Can MDMA Therapy Ease the World’s Traumas? Critics Aren’t Sure.
When the war in Ukraine broke out, many countries and agencies around the world lent their support in the form of financial aid, weapons, and food. But Olga Chernoloz, a Ukrainian neuroscientist based in Canada, wanted to provide a different kind of assistance: a combination of therapy and the psychedelic drug MDMA.
Such therapy, she said, could help countless people on the ground who are suffering from psychological trauma. “I thought that the most efficacious way I could be of help,” she told Undark, “would be to bring psychedelic-assisted therapy to Ukraine.”
Chernoloz’s confidence stems in part from the results of clinical trials on MDMA to treat post-traumatic stress disorder in vulnerable populations, which suggest that such treatments may improve symptoms, or do away with them altogether. But the approach is experimental and has not yet cleared major regulatory hurdles in Canada, Europe, or the United States.
Still, Chernoloz, who is a professor at the University of Ottawa, plans on carrying out clinical trials with Ukrainian refugees in a psychedelic center in the Netherlands in early 2024.
This month, Chernoloz and her colleagues organized an education session for 20 Ukrainian therapists to learn about MDMA-assisted therapy for PTSD from the Multidisciplinary Association for Psychedelic Studies, or MAPS, one of the most influential organizations dedicated to education and promotion of psychedelic drugs.
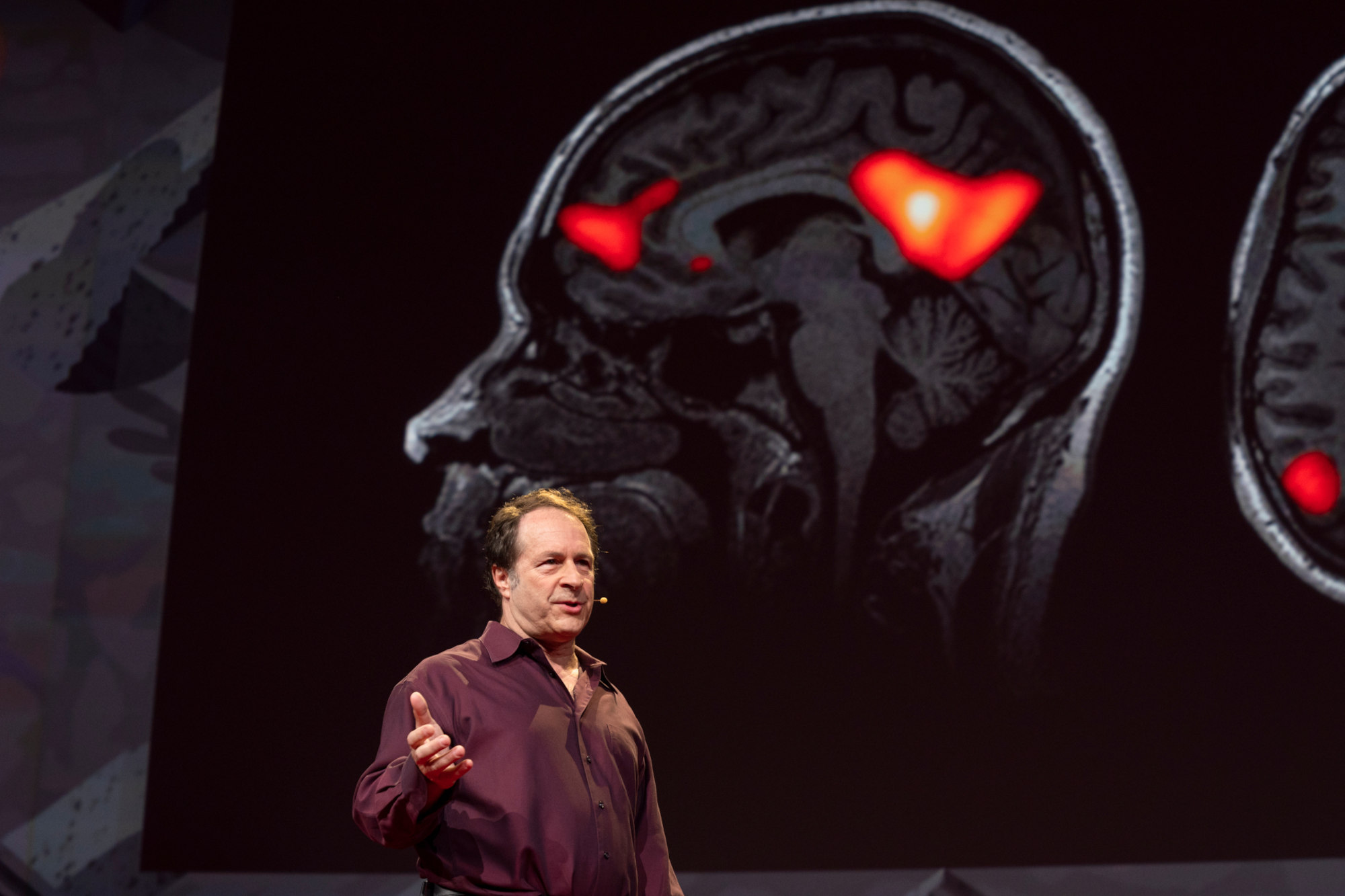
Chernoloz’s initiative is part of a larger, more ambitious project. More than a dozen countries currently facing war, or with a history of violence and discrimination, have similar ongoing initiatives led by MAPS, among them Afghanistan, Iraq, Rwanda, Somaliland (an unrecognized state), and South Africa, and Rick Doblin, president and founder of MAPS, calls these “humanitarian projects.”
