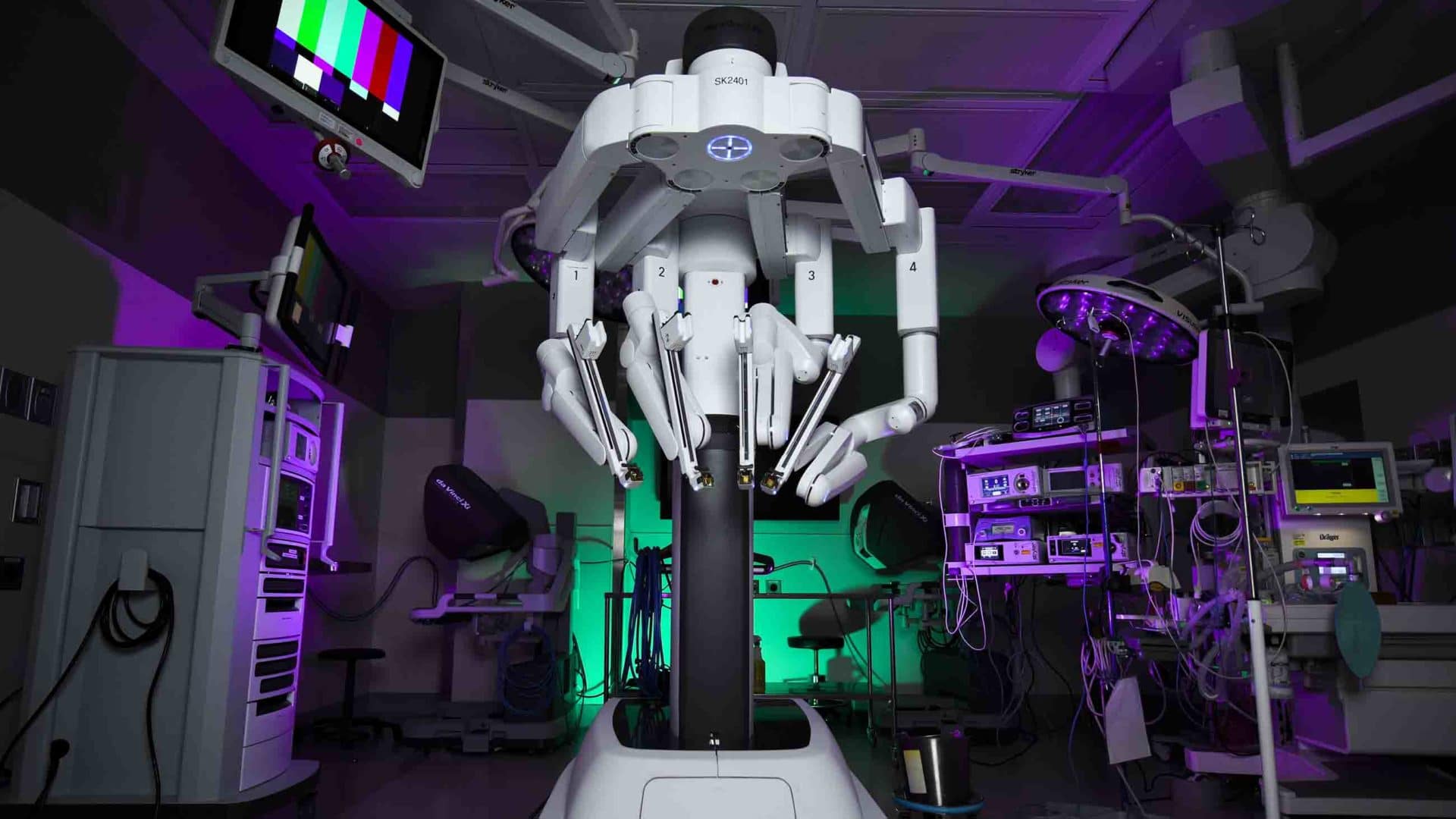
Over the years, Ken and his students developed a number of pioneering robotic hands and helped found the field of haptics. In the mid-1990s, an old friend asked Ken to travel to California to talk to a newly formed company about his work. Soon thereafter, Ken started working on some of the key systems for the da Vinci surgical robot, which is today one of the most successful robots in the world.
