$475,000 for a Cancer Drug? Time to Put a Lid on Costs
On August 30, the Food and Drug Administration approved a first-of-its-kind treatment for a deadly form of childhood leukemia: a genetically engineered white blood cell that stimulates the body’s immune system to attack the cancer. The decision is the culmination of nearly five decades of work on so-called recombinant DNA research, but it raises troubling questions about the pricing of a new generation of biologic drugs and how we will pay for them.

The T-cell treatment, which is licensed to Novartis, will cost $475,000 per patient — a price that is all the more striking considering that general estimates for these types of medicines cite a manufacturing cost of $25,000. The company said that it would provide financial assistance to uninsured or underinsured patients, and that it would not receive any reimbursement if the drug doesn’t work. But these concessions — drawn from a playbook on how to price a new generation of biologic medicines as high as possible while negotiating their reimbursement from insurance companies — are not enough. Unless regulators cap the costs of such medicines, they will only intensify the financial pressure on a health care system that is already the most expensive in the world.
Well before the FDA announcement, the treatment had been given a public relations bonanza. In early 2016, Joe Biden, then vice president, shook hands with two of its leading developers during his tour to launch his $1.8 billion Cancer Moonshot. The scientists, Carl June and Bruce Levine of the University of Pennsylvania, had used recombinant technology to create a chimeric molecule that works as a receptor, enabling the immune system’s T-cells to bind to a protein on cancerous B-cells with the goal of killing them off. Hence the treatment’s name: CAR-T, short for chimeric antigen receptor T-cells.
In a Novartis trial of 63 children and young adults with B-cell acute lymphoblastic leukemia, 83 percent were cancer-free after three months. Every patient did suffer adverse events, and half suffered relatively severe forms of cytokine release syndrome, a chain of events that can lead to escalating heart rate, blood pressure collapse, fever, even death. But none of the patients died from such events.
Other T-cell trials have not gone as well. In March, Juno Therapeutics stopped a trial after 5 of 38 patients died from a mysterious inflammatory reaction in the brain. In May, Kite Pharma reported a death from a similar adverse event with another T-cell product. Novartis, though, believes its product is safer. The company, which just completed a $600 million campus in Cambridge, Massachusetts, thinks the technology — even though embroiled in patent fights and a tough regulatory process — could easily bring $1 billion in sales.
About 6,500 people in the U.S. are diagnosed with this form of leukemia each year, and 1,500 die from it. Novartis’s CAR-T is approved for children and teenagers with particularly persistent cases. The financial pressures on the insurance system will intensify if this new class of biologic medicines can be applied to a multitude of cancers, including solid tumors, as scientists hope.
Drug companies and their defenders explain the jaw-dropping prices of new drugs by appealing to the narrative that they were invented by a handful of whip-smart scientists who have a right to charge whatever the market will allow. But much of the research that led to biologic drugs and treatments like CAR-T was funded by taxpayers. Novartis didn’t invent this half-million-dollar drug, and it’s questionable whether the Penn scientists from whom it bought a license invented it either, or whether they were building on the work of the Italian researcher Dario Campana.
Furthermore, the technology is not an airtight solution. Genetically engineered immunotherapy drugs raise questions of safety and reliability, especially since everyone’s immune system is different. Richard C. Mulligan of Harvard Medical School — who in 1982, at MIT, engineered a virus that could be used to insert genes into human cells, and who later advised the National Institutes of Health on recombinant DNA — told me the FDA was “kind of scratching their heads” on how to evaluate biologics: “They’re used to situations involving a conventional drug, where its toxicity can be measured, and where there are more patients and more statistics.” Tania Bubela, a health policy expert at Simon Fraser University in British Columbia, noted that despite the approval of CAR-T, it’s still uncertain whether many hospitals will assume the risk of adverse events. “That goes back to tort liability, informed consent,” she said. “And not all institutions may be willing to take those risks.”
The gene modification system CRISPR has been hailed for its promise in re-engineering T-cells to prevent cancer cells from shutting down an immune response. But some scientists are not so sure the technology will vastly improve the state of the field. “You’re putting a lot of molecular machinery into cells and taking a lot of immunogenicity risk,” warned Jonathan Appleby, a chief scientific officer at GlaxoSmithKline in Britain.
Appleby, whose company hopes to sell a gene therapy in the U.S., said that many scientists held a cautious optimism, but were conscious the field was still grappling with a “fragile trust.” This trust is made more tenuous by aggressive pricing. Since the first biotech patents were issued in the 1980s, science has shifted to a mechanism of subsidizing biotech as a business. I have argued that large scientific institutions and their industrial partners will eventually mature into a robust infrastructure that can afford to fund their own basic research and business concerns. If federal and state regulators do not do more to contain the costs of drugs, and if access to health care becomes more unequal, scientists risk a public backlash that could set this shift in motion sooner than they might like.
