The Ephemeral Organ: Researchers Look Closer at the Placenta
When Mana Parast was a medical resident in 2003, she had an experience that would change the course of her entire career: her first fetal autopsy.
The autopsy, which pushed Parast to pursue perinatal and placental pathology, was on a third-trimester stillbirth. “There was nothing wrong with the baby, it was a beautiful baby,” she recalled. We’re not done, she remembers her teacher telling her, go find the placenta.
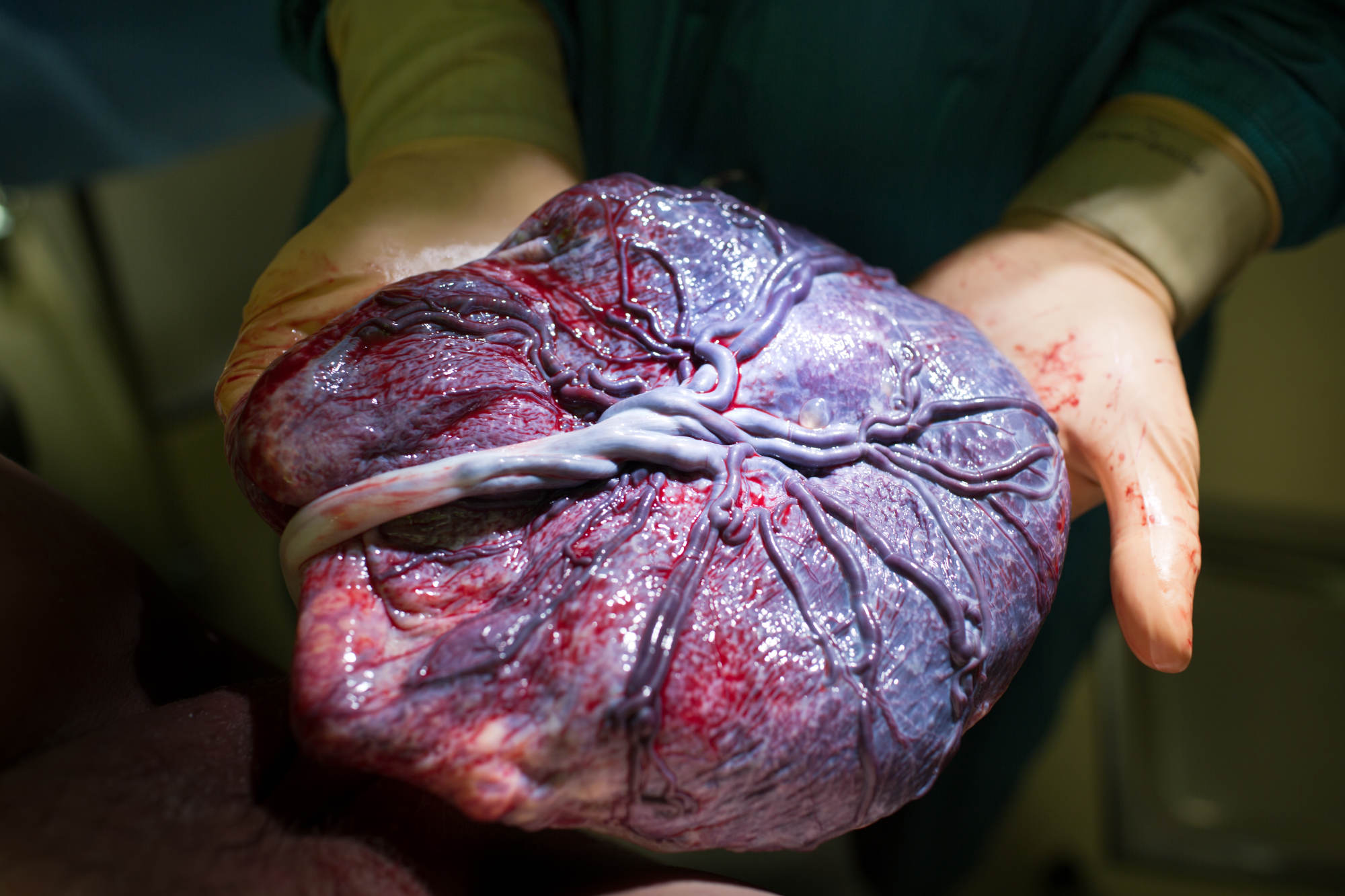
The placenta, a temporary organ that appears during pregnancy to help support a growing fetus, didn’t look as it should. Instead, it “looked like a rock,” said Parast. As far as they could tell, no one had ever examined this patient’s placenta through her pregnancy, and it was her fifth or sixth stillbirth, Parast recalled.
