In 1945, bacteriologist Alexander Fleming saw the future. Doctors and nurses were using penicillin, which Fleming had discovered 17 years prior, to save countless lives from once untreatable infections. But upon accepting the Nobel Prize for Physiology or Medicine that year alongside colleagues Ernst Chain and Howard Florey, he worried about the day when the drug might falter.
“The time may come when penicillin can be bought by anyone in the shops,” Fleming said. “Then there is the danger that the ignorant man may easily underdose himself, and by exposing his microbes to non-lethal quantities of the drug, make them resistant.”
Seven decades later, in 2018, an equivalent of more than 40 billion doses of antibiotics were doled out to the world’s population, according to a study in The Lancet Planetary Health. A later study, published in 2022, used global predictive models to attribute almost 1.3 million deaths to antimicrobial resistance in a given year — as many people who succumb to HIV and malaria combined. That number is expected to rise: Researchers believe that infections impervious to antibiotics, which have steadily risen over the course of the Covid-19 pandemic, will claim nearly 10 million lives annually by 2050. Such infections have become modern medicine’s silent scourge. Even relatively common bacteria are now becoming resistant to time-honored therapies.
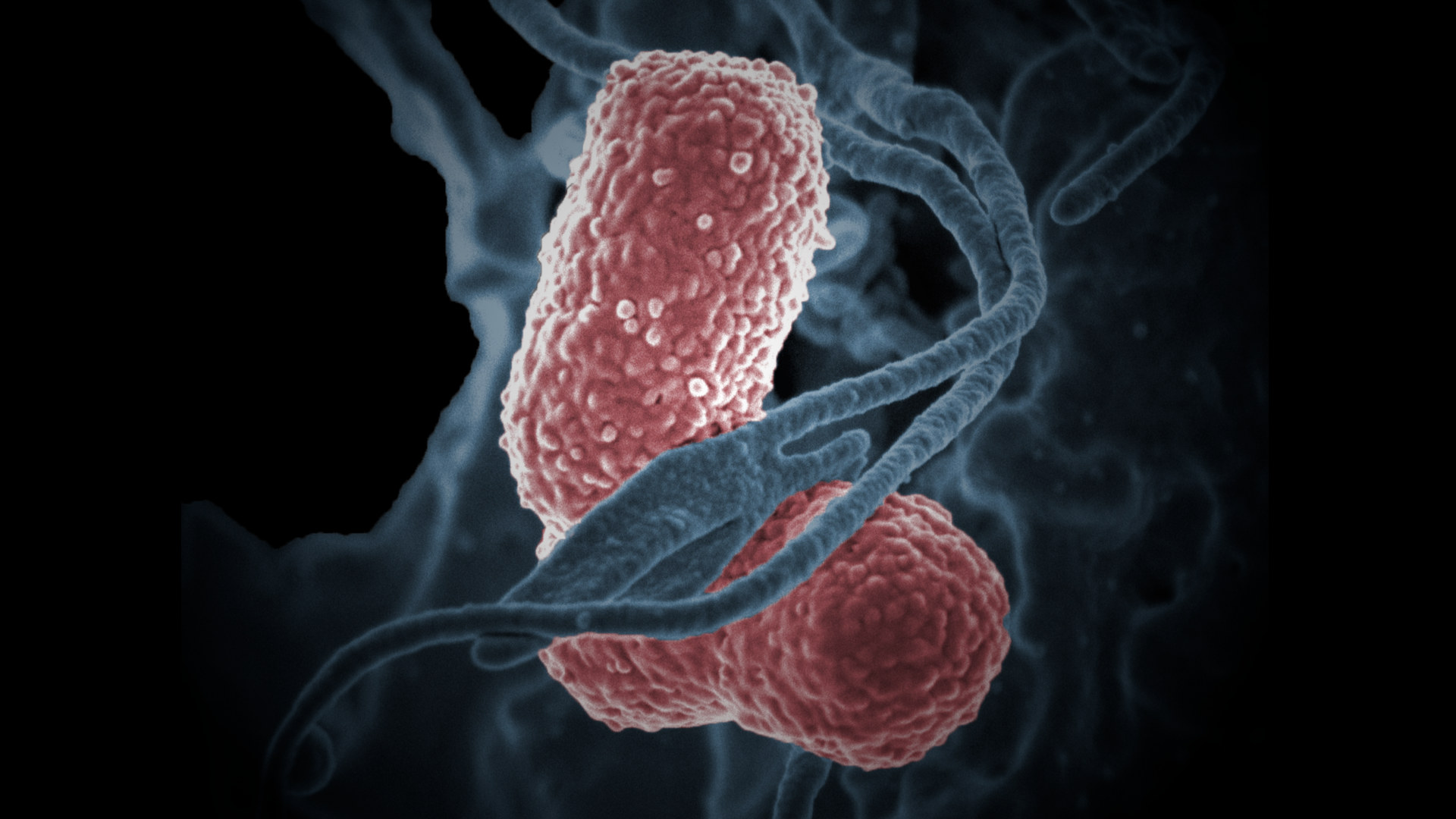
To meet the growing challenge of antimicrobial resistance, researchers from MIT, Harvard, and McMaster University recently reported discovering a novel antibiotic using artificial intelligence. Abaucin, as they call it, inhibits the growth of the bacterium Acinetobacter baumannii. The microbe, one of the most resistant in existence, often infects people in hospitals. It clogs patients’ lungs with pneumonias and circulates through their bodies as bloodstream infections. Its fiercely resistant incarnations carry a mortality rate of almost 25 percent. Those disturbing effects led the World Health Organization to declare in 2017 that A. baumannii was one of the pathogens in greatest need of new treatments.