The da Vinci is a fantastic example of how the heart and the chip can work together to achieve a higher order of success. Despite what we see in the movies, intelligent machines cannot perform surgeries alone.
At the end of the film “Star Wars: Episode III – Revenge of the Sith,” the burned and mutilated character Anakin Skywalker is deftly operated on by a suite of robots. But this level of autonomy is not achievable yet — and even if we did somehow reach that point, we should not leave something as important as surgery to an autonomous machine.
Instead, what we’re seeing now with the da Vinci and other systems are highly trained, immensely capable human surgeons utilizing robots as another tool that helps them do their job with higher precision and smaller incisions.
One of the surgeons I spoke with about the role of robots in his field sees them as being most useful as extensions of human beings in complex, high-stakes surgical procedures. Yet he told me that robots are also tremendously helpful with low-risk, high-volume procedures, as they allow surgeons to work more efficiently and with a lower volume of error.
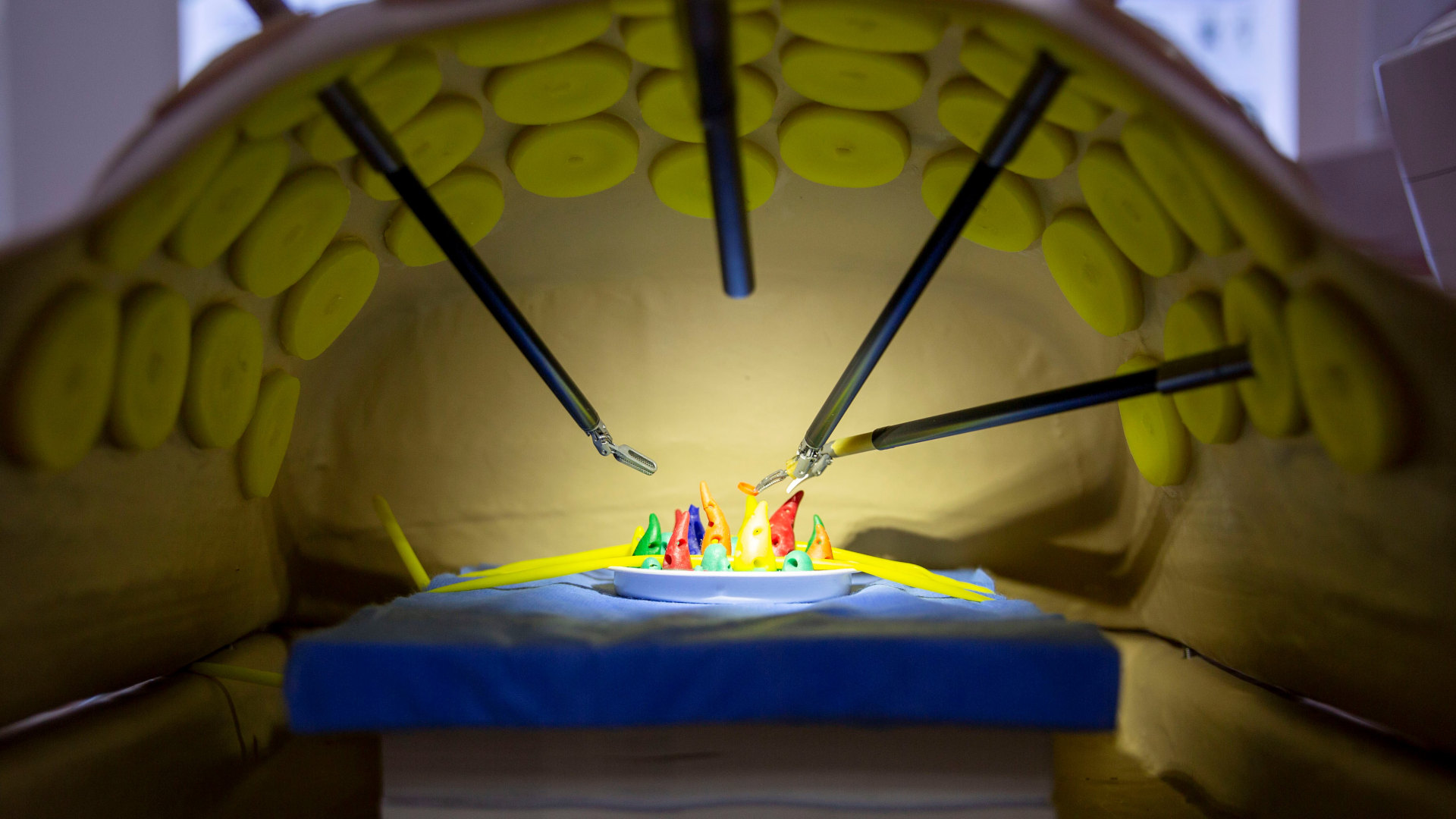
A surgeon using a da Vinci robot sits at a console inside the operating room near the patient. The surgical apparatus, which typically consists of a base and four robotic arms, hovers over the patient, and the surgeon at the console operates two handheld grippers that manipulate the different instruments on the ends of the robotic arms. A pair of forceps, for example. A tiny endoscope relays a three-dimensional, high- resolution view of the site, allowing the surgeon to see the spot up close, at 10 times magnification — a means of extending the surgeon’s vision to the very small.
