The Lifesaving Potential of Less-Than-Perfect Donor Kidneys
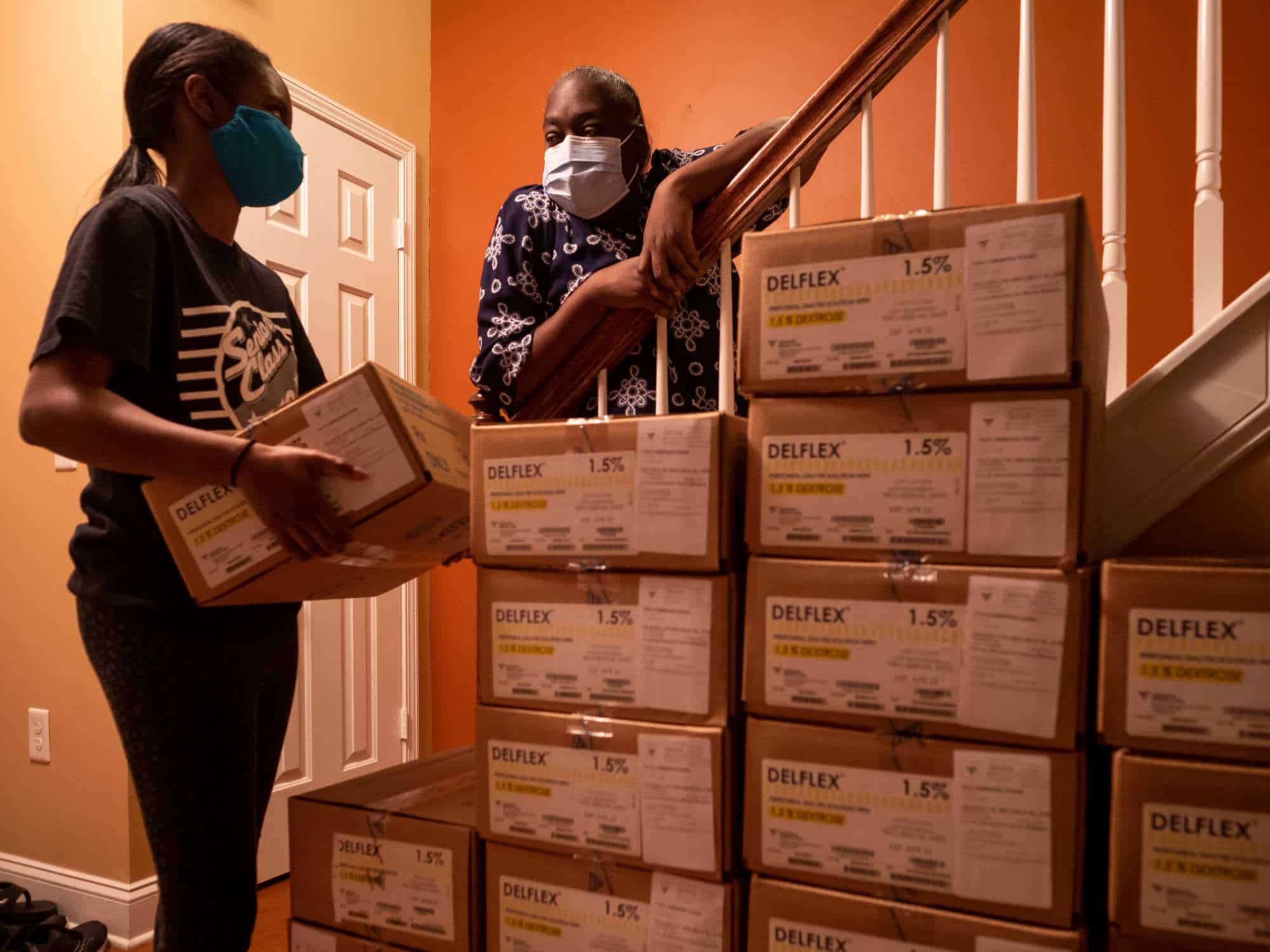
In 2017, Traci Evans-Simmons could no longer avoid dialysis for her failing kidneys. She had lived with a condition known as glomerulonephritis, which was destroying her renal function, since her diagnosis 16 years earlier. For the last three years, nearly every night, she has hooked herself up to machines that take the place of her functioning kidneys. It was always going to be a temporary solution. Eventually, her nephrologist had cautioned, Evans-Simmons would need a transplant to have the best quality of life.
“You cannot be on dialysis indefinitely,” she said.
PROFIT & LOSS: THE COMPLETE SERIES
Intro | The Market | The Conflicts | The Disparities | The Waiting | The Alternatives
So the 51-year-old resident of Charlotte, North Carolina sought access to a transplant waiting list — the first step for chronic kidney disease patients hopeful for a replacement organ. She was added to a transplant waiting list at Wake Forest University in the spring of 2019.