“There’s always going to be accidents and diseases and natural disasters and human cruelty,” said Doblin. “But we want to stop the burden of trauma that is experienced collectively by humanity, and then is passed on.”
Ultimately, Doblin said he wants to achieve “net zero trauma by 2070.”
But to achieve those lofty ambitions, MAPS first needs to hit a key milestone: approval from the Food and Drug Administration in the U.S. Despite reported financial issues, the organization expects to obtain approval for MDMA-assisted therapy for patients suffering from PTSD by mid-2024, according to Doblin.
If MAPS gains FDA approval in the U.S. — and, later, its European equivalent, the European Medicines Agency — the organization will effectively have a monopoly on the market, and will aim to build the momentum and political leverage necessary to export MDMA-assisted therapy worldwide. But experts warn that the long-term mission to bring the therapy to war-afflicted regions is culturally, politically, and even scientifically fraught. Some critics say, for example, that MAPS’ training program so far has been overly focused on U.S. veterans, providing little relevancy for other nations. Others point out that evidence for MDMA’s efficacy in helping to treat trauma is mostly based on research in Western populations, with little data on how cultural differences might affect outcomes elsewhere. Some research also suggests that results can vary among different demographic groups, and potential adverse effects, some researchers argue, remain poorly understood.
Even with FDA approval, these and many other issues would need to be worked out before any safe and meaningful export of the therapy could unfold, many experts say.
In an email to Undark, Natalie Gukasyan, an assistant professor of psychiatry at Columbia University, wrote of the project: “If they do proceed with this plan, my hope is that the program is culturally informed, has robust consent practices (making it clear what is and isn’t known about this intervention), and has ample and flexible support available for those who participate.”
As of 2022, MAPS has trained therapists from nearly 40 countries, according to a list shared by the organization. It has not yet conducted any clinical trials investigating the use of MDMA-assisted therapy for PTSD in war-torn countries. That said, multiple MAPS-trained therapists in these countries have already had conversations with their respective health authorities and governments to discuss the possibilities of introducing MDMA-assisted therapy.
In Afghanistan, for instance, as of late 2022, the goal was to bring MDMA-assisted therapy to Taliban soldiers suffering from PTSD following the war with the U.S, said Murtaza Majeed, a MAPS-trained therapist who had negotiated clinical trials with the Afghanistan government before the Taliban took over. The plans have since come to an end.
In the U.S., MAPS clinical trials have so far provided MDMA to U.S. veterans traumatized by the war in Afghanistan, “so why wouldn’t we give this MDMA to Taliban as well, because they’re also, you know, being traumatized?” Majeed asked Doblin after a conference. Doblin agreed to give it a try.
To some, there’s no real reason to think these humanitarian projects won’t work out. MDMA and other psychedelic drugs have been used by communities around the world, often for therapeutic or spiritual purposes. “I don’t see why it shouldn’t work for whether your trauma is because of being raised in a war, amongst a war, or it’s you went to war and came back,” said Manoj Doss, a psychedelic researcher at the University of Texas at Austin Dell Medical School.
Still, multiple MAPS-trained therapists from the Middle East told Undark that, while the training was generally high quality, its focus on U.S. veterans didn’t really prepare them for how to bring MDMA to their respective homes.
“There was a lot of talk about, you know, trauma that veterans had from their involvement in war in the Middle East,” said Haya Al-Hejailan, a psychedelic researcher in Saudi Arabia. “That didn’t help me with understanding how I would help my population — if anything, actually was quite triggering to listen to that content.”
The science underpinning psychedelics and its intersection with demographic differences is also poorly understood. Most studies so far have used unrepresentative samples focused on Westerners, said Gukasyan, and “none of those studies even begin to address whether this intervention would be safe or effective” for places like Somaliland, “where most are living in poverty and may have very different customs and spiritual beliefs from Westerners who participated in MAPS’ early studies.”