What we’re seeing now with the da Vinci and other systems are highly trained, immensely capable human surgeons utilizing robots as another tool that helps them do their job with higher precision and smaller incisions.
The system is designed to let surgeons view the tools they’re manipulating in real time, as if the tools are right below their physical eyes and held in their own hands. And the tools themselves are designed for precision. The surgeon has to move one of the handheld manipulators 10 centimeters for the tool to move a single centimeter, and the system filters out any tremors in the surgeon’s hands.
Another popular robotic surgery system, the Mazor X Stealth Edition, is ideal for the kind of high-stakes procedure my surgeon friend described. This robot is particularly good at assisting with a type of scoliosis surgery. A dozen screws are placed along a patient’s spine, inserted into different vertebrae. These screws are then connected by a metal rod, which helps to straighten out the patient’s back.
Surgeons have been performing this operation successfully by hand for a long time. Yet it remains a high-risk endeavor; if one of the screws is misplaced and hits the spinal cord, the patient could be paralyzed. Precision is essential, and spinal surgeons have willingly accepted this robot as an assistant capable of reducing the associated risk.
Prior to the operation, the surgeon plans the placement of each screw with the help of CT scans and 3D visualization software. The AI-powered robot suggests a particular alignment, and the surgeon adjusts this as they see fit, applying their superior human knowledge and judgment. Once the surgeon has designed and planned out the surgery, choosing the placement of each screw, the robot carries out the procedure, inserting each screw exactly as planned.
Human expertise sets the scenario. Then robotic precision throws the bullseyes.
Precision is essential, and spinal surgeons have willingly accepted this robot as an assistant capable of reducing the associated risk.
This idea of enhanced precision through robotic surgery could be extended to new and more science-fiction-like domains. In my lab, for example, we’ve experimented with miniature robots that could be swallowed like vitamins, travel to the site of an infection or internal wound, administer treatment at the site, then slip out through the digestive system. We made these robots partially out of sausage casing, so they’d be biodegradable.
To test the concept, we needed a target application, and one of my students suggested we address an odd but increasingly common problem reported by the National Poison Data System. Each year in the United States, more than 3,500 people swallow tiny button batteries. The number is on the rise and, not surprisingly, most of the cases involve children. Removing the battery often requires surgery.
Imagine a young child has just swallowed a battery. Within an hour, it may begin to pierce the stomach tissue. Removing it through the standard surgical procedure would be highly invasive and thereby increase the risk of pain and infection. Now picture a small, digestible robot packaged into an ice capsule small enough for the child to swallow. Once inside the stomach, the ice melts and the robot unfolds itself like origami.
By manipulating external magnetic fields, the surgeon steers the robot pill, which includes a magnet of its own, across the stomach wall to the precise site of the wound.