During a routine check-up at Wake Forest early this year to maintain her transplant eligibility, she learned that while she was steadily moving up the wait list as those above her got transplants — or died while waiting — she was still fairly low down on the roster. The team also told Evans-Simmons that her wait time was probably going to be longer because it was harder to find a match for her particular blood type. Her heart sank.
And then her team asked Evans-Simmons something she had never considered: Would she be willing to accept a kidney from a donor who had hepatitis C, a viral liver infection? The transplant coordinator said that the waiting list for organs from hepatitis C-infected donors was usually shorter — an appealing carrot to dangle for someone who had just learned she was likely to have an extended waiting period. Evans-Simmons had never heard of hepatitis C-positive kidneys — or what risks they posed. “Immediately I was like, no,” she said.

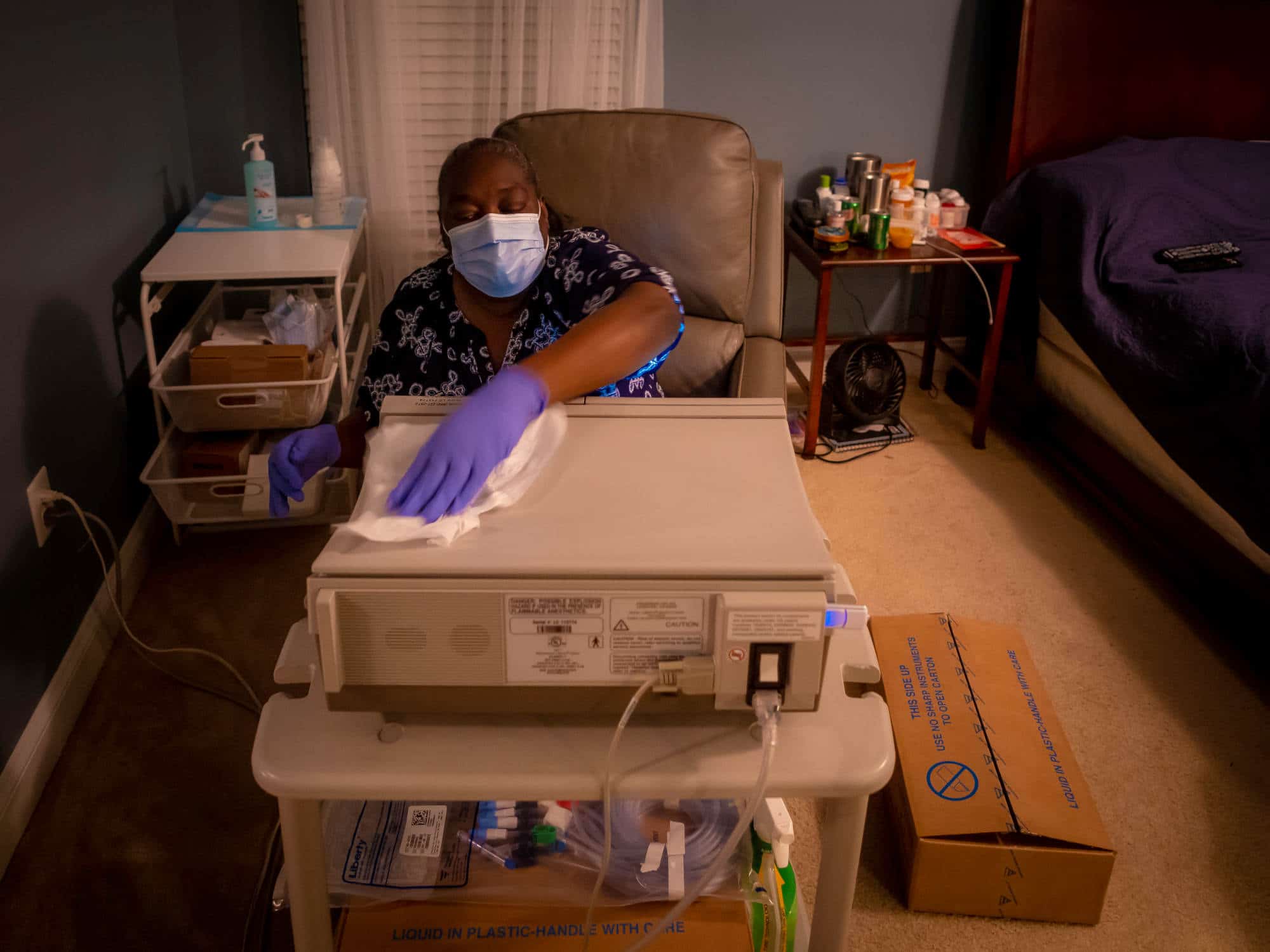
On the two-hour drive back to Charlotte, she called a family member, who immediately searched the internet and described to Evans-Simmons the information she had found. She also discussed the option with her husband. Evans-Simmons wanted a transplant, she said. But what she couldn’t decide was whether a hepatitis C-infected kidney was too steep of a cost.