Jim Kozubek is the author of “Modern Prometheus: Editing the Human Genome With CRISPR-Cas9,” published by Cambridge University Press.
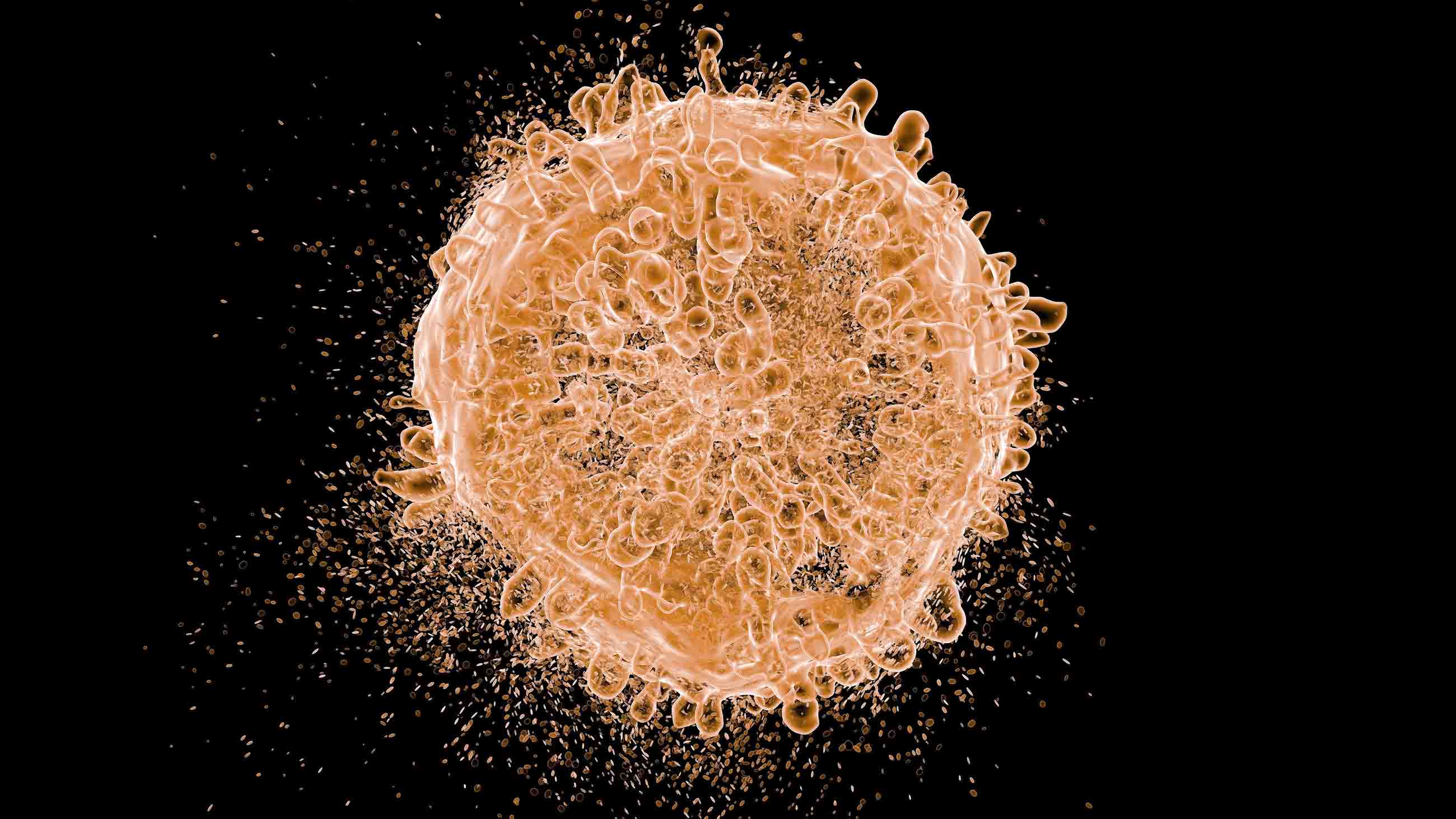
UPDATE: An earlier version of this article included a picture caption suggesting that the image depicted Novartis’s CAR-T treatment. It is a computer rendering of a leukemia blood cell, not of any specific treatment.