Every year, there are approximately 5 million pregnancies in the United States. One million of those pregnancies end in miscarriage, and more than 20,000 end in stillbirth. Up to half of these pregnancy losses have unidentified causes. Recent and ongoing research, though, suggests that the placenta may hold the key to understanding and preventing some pregnancy complications, such as preterm birth and maternal and infant mortality. A closer look at the placenta — including its size and function — may have a significant impact on stillbirth rates.
Still, the placenta and its pathologies have largely been understudied, some clinicians say. There are multiple reasons why: the difficulties in studying a fleeting and dynamic organ, the limitations in researching pregnant people, a lack of scientific consensus, few prospective studies, and the absence of standardized pathology reports on placentas.
Some groups are working to change that. The placenta “is this complex organ that’s critical to support fetal development, so you would think we know everything about it,” said David Weinberg, project lead for the Human Placenta Project, or HPP, an initiative by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The project has awarded studies more than $101 million from 2014 to the fall of 2023 to develop better assessment tools for the placenta while it is growing inside a pregnant person.
In the U.S. every year, 1 million pregnancies end in miscarriage, and more than 20,000 end in stillbirth. Up to half of these pregnancy losses have unidentified causes.
Placental research is an area of obstetrics that is sorely lacking, according to Weinberg. While limited research has been done on abnormal placentas after delivery, the HPP research teams realized in early meetings that if they wanted to improve outcomes, they’d need to know more about what a normal placenta does over the course of pregnancy. They are one of several U.S. based teams tackling this issue.
The shift in research is a welcome one for Parast, who is now director of the Perinatal Pathology Service and co-director of the Center for Perinatal Discovery at University of California, San Diego, and has received HPP funding for some of her work. But more should be done, she added, including adopting a more cooperative approach to applying new findings: “If we’re going to do this right, we have to come at it with this mindset.”
The human placenta does a lot of work for the fetus; it is, effectively, the fetal lungs, kidneys, and digestive tract. It’s also one of the only organs in the animal world that consists of two separate organisms — with tissues from both the mother and fetus — as well as the only temporary organ.
The placenta evolves across a pregnancy, too, continuing to support the developing fetus while interacting with the maternal environment, said Weinberg. The research has, so far, shown that issues with the placenta — its size, its placement, its microbiome — can signal health problems with both pregnant person and fetus, such as preeclampsia, gestational diabetes, preterm birth, and stillbirth.
As researchers have tried to develop ways to observe the placenta throughout the course of an entire pregnancy, they’re facing challenges, though. It’s difficult, for instance, to study the organ before a birth, due to potential risks both for the woman and for her developing fetus. Pregnant women have been historically excluded from medical trials according to National Institutes of Health Office of Research on Women’s Health. The potential reasons include threat of legal liability should the study harm the fetus, and the complex physiology of the pregnant body.
Because research on pregnant women faces so many restrictions, the largest body of placental research has been done after birth in a pathology lab. Here, the organ is typically only examined after a poor pregnancy outcome, such as stillbirth or placental abruption, in which the placenta pulls away from the uterus wall and causes heavy bleeding.
Placental pathology, though, has also long had limitations. “No one in their right mind was studying placentas,” said Harvey Kliman, director of the Yale School of Medicine’s Reproductive and Placental Research Unit, when recalling the early years of his pathology training in the 1980s when the organ was particularly understudied. As a medical student, he said, “I was discouraged from going into OB/GYN. I was told you can’t really do research on pregnant women. This is still basically true.” Conducting OBGYN research can be particularly challenging compared to other fields of medicine, he added.
While the advanced pathology residents were working on cancer, Kliman said newer residents started in the basement morgue performing autopsies on placentas and fetuses. Even today, there is a hierarchy in pathology, and placental pathology is at the bottom, he said, akin to “scrubbing toilet bowls in the Navy.”
“A placenta review after loss can take up to six months, because there’s no priority — there’s no patient on the table,” said Kliman. Most pathologists, he added, “don’t see the human side of this at all. I deal with patients every day. This is very real to me.”
The human placenta does a lot of work for the fetus; it is, effectively, the fetal lungs, kidneys, and digestive track.