Ever since Joseph Murray successfully transplanted the first kidney from one identical twin to another on Dec. 23, 1954, the need for organs has always outstripped supply. Even with modern medicine’s latest organ-preserving technologies, about 13 Americans die each day waiting for a kidney transplant.
Historically the backbone of the kidney donor system has been made up of young people who died suddenly — in a traffic accident, for example, or from a gunshot wound. Their organs are carefully screened for disease and, where an infection is found — or even where one is considered more likely, as with the organs of drug overdose victims — the organs are typically removed from consideration for the main transplant pipeline. Some studies have suggested that the U.S. discards a larger percentage of deceased-donor kidneys than in comparably developed countries like France.
Transplant surgeons like Jayme Locke at the University of Alabama at Birmingham have primarily worried about the transmission of a virus from the trifecta of bloodborne pathogens: HIV, hepatitis B, or hepatitis C. The latter created the greatest worry because it was most common. The Centers for Disease Control and Prevention estimates that in 2016, about 2.4 million Americans were living with hepatitis C.
The rise of the opioid epidemic, however, has forced a new reckoning. With the tragic increase in overdose deaths has come a similar rise in the supply of available donor organs — albeit from a demographic that doctors have traditionally shunned. But the arrival of better HIV and hepatitis C tests, along with a new generation of antiviral medications for hepatitis C that cure upwards of 95 percent of those infected, now has doctors like Locke — and patients like Evans-Simmons — considering kidneys that, only a few short years ago, would have never been on the table. “Every year, we throw away way more hepatitis C-positive organs than we use. So instead of throwing them away, could we actually put them in someone who could benefit?” Locke said.
In its acute stage, hepatitis C often causes no symptoms. But as it becomes chronic in more than half of people infected, hepatitis C can lead to cirrhosis — or scarring of the liver — cancer, and even death. Ironically, it can also cause kidney disease. And while the majority of cases are curable — and some people clear the virus from their bodies without treatment — at least 15,700 hepatitis C-related deaths were reported to the CDC in 2016.

Transplant surgeon Jayme Locke, shown here at the University of Alabama at Birmingham in a recent video call. “Every year, we throw away way more hepatitis C-positive organs than we use.” Locke said.
Even so, advocates say that the benefits of kidneys from hepatitis C-infected donors vastly outweigh the risks. Given the arrival of powerful new drugs for treating and controlling the viral infection, even a previously hepatitis C-negative recipient of a hepatitis C-positive kidney is far more likely to die waiting on dialysis than from the infected kidney. And that argument appears to be gaining currency: Data from the Organ Procurement and Transplantation Network (OPTN) — a public-private partnership overseen by the Department of Health and Human Services that connects health professionals involved in the U.S. transplant program — shows an increase in the number of hepatitis C-positive kidney donors each year from 2011 to the present.
But even with that increase, barriers to the use of these less-than-ideal kidneys persist — and not every expert has embraced their use. According to a survey published in the journal Kidney360 in November, only 58 percent of responding kidney transplant programs said they offer hepatitis C-positive organs to uninfected recipients.
David Roth, a nephrologist at the University of Miami, isn’t against the use of kidneys from hepatitis C-positive donors, per se, but he says he also worries that some of his patients’ desperation to get off dialysis may lead them to accept a less-than-stellar kidney. Many of his patients don’t have sophisticated medical backgrounds that make them familiar with the science, he says, which means it’s his responsibility to explain the risk in terms that they can understand.
“The decision-making process can be compromised,” Roth said. “In medicine, that’s very dangerous because then patients go down a road which they maybe can’t get out of. And that’s a real problem.” Nearly every person Evans-Simmons talked to had a different opinion on the subject. One relative told her, “I don’t think you should do it.” A physician in the medical office where she worked told Evans-Simmons to go for it. Opinions, she knew, were easy, but she was the one who would have to live with the outcome. Every option had major benefits — and serious drawbacks.
“The prospects of getting a kidney are exciting and scary at the same time,” she said. “While I am excited to not have to hook myself up every night, I am a little bit wary of, if I take this kidney, will I get hepatitis?”