Reading about the discovery of abaucin initially left me, as one of a league of physicians whose mission is to diagnose and treat the array of infections that can affect us, in a floating kind of awe: A trained neural network shrunk a tedious screening process that takes weeks to mere hours. Abaucin is also unique because it targets a select bacterium — unlike conventional antibiotics, which knock down a broad range of bacteria but leave some that are not so readily killed. The progeny of those survivors, in turn, are more likely to resist antibiotics they later face.
The ability of AI to rapidly increase the number of potential antibiotics is embodied in new policies such as the bipartisan PASTEUR Act of 2021. Reintroduced to the U.S. Senate in April, it hopes to incentivize pharmaceutical companies to speed up the sluggish pipeline of antibiotics. (Only 12 were approved for use between 2017 and 2021.) The bill hinges on a philosophy of having plenty of alternative drugs on deck, given that resistance to most new agents develops only a few years after they’re introduced.
It’s fair to wonder if AI will allow us to outpace an evolutionary advantage conferred to an organism that, for billions of years, has mounted resistance to ensure its survival. Most concerning is that scientists and policymakers will rely on this strategy alone to parry the tsunami of antimicrobial resistance and assume that AI can absolve humanity of the various indiscretions that have brought it crashing our way. Once again, we would be reacting to, instead of preventing, the problem.
The impulse to develop new antibiotics is the inevitable fallout of irresponsibly using the ones we already have. In health care, antibiotics are routinely misused. They are often administered for longer than they should be, for infectious syndromes in which bacteria are not implicated, and for “treating” bacteria that benignly inhabit our bodies.
As a physician working in infectious diseases, I do as much to stop the use of antibiotics as to start them. Studies suggest almost a third of antibiotics are dispensed unnecessarily. And in nursing homes, about a tenth of residents are on an antibiotic at any moment, 40 to 75 percent of which, according to the Centers for Disease Control and Prevention, were likely prescribed inappropriately.
But the truest damage is done far from any place where a patient or a health care worker sets foot: the cramped, caged, and unsanitary conditions of livestock feedlots.
Some countries, like the U.S., are known to divert as much as 65 percent of their national antibiotic inventory to cattle, swine, and poultry. After a New York laboratory in late 1949 found that subtherapeutic doses of antimicrobials would enhance the animals’ feed-to-weight ratio, agricultural industries began giving low doses of these drugs to livestock over prolonged periods to increase profits. And no situation, it turns out, is better for breeding resistance. Where animal antimicrobial consumption has increased, so has the isolation of antimicrobial resistant bacteria in humans, and vice versa.
Farming and pharmaceutical lobbies have long fought in tandem against governmental efforts to limit antibiotic use in livestock. California enacted a law in 2018 that restricted antimicrobial use to veterinarians, yet research has shown that little has changed. Canada passed a similar law the same year, but two years later, the share of the country’s antimicrobial supply ingested by livestock had increased.
In the U.S., where more than 10 billion land animals are killed for food each year, the Food and Drug Administration issued the same guidance in 2021. It took full effect in June. What, if any, impact this federal directive will have is hard to guess, especially given that, in order to fulfill the insatiable global demand for meat, antimicrobial use in farming is expected to increase another 8 percent by the end of the decade.
Solving the problem of antimicrobial resistance faces the same challenge presented by most points of public health. Finding individual solutions — even remarkable ones — is not enough. Rather, the key lies in finding solutions that function in unison.
The thought of AI reaching so many corners of our society fills many of us with an existential dread. In some realms, like drug discovery, AI holds the prospect of offering help. But a human responsibility will be needed nevertheless. What would stop our most crucial medicines from being indiscriminately fed to our animals or overprescribed to our patients?
Only human intelligence, with proper policies and attitudinal shifts to govern the faithful use of antibiotics, can mitigate the collective negligence that has caused resistance to run amok.
Arjun V.K. Sharma is a writer and clinical fellow in infectious diseases at Western University.