Parast said that the culture of pathology is partly responsible for lack of placental recognition, because they often work in isolation from each other: “If there’s a perinatal pathologist, they’re the only one. So few people are doing this.”
Historically, getting pathologists to come together and agree on the details of placenta work is difficult; to change that, Parast has been working with PUSH for Empowered Pregnancy, a nonprofit that aims to end preventable stillbirths, along with other advocacy groups such as Star Legacy Foundation. Parast has also pushed the Society for Pediatric Pathology to come together and standardize the way placental autopsy reports are written. This a big complaint among obstetricians and advocates, she said, because when it comes to the reports as they are now, “no one understands them.” She added that clinicians also need more training on how to interpret them.
Placenta research is also hampered because of how science is done more broadly, said Michelle Oyen, an associate professor of biomedical engineering at Washington University in St. Louis. Competitive grant proposals and funding incentives tend to dissuade collaboration and methodology sharing. But building improved obstetrical outcomes requires collaboration between engineers and OBGYNs, she explained. Historically, she added, there hasn’t been a relationship between those fields unlike other areas of medicine, such as orthopedics or cardiology.
Also at issue are shame and stigma around pregnancy loss — and women’s health in general. “It’s not just about the science, it’s about the fact that these problems are much bigger than most people understand,” Oyen said, referring to the systemic, gender-based obstacles in medicine. And NIH funding, which supports biomedical and health research disproportionately goes to diseases that primarily affect men, according to a 2021 study published in the Journal of Women’s Health.
Furthermore, a 2021 study in the journal Science showed majority female teams of inventors are much more likely to pioneer new inventions in women’s health than majority male teams, said Oyen, “so it is a patriarchy issue.” With the majority of patents being held by men, “there is a balance problem there.”
That may be changing. “Women’s health is having a moment. Those of us who have been working quietly on this for 25 years are laughing about it,” she added. “Like we’ve been doing this this whole time, and suddenly, you’re really interested in it.”
Research efforts like the Human Placenta Project aim to build a new research base on the ephemeral organ. Now, 10 years into the HPP, researchers have a better understanding of the organ and its role in pregnancy outcomes. They are developing tools to monitor the placenta non-invasively, Weinberg said, such as advances in magnetic resonance imaging and ultrasounds, both of which can help better visualize the placenta and its blood flow.
“We’re at a point of clinical validation,” he said. “Researchers think they have a measure that can indicate whether or not a fetus may be a risk.” Prospective studies are the next step.
Unfortunately, none of these projects will be market ready in the near future, he said, although he argues that the project has brought national attention to the placenta.
“I do believe the HPP raised global awareness,” said Weinberg. “Things that seemed sci-fi not that long ago are now a possibility.”
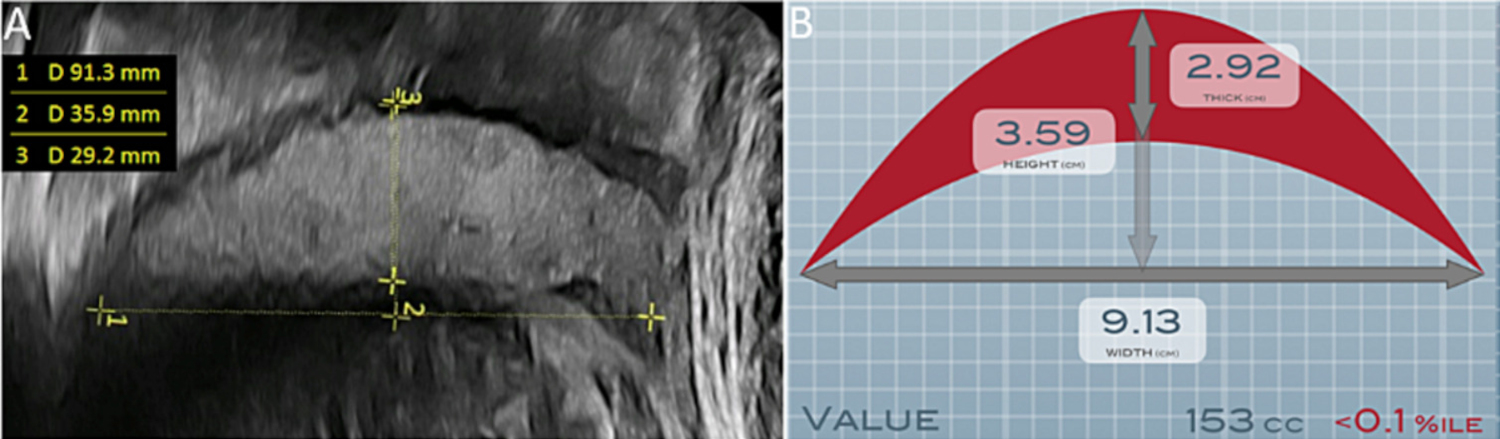
Still, some clinicians and advocates are disheartened by what they feel is slow progress with big projects like the HPP, including Kliman and the advocacy groups PUSH and Measure the Placenta. Kliman’s placental research has highlighted the role of a small placenta as the leading cause of stillbirth. An unusually small placenta, he said, is a stillbirth risk because fetuses can grow too large for it; this may cause the fetus’s growth to stagnate, or make the organ simply give out.