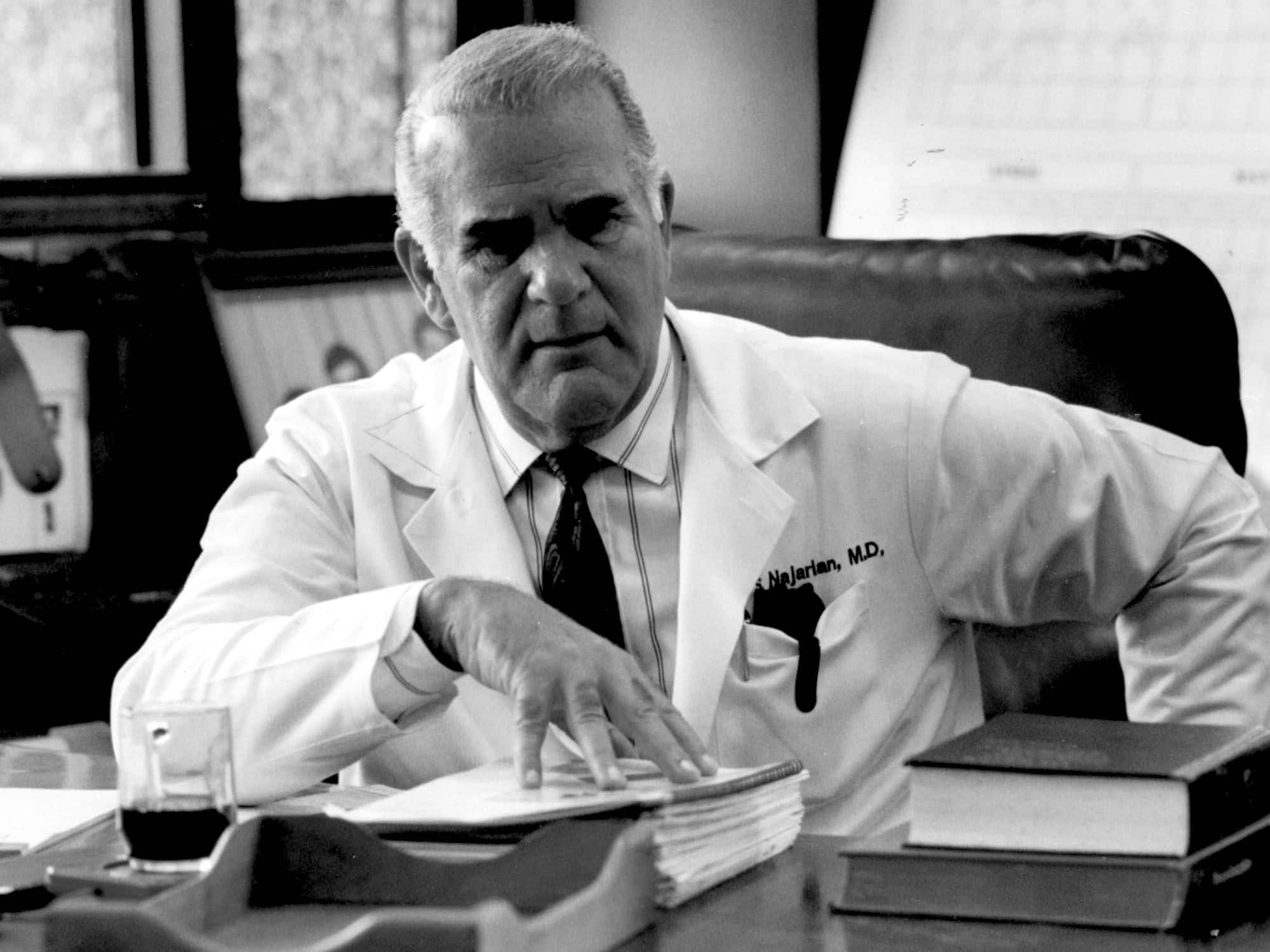
Alongside professional medical certificates and images of his family, portraits of Thomas Starzl and John Najarian, pioneers of American transplant surgery, peer down from the walls of Timothy Pruett’s office at the University of Minnesota. They remind him, he says, of how the field started back in the 1950s and 60s — a time when surgeons like Starzl and Najarian took incredible risks to find their patients a liver or a kidney that would potentially save their lives. Surgeons looking for a transplantable organ had standard but strict criteria about who ideal donors should be, and the classic example would be someone under the age of 35, with no chronic medical conditions, who had died in a car accident. This demographic, the thinking was, would have the healthiest organs, and the ones most likely to work well after the stress of transplant.
The problem, Pruett says, is that “very few people die that way in this country.” (The OPTN estimates that only three in 1,000 deaths allow for organ donation.) “Our standard-criteria donor,” Pruett said, “is not the standard death.”
About half of Americans are currently registered as organ donors, according to Donate Life America, a nonprofit organ donation advocacy group — many of them enlisted through a familiar check box selection during driver’s license renewal. But even that percentage is reduced by natural barriers — chief of which is the location of death. Because a potential donor’s organs need to be nourished with oxygen-rich blood to remain viable, it is typically only those would-be donors who die in a hospital, after all potential life-saving interventions have been tried and failed, who will even have their organs considered — and the bar is necessarily high. A transplant team will evaluate such a patient’s medical condition to ensure they are a candidate for organ donation and the cause of their death hasn’t harmed their organs. The evaluation process also tests for bloodborne diseases such as hepatitis B, hepatitis C, and HIV, as well as recent risky behaviors like injection drug use.