One study, published in Nature, found that while White participants showed significant decreases in distress and suicidality after MDMA-use, these same benefits were either dampened or non-existent for racial and ethnic minorities, including Black and Indigenous participants.
MAPS’ trials have been conducted in at least three sites — the U.S., Israel, and Canada — and the results are consistent said Sergey Vardanyan, a MAPS-trained therapist who hopes to bring psychedelic-assisted therapy to his home country in Armenia, suggesting cultural differences may not play as large of a role in the outcomes. Gukasyan noted that all three countries are developed, with high levels of education; it’s unclear whether study results will hold across other countries.
Vardanyan acknowledged that there will inevitably be case-by-case challenges ahead. In Armenia, for instance, veteran soldiers tend to respond better when their therapist is a man, according to Vardanyan. “The stereotype that the man should be strong,” and that “they don’t want to show them being weak in front of the opposite gender,” he said. “Those are the things we need to work with.”
Given the sheer scale and complexity of the project, Doblin envisions adopting new, and sometimes clinically untested modes of delivering therapy. Clinical trials so far have two therapists per participant, but Doblin is eager to see if they can ramp this up in new contexts and cultures, such as therapy for entire families traumatized by a war.
“It could be like family clusters altogether,” he said, “which could mean also working with adolescents or potentially even kids that are younger.”
For all its ambition, MAPS is no stranger to controversy. The organization’s training protocols came under fire in 2021, when New York Magazine, in collaboration with Psymposia, produced a podcast about harm and abuse in the psychedelic space, including a story about a MAPS clinical trial participant who has accused her two therapists of sexual assault. The scandal opened the lid on a series of questions about MAPS’ training and protocols, and revealed that it was more of an art than science.
Therapists are told that the process involves “unlearning” what they might already know and trust the participant’s “inner healing intelligence” — a term MAPS defines as “a person’s innate capacity to heal the wounds of trauma,” said Joe Flanders, who trained with MAPS and worked as a co-therapist for one of the phase 2 MAPS clinical trials on PTSD.
Flanders said the ambiguities leave far too much room for interpretation and risk harming patients. “The notion of inner healing therapy,” said Flanders, is messy and ill-defined, adding that it was “a grab-all term that’s doing a huge amount of heavy-lifting.”
Another contentious practice MAPS encourages is the use of “nurturing touch.” MAPS’ latest version of their training manual says that therapists should use touch with “attention and care” and that “any touch that has sexual connotations or is driven by the therapist’s need, rather than the participant’s, has no place in therapy.” But critics say the term is still ill-defined and does not provide the necessary context for which touch may be acceptable.
And although multiple MAPS clinical trial participants Undark spoke to said MDMA-assisted therapy radically changed their lives for the better, not everyone comes out of these clinical trials feeling revived. “Following the trial I felt a bit lost at sea,” Sarah McNamee, who enrolled as a clinical trial participant to treat PTSD, wrote by email. In MAPS’ first phase III clinical trial, at least three of 42 participants reported increased suicidality and suicidal behavior in the two months following the study, according to a viewpoint McNamee co-published at JAMA Psychiatry earlier this year. Serious adverse effects are also “poorly defined” and “probably underreported,” concludes a systematic review of psychedelic-related studies.
Some experts stress that there should be greater scrutiny of MAPS’ clinical trial results. One of the biggest problems relates to the concept of blinding: In order to compare whether a drug’s effects on a participant is driven by a drug rather than their expectations, scientists try to design experiments so that participants don’t know whether they’ve taken a psychedelic or a placebo.
Support Undark MagazineUndark is a non-profit, editorially independent magazine covering the complicated and often fractious intersection of science and society. If you would like to help support our journalism, please consider making a donation. All proceeds go directly to Undark’s editorial fund.
|
But it’s “very hard, or some people say impossible” to achieve this with psychedelics, said Eiko Fried, a psychologist at the University of Leiden in the Netherlands, given that they elicit such powerful and conspicuous experiences.
When participants know they are on a drug during a clinical trial, it can inflate results, whereas knowing they’re not can have the reverse effect. That, combined with the fact that MAPS, along with media coverage on psychedelics, have been drumming up expectations for years means that results almost invariably become exaggerated, Fried added.
In some cases, expectations are so high that participants may prefer not to voice adverse effects. In an email to Undark, McNamee wrote: “I felt a heavy burden to avoid putting anything into the public sphere that could ‘hurt the movement.’”
In the U.S., one of the biggest and most consequential questions facing the psychedelic therapy industry is how MAPS will operate when, and if, it gets FDA approval. Many, MAPS-included, are largely in the dark when it comes to details.