In this way, the robot allows the surgeon to reach into the child’s stomach without making a single incision. Using its tiny magnet, the robot grabs the battery, then exits the body naturally. The surgeon can then guide a second robot pill to the location of the wound to deliver targeted, on-site medication. In our experiments, this second robot had an accordion-like shape, and as we steered it forward with our external magnetic field, the robot folded and unfolded its body, walking across the artificial stomach lining like an inchworm.
Once it arrived at the target site, the robot spread itself out and covered the wound. In a real medical scenario, this folding bot would be laden with medicine designed to prevent infection. The robot itself, made from biodegradable materials, would break down over time, and the tiny magnet we used to steer and control it would pass out through the digestive system. No incision would be necessary. The drug would go precisely to the site of infection. And the child would be able to go home the same day.
Today, this robot exists only as a lab prototype. But in five years or 10, there’s no telling where we would be able to reach with this sort of robot, and the potential impact of such technologies.
One of the complexities involved with robot-assisted surgery is that a human being is a living, breathing, changing organism, not an industrial part. Our bodies don’t remain perfectly static. So, with the spinal surgery robot, the system has to continuously track the precise position of the patient, his or her spine, and its own robotic components to ensure accuracy.
Among other things, this requires technology to ensure that the person remains precisely fixed relative to the robot, which is similar to something we’re working on in my lab. In this project, though, we’re looking at improving cancer treatment.
The conventional way to treat cancer with radiation relies on X-rays. While traditional radiation therapy can be very effective against tumors, it also harms the neighboring healthy tissue, leading to side effects. One of the alternatives to this approach is proton therapy, which shoots narrow beams of high-energy particles directly at cancerous cells, thereby limiting the collateral damage.
Unfortunately, generating the beams requires a particle accelerator and a 100-ton gantry that rotates around the patient to precisely steer the stream of protons. The equipment can take up a small building and cost as much as $100 million. As a result, there aren’t many proton therapy treatment centers in the world, which is terribly unfortunate: Although only around 1 percent of cancer patients receive the treatment, as many as 50 percent would benefit.
Thomas Bortfeld and Susu Yan at Massachusetts General Hospital asked me if we could redesign the system. Could we use robots and AI to find a way to extend the treatment to more people? The largest and most expensive piece of the proton therapy system is the gantry, which steers the beam precisely enough to strike the target tumor. What if, we wondered, instead of steering the beam, we kept the beam static? What if we moved the patient instead?
Robotic couches have been tested for traditional radiation therapy. What we suggested would be the first such system with the level of real-time tracking and adaptability required for proton therapy in particular. Our proposed system consisted of two parts. A soft robotic exoskeleton would wrap around the waist, shoulders, and upper arms of the patient, to keep them immobilized in a precise body position.
Robots, despite their capabilities, are not magic.
This soft immobilization system is in turn attached to a robotic chair normally used for flight simulators. We adapted this commercially available chair into a precise patient positioner, linking it to a vision system that tracks the patient relative to the beam. This way, if the patient does move slightly, despite the efforts of the soft immobilizing robot, the chair can make the necessary adjustments and ensure that the proton beam continues to hit the right spot.
In our early tests, the system was able to rapidly respond to a patient’s change in position — from slouching, for example — and readjust to within one millimeter of accuracy. This is the precision required for a clinical setting.
How else could we put precision robots to work in our world? There are many wild ideas and applications underway in robotics labs around the world and undoubtedly many more incubating in the minds of young inventors. The advances in robotics and AI over the past decade have been tremendous.
Yet robots, despite their capabilities, are not magic. We do not wave our wands like the sorcerer’s apprentice and instantly endow our clothes, vehicles, and household items with magical capabilities. No — we have to build them, often from scratch. We have to design, construct, assemble, and test their bodies and their brains, and ensure that the two are working together efficiently in the service of humans.
Daniela Rus is a roboticist, the first female director of MIT’s Computer Science and Artificial Intelligence Laboratory, and a MacArthur Fellow. Gregory Mone is the coauthor of four New York Times bestsellers.










You are incorrect when you state “Despite what we see in the movies, intelligent machines cannot perform surgeries alone.”
The first unassisted (AI/code only, no human intervention) appendectomy on a pig was performed over a decade ago at Johns Hopkins robotic surgery research lab. I imagine it has been repeated at other institutions by now as well.