Visual: Lyn Alweis / The Denver Post via Getty Images
Visual: Judy Griesedieck / Star Tribune via Getty Images
If they are one of the rare individuals who is a candidate, the transplant team will discuss donation options with their family. If the deceased patient had authorized donation or if the patient’s next-of-kin consents to donation, an organ procurement organization can then provide information to the United Network of Organ Sharing (UNOS) — a private, non-profit organization that runs OPTN for the federal government — about the donor’s blood type and body size. UNOS’ computer algorithm then matches the organs to recipients based on blood and tissue type, body size, how desperately someone needs an organ, and how long they’ve been waiting.
If UNOS finds a potential match, they send an electronic message to the recipient’s transplant surgeon, who can accept or reject the organ. Should the surgeon decide against using the kidney (say, because the surgeon doesn’t believe it functions well enough for a patient), UNOS goes to the next match on the list and repeats the process until a surgeon accepts. If an organ is turned down outright, a patient may never know one was available. At the donor’s hospital, surgeons recover the organs, which are then infused with a special solution to remove blood, packed on ice, and transported to the recipient’s hospital. Once a kidney is closer to transplant, doctors can perform more tests to evaluate its function and may make a last-minute call that the organ isn’t suitable, even after the potential recipient has already checked into the hospital.
Even though physicians and advocates have worked hard to expand the donor pool since Starzl and Najarian began performing transplants 50 years ago, demand for organs far outstrips supply, and nowhere is that gap starker than in the world of kidney transplants. Nearly 750,000 Americans are living with end-stage renal disease (ESRD), meaning that their kidneys can no longer keep them alive on their own. Some of these individuals are too sick for a transplant or aren’t interested. But as of December 2020, nearly 92,000 Americans were on a list waiting for a kidney transplant. And while living donation — in which a family member or other living donor provides a kidney to an ailing recipient — has helped thousands of people get off dialysis, someone in the United States still dies every 110 minutes while waiting for a kidney that never comes.

Dr. Timothy Pruett in his office at the University of Minnesota in a recent video call. “Our standard-criteria donor,” Pruett said, “is not the standard death.”
With so many patients on the brink of death, surgeons have been pushing the boundaries for years. While nephrologists and transplant surgeons were — and continue to be — far more picky when choosing donor kidneys for children and young adults, for example, because those organs will need to function for far longer, they’ve come to realize that organs that fall short of the Starzl- and Najarian-era ideal can still provide older recipients with a decade of good-quality life. To provide transplant surgeons with a quantitative metric of a kidney’s quality, the Kidney Donor Profile Index (KDPI) was introduced in 2014. The index, based on transplant outcome data from UNOS’ tracking system, integrates information about the donor (their age, body mass index, ethnicity, kidney function, cause of death, and other health variables. The KDPI ranges from 0 percent to 100 percent, with 0 percent being the best possible quality organ. A KDPI score of 85 percent, on the other hand, means the organ has a risk of transplant failure greater than 85 percent of recovered kidneys.
Over time, better immunosuppressant medications have made it possible to expand the pool of potential matches without risking rejection. But a surge in opioid overdose deaths in the U.S., which began in the late 1990s, created an unprecedented supply of potential donor organs — and presented tough new questions for transplant doctors and would-be recipients. With most overdose deaths occurring in individuals aged 25 to 34, and with organs that were generally in good shape, most overdose victims would seem to make for ideal organ donors — with one small catch. People with a long history of injecting drugs often have a similarly long history of sharing with other users, exposing them to a variety of bloodborne infections. A global study from 2019 showed that about 40 percent of people who use injection drugs are currently infected with the hepatitis C virus.
Such metrics have long made the transplant community wary. The first generation of diagnostic tests used to detect hepatitis C infections, after all, relied on identifying antibodies the body produced in response to infection. But the CDC estimates it can take 8 to 11 weeks to produce enough antibodies to create a positive test result, meaning that someone could be infected with hepatitis C, but still have a false negative test result because they didn’t yet develop enough antibodies to the virus. The long lag between exposure and positive test results meant that someone who injects drugs several times each day could be exposed to the virus multiple times but still test negative, explained Christine Durand, an infectious diseases physician at Johns Hopkins University. As a result, the CDC classified an organ from anyone known to inject drugs for nonmedical reasons as being “high risk.”