Experts Undark spoke with said they believe the FDA will approve MDMA and therapy as a package, rather than the drug alone. If that’s the case, patients suffering from PTSD would need to take MDMA under yet-unknown restrictions, for example under supervision of a qualified health professional and in a clinical setting.
The problem, however, is that scientists are still missing key answers to basic questions. “One of the biggest issues is in understanding whether the effect is due to the drug, the psychotherapy, or the combination,” said Joshua A. Gordon, director of the National Institute of Mental Health.
A leading theory for how MDMA works is that it elicits powerful psychological experiences that induce a special receptiveness to change, said Gordon, but “it might be some other biochemical effect of the drug that causes the therapeutic change with or without the psychotherapy.”
Another major obstacle is cost. Experts in the field estimate the full treatment could cost tens of thousands of dollars. Most experts Undark spoke to agreed that cost would come from funding the therapy and paying and training therapists, rather than manufacturing the drug itself. MAPS clinical trial sessions involve three multiple-hour sessions, with therapists, plus integrative and pre-treatment sessions.
Amy Emerson, CEO of MAPS PBC, a subsidiary of MAPS, could not give an estimate cost for the treatment but said that company’s top priority at the moment was to try and make sure the treatment would be insurable for patients.
If MDMA-assisted therapy gets approved in the U.S., MAPS PBC will have exclusive use for around five years, due to an FDA law signed in 1984 aimed at allowing companies to recoup the costs of drug development. Pending approval in Europe, MAPS PBC may dominate that market for 10 years. Clinical trials in the continent were recently put on hold so that MAPS PBC could focus on drug approval in the U.S., said Tadeusz Hawrot, founder and executive director of Psychedelic Access and Research European Alliance, a nonprofit devoted to the safe and ethically responsible integration of psychedelic therapies in Europe .
Assuming everything runs according to plan, MAPS PBC has the potential to make multiple billions, said Doblin. The psychedelic therapeutic market is predicted to reach around $13 billion by 2031, according to an analysis from the market research and consulting firm InsightAce Analytic.
That’s not to say they’ll be a profitable company, said Josh Hardman, founder of Psychedelic Alpha, a website that tracks and publishes data on the psychedelic industry. Doblin said it will cost them about $350 million to clear the final FDA regulatory hurdles and reach profitability although others estimate this number at about $500 million and $1 billion. Peak sales also only come in at about five years into a drug’s launch, said Hardman, meaning they’ll be getting their revenues at the tail-end of their dominance in the market.
The organization also has financial issues to contend with. MAPS only has two months’ worth of cash available to continue its operations, according to recent news reports, in large part because investors have increasingly been putting their money in for-profit pharmaceutical companies that potentially yield high returns, rather than donating to MAPS. To survive, MAPS PBC is allegedly selling $85 million in shares to investors.
How this all will translate to war-torn countries remains to be seen. So far, cost predictions have primarily focused on the U.S., but “in other jurisdictions/other systems the cost of highly qualified labor is significantly lower, thus lowering treatment costs,” Chernoloz, the Ukrainian neuroscientist, wrote in a follow-up email to Undark.
She added that scaling therapy to groups would “enable drastic cost reductions” and is “well fitted for certain populations,” for example veteran soldiers for whom camaraderie and shared trauma might make it easier for them to open up.
“It’s entire generations being uprooted, traumatized,” said Chernoloz. “And to be honest with you, I don’t think that psychedelics are a solution. But it is a method of therapy that today shows to be far more efficacious in a variety of mental health disorders than anything that we currently have.”
Jonathan Moens is a freelance journalist based in Rome. His work has appeared in The New York Times, National Geographic, and The Atlantic, among other publications.











What would be interesting to hear in this piece is a comparison of the existing treatment efficacies AND their costs compared to what entheogens are likely to provide. How much are we spending on western insurance- and pharmaceutical-driven treatment, say SSRIs, and what percent of those patients benefit… a dollar-to-unit-of-trauma-relief, if you will. Then calculate that for entheogens based on the existing sample.
Also, the notion that it’s a white-dominated therapy approach may warrant tweaks for patients in Somalia, etc, but this is a therapy that the West has at first tried to snuff out (See: Nixon) and then has finally decided works, based on thousands of years of use by indigenous populations. This is THEIR therapy model and we’re finally borrowing it. (See: Richard Schulte, Terrence McKenna, and others who have written extensively about their first-hand experience with shamans.)
Another questionable statement in this article is the proposition that there is a risk to patients who DON’T enlist the assistance of a trained therapist to administer this?
That is laughable to anyone familiar with the proper use of entheogens therapeutically.
Just my two cents. I could be wrong.
Thanks for reading. :)