A 1998 study by a group of French scientists showed just how dangerous accidental hepatitis C infection could be in kidney transplant recipients. The researchers, from Hôpital Necker in Paris, followed 499 patients who received a kidney between 1979 and 1994. Tests of the patients’ blood for hepatitis C antibodies from the time of transplant revealed that 22 percent were already infected. Their analysis revealed that these patients had 2.8 times the odds of dying during the study follow-up period, largely due to liver failure and sepsis. Early research from the U.S. showed that the results weren’t better when they evaluated transplanting kidneys from hepatitis C-positive individuals into older adults who tested negative. According to the 2011 study, seven of 13 elderly individuals who received kidneys from hepatitis C-positive donors between 2003 and 2009 developed positive hepatitis C viral loads, and only six had survived a year and a half after transplant, compared to 85 percent of similarly-aged adults who received a kidney from an uninfected donor.
But newer hepatitis C diagnostic tests that could detect the virus at very low levels have greatly reduced the latency period from about six months to one or two weeks, and the potential for inadvertently infecting someone with hepatitis C via a transplant that was considered nominally disease-free has also dropped. The chances that someone would be infected with the hepatitis C virus after a false negative test is now about 1 in 1,000, according to the OPTN. It is roughly the same for HIV.
“You have more of a likelihood of being hit by lightning than getting an infection from an increased risk donor,” said Durand. Still, the OPTN notes that unexpected transmissions from donor organs have increased in recent years and recommends that health care providers view negative tests cautiously.
Recognizing the improvements in hepatitis C treatment in transplant, the U.S. Public Health Service, which issues guidelines under the U.S. Department of Health and Human Services for assessing organs and mitigating disease transmission in the OPTN began using the term “increased risk” donor organ in place of “high risk” in 2013. The term was used for any organ that came from someone who tested negative for hepatitis C and other diseases, but met one or more risk factor criteria, including having injected drugs for nonmedical reasons within the past 12 months. The idea was to make the label more accurate and less stigmatizing, but the change did not do much to inspire confidence — nor change. “Just putting that label on will reduce — will decrease people’s likelihood of accepting that organ,” Durand said.
The reluctance doesn’t just come from patients. Indeed, physicians themselves have sometimes been hesitant to use increased risk donor organs because they, too, can overestimate the risk of infection. Passing over a potentially risky organ, however, reduces that risk.
Across the ocean, however, HIV has forced a re-calibrated view.
As a practicing physician in South Africa, Elmi Muller understands how the virus could ravage the body. While rates are coming down, some 13 percent of the country’s populace is infected with HIV, and as a kidney disease specialist, many of Muller’s patients have had HIV-associated kidney disease. HIV in their bodies directly attacks the kidneys, causing sudden, irreversible renal failure. Their only hope of survival is dialysis and transplant. In 2001, when Muller started practicing in Cape Town, South Africa had only a handful of dialysis centers to treat its population of roughly 50 million. Dialysis was reserved only for patients who were likely to receive transplants, she said. Although newer antiretroviral medications had turned AIDS, the most advanced stage of HIV, from a death sentence into a chronic condition in the U.S. and Europe, the medications remained out of reach much longer in South Africa. As a result, anyone with HIV was de facto ineligible for dialysis — even after the antiretrovirals became available in the country in 2004.
To Muller, this was a travesty. “I felt that HIV patients were generally quite young, they were economically active people, and they often had some young families. And it felt to me like our criteria for dialysis, excluding them was a problem,” she said.
Not only did Muller have to watch her own HIV-positive kidney failure patients succumb to a potentially treatable condition, she also saw otherwise healthy kidneys from HIV-positive donors discarded. To Muller, the solution was obvious: Transplant HIV-positive kidneys into the HIV-positive patients who needed them.
In 2008, Muller performed just such a transplant. Then, about a month later, she performed another. The surgeries were a resounding success, but before Muller could relish her victory, she had to face the very real blowback from her superiors, who viewed her work as being a waste of limited health resources. “The reaction locally was quite negative,” Muller said. The support of her boss, Del Kahn, along with that of a few locals and many international physicians, saved her job and career.
But Muller’s use of “compromised” organs in transplants nonetheless reverberated around the globe. Follow-up studies published in the New England Journal of Medicine showed that Muller’s HIV-positive transplant recipients fared just as well as their uninfected counterparts, raising the question of whether the same might be true for transplants involving hepatitis C infections.
Just as Muller’s HIV work was being published, a new hepatitis C treatment known as direct-acting antivirals hit the market. Compared to the existing therapy, which made use of immune stimulants called interferons, the new medications were more effective at suppressing viral replication and had fewer side effects. For the first time, said Niraj Desai, surgical director for kidney and pancreas transplants and an assistant professor of surgery at Johns Hopkins Medicine, physicians treating people with hepatitis C could talk about a cure. The key question, though, was whether the drugs would be effective in kidney transplant recipients.
It would be unethical to transplant a kidney from a hepatitis C-positive donor into a hepatitis C-negative patient without knowing if the drugs would work, so researchers started by enrolling a small group of kidney transplant recipients who were hepatitis C-positive before their transplant in a controlled study. They found that the drugs worked just as well at suppressing the disease in transplant patients as they did in healthy adults. “The next step,” Durand said, “was saying ‘Well, what about actually intentionally doing a transplant where you knew there was going to be an expected transmission?’”

Visual: Lerato Maduna

Visual: Lerato Maduna

Visual: Lerato Maduna
Several trials, including one at the University of Pennsylvania and another at Johns Hopkins, asked a handful of patients to do just that. Both trials provided 12 weeks of direct-acting antivirals to the patients at no cost. The UPenn trial began treatment with the drugs after confirming hepatitis C transmission post-surgery, whereas the Johns Hopkins participants took their first dose immediately before. Even with all the potential risks spelled out, both trials had no problems finding participants. One year post-transplant, none of the patients in the UPenn and Johns Hopkins studies had developed any signs and symptoms of hepatitis C. Some never even showed any signs of hepatitis C viral RNA in their blood — a sign of just how effective the medications were at suppressing viral replication, says Desai, who co-led the Hopkins trial with Durand.
“We had really good success — 100 percent success rates,” Desai said. He had good reason to believe that the drugs would work as he had hoped, but “the proof is when you have the data,” he said.
Studies following patients who received hepatitis C-positive kidneys but were not part of clinical trials were nearly as good. A major difference, says Meghan Sise of Massachusetts General Hospital, was that for some patients, their insurance companies would only approve the expensive medications after the individual had formally tested positive for hepatitis C, despite the fact that transplant is virtually guaranteed to transmit the virus. Although the patients had transient signs of liver dysfunction, all finally cleared their infection. In one study first published online in August, patients’ new kidneys also remained healthy six months later.
“The risk of dying while on the waiting list is actually higher than the risk of dying from one of these transmitted infections,” said Michael Ison, a transplant infectious diseases physician at Northwestern University. “By limiting the use of these organs, we could actually be harming the patients.”
Infectious disease transplant physician Daniel Kaul at the University of Michigan says he watched these trials with interest. The results were clear that newer antivirals made transplanting less than perfect organs a viable option — far safer than remaining on dialysis. Convincing patients, however, is a different story.
Indeed, where Kaul saw benefit, some patients saw risk. The threats of dialysis were familiar — many of those on the transplant list had been navigating them for years. A potentially fatal infection, especially one with decades of stigma attached to it, however, was a total unknown. As a result, hundreds of perfectly good organs labeled “increased risk” were discarded each year, according to a study Kaul and colleagues published in 2017 in the journal Transplantation. From a patient perspective, it’s not hard to see why “increased risk” might be problematic, Kaul says. The term may make it seem like someone stands a 10 or 20 percent chance of getting hepatitis C from a transplant when, in reality, it’s more like 1 in 1,000 — or 0.1 percent odds.
“It’s far lower than the risk of organ failure, and in fact, it’s probably about the same as the risk of getting hepatitis C if you stay on dialysis for an extra year or two,” Kaul said. “So you’re not really lowering your risk of getting hepatitis C by saying no to that increased risk organ, but you’re increasing your risk of death and never getting a transplant.”
This is one of the reasons, says David Klassen, the chief medical officer at UNOS, that the U.S. Public Health Service and OPTN are moving away from calling these organs “increased risk.” This year, the Public Health Service released new guidelines that include a recommendation from an advisory committee to eliminate the “increased risk donor” terminology, which OPTN plans to implement in March. The guidelines, according to a statement provided to Undark by Sridhar V. Basavaraju, director of CDC’s Office of Blood, Organ, and Other Tissue Safety, recommended that no specific term be used to describe donors with risk factors. Instead, the statement noted, “the organ procurement organizations should ascertain donor risk factors if they occur within the 30 days prior to organ donation (for example, if someone was an IV drug user within 30 days prior to organ donation) and convey this information to transplant centers. The transplant centers should, as part of standard informed consent, explain this information to transplant recipients.”
Klassen says the old term is a relic of the days before the KDPI, when organs were considered either “increased risk” or not in a binary paradigm rather than in a spectrum of potential risk. An organ from virtually any donor has the potential to transmit hepatitis C if someone has been infected in the days before death, Klassen noted. And whether a donor kidney is known to be hepatitis C-positive or not, the arrival of direct-acting antivirals has greatly minimized the risk from the hepatitis C virus, further rendering the term obsolete.
But for individuals like Evans-Simmons, the issue is not one of terminology; she was offered a kidney from a donor known to be infected with hepatitis C. In a Facebook transplant support group, Evans-Simmons read the story of one poster who said he accepted an organ from a hepatitis C-positive donor and subsequently tested positive himself before being cured by a course of direct acting antivirals.
“While I felt, OK, believe there is a cure, at the same time, I don’t want to deal with hepatitis on top of recovering from major surgery and all the stuff that comes with the medications you have to take,” she said.
Torn, Evans-Simmons came across a newspaper article profiling Sharon Price, a 74-year-old retiree who had received the first hepatitis C-positive donor kidney at Atrium Health, Charlotte’s largest health system, in 2019. Price had grandchildren and was doing well, Evans-Simmons recalled. Accepting that kidney meant that Price was able to receive a transplant before he ever had to begin dialysis. He started on hepatitis C antiviral medication immediately after transplant, and to date has had no side effects from the treatment or from the virus.
“I have no reservations — none whatsoever — about getting a hepatitis C kidney,” Price said in a follow-up phone call with Undark.
Still, there are lingering concerns. On the one hand, Roth, the University of Miami nephrologist, says that he embraces the idea of using hepatitis C-positive and other donor organs that function fine but aren’t in pristine condition. It’s one way to help partially ease the persistent organ shortage in the country, he says. But Roth is concerned that some patients may be so eager to escape the drudgeries of dialysis that they are willing to accept a sub-par kidney.
“When you have a population of patients who are vulnerable in that regard, it’s really incumbent on us to paint a very clear picture,” Roth said. “Many of them are so anxious to get off dialysis that they will accept a lot of things that maybe they’re not 100 percent certain what they’re accepting, and I think you have to be very careful about that.”
While studies of the general population suggest that cure rates from direct-acting antivirals hover at over 95 percent — a high number, especially when compared to previous hepatitis C cure rates — it’s still not 100 percent. Two participants in one of Sise’s trials weren’t cured after a single course of direct-acting antivirals, Sise acknowledged, though both were cured after a subsequent course. Another concern might be the development of antiviral resistance, especially as scientists try shorter courses of medications. “The more time the virus has to exist in someone’s body or only exposing patients to extremely short courses of therapy could potentially breed resistance,” Sise said.
In a 2018 review in the journal Clinical Liver Disease, a team of transplant surgeons and doctors from the University of Pennsylvania argued that organs from hepatitis C-positive donors should only be used as part of formal clinical studies at this time. The authors wrote that the procedures have too many unknowns, including the best protocols for what antivirals to take and for how long, as well as the long-term outcomes of those who have received these kidneys. Given how little researchers know about the use of kidneys from hepatitis C-positive donors, the authors wrote, “without sufficient knowledge to craft comprehensive post-transplant care plans, any further use of HCV‐infected donors, whether through a research protocol or so‐called standard of care, is arguably experimentation.” The following year, hepatologist David Goldberg, one of the co-authors of that review, participated in a meeting that developed consensus opinions on the use of such organs, one of which suggested that transplanting hepatitis-C positive organs into hepatitis C-negative patients is permissible as long as there is “rigorous informed consent.”

But all of the lingering qualifiers still make the decision to accept an imperfect organ a weighty one for patients living with kidney disease and the gauntlet of dialysis. Evans-Simmons says she contemplated the possibility of regret — both if she accepted a hepatitis C-positive kidney and if she didn’t. But after additional conversations with her nephrologist and her family, she decided to add her name to the list for people willing to consider a kidney from a hepatitis C-positive donor.
It didn’t remove her from the other, “regular” list, nor did it obligate her to accept the kidney. Her health insurance provider also still needs to agree to pay the high cost of the direct-acting antivirals before Evans-Simmons can receive a kidney from a hepatitis C-positive donor.
She’s still not 100 percent sold on the idea, but as she waits for the day when the phone will ring with news of an available kidney — any kidney — Evans-Simmons says that she is keeping an open mind. “It’s still very concerning for me,” she said of the prospect of accepting a kidney from a hepatitis C-positive donor. “But at the same time, I’d rather try that than be on the dialysis.”
This series was supported in part by the National Institute for Health Care Management Foundation.
Carrie Arnold is an award-winning freelance science journalist based in Virginia. In addition to Undark, her work has appeared with Scientific American, STAT, National Geographic, Wired, and The New York Times, among other publications.
Larry C. Price is a two-time Pulitzer Prize-winning documentary photographer and multimedia journalist based in Dayton, Ohio. He previously produced award-winning photography and video footage for Undark’s Breathtaking series on air pollution, which won a George Polk Award for Environmental Reporting in 2018.
PROFIT & LOSS: THE COMPLETE SERIES











Comments are automatically closed one year after article publication. Archived comments are below.
6 years ago I was found HBsAg positive and by taking Worldherbsclinic HBV herbal medicine, now I am negative. abdominal pain gone. All this happened between 2 months.
Am very happy to share my victory over HBV. I always knew i will beat this deadly disease, i never stopped researching for solution. Don’t ever give up, you will surely be free on day.