Diagnosing a small placenta is “low-hanging fruit,” he said, estimating that it could prevent 7,000 stillbirths per year.
“Things that seemed sci-fi not that long ago are now a possibility.”
A recent study that Kliman co-authored in the journal of Reproductive Sciences showed that in the pregnancy losses they studied, one-third of previously “uncategorized” stillbirths can be attributed to a small placenta. His team reviewed clinical data and placental pathology for more than 1,200 unexplained pregnancy losses and determined that the number one cause of stillbirth is a small placenta. This article, the most popular Reproductive Sciences article of 2023, has hopefully opened up a door to confirming where these losses are coming from, he said.
In 2009, together with his father, an electrical engineer and a mathematician who has since passed away, Kliman developed a 2D ultrasound measurement tool called Estimated Placental Volume which takes about 30 extra seconds at a routine ultrasound. But although the tool launched 15 years ago, getting it implemented has proven difficult.
Whether or not his EPV tool will become standard across obstetrics is still uncertain, he said. “We’re dealing with a paradigm change and there’s a lot of resistance to changing the paradigm.”
Other groups are also developing new tools for placental health. Oyen, for instance, is part of In Utero, a $50 million program funded by Wellcome Leap, a U.S. program which aims to halve stillbirth rates globally. For research on the placenta — and maternal and fetal health more broadly — the stakes are particularly high, she said: “Right now, all of the statistics on maternal and fetal mortality are going in the wrong direction in this country.” Although fetal mortality rates have held relatively steady in the most recent years for which there is data, Oyen emphasized that stagnating is not improvement.
Oyen’s team is working to develop new ways to see how oxygen flows in and out of the placenta, using high resolution imaging and modeling. The models could help determine how the placenta is working and, ultimately, detect if there is growth restriction.
The project follows a collaborative model with more than 15 teams around the world made up of biomedical engineers, clinicians, and computer scientists. Because of this, Oyen argued, the project is more nimble than traditional research: “We have all these data sharing agreements. We share techniques, we share information within this program. This is a model for how we have to move forward.”
“OBs need to come out and say we need this. If there’s a little bit of a push from the OBs, our societies will catch on.”
Getting obstetricians to implement these new findings in placental research will be the next big push, and in the U.S., that means taking the consensus to the American College of Obstetricians and Gynecologists — the herald of standard of care practices and guidelines for obstetricians.
Professional societies need to develop guidelines, Parast said: “OBs need to come out and say we need this. If there’s a little bit of a push from the OBs, our societies will catch on.”
More than 20 years ago, when Parast processed her first placenta, the one that looked more like a rock than an organ, she and her teacher identified accumulation of protein-containing material that indicated an underlying condition, possibly autoimmune, she said, which may have restricted the fetus’s growth. Had someone looked at this patient’s placentas sooner, said Parast, her multiple stillbirths may have been prevented with treatment.
Claire Marie Porter is a health and science journalist whose work has been published in Scientific American, The Washington Post, WIRED, and more.










Comments are automatically closed one year after article publication. Archived comments are below.
I wholeheartedly agree that more needs to be done to understand the placenta. I am a retired L&D nurse who saw many IUFDs during my career, which often included beautiful term babies who appeared to have nothing wrong, but nonetheless were not born alive. During my own pregnancy in 1983, I started having preterm contractions at 28 weeks, and I was subsequently induced at 30 weeks 5 days gestation because of IUGR. Being an L&D nurse made me more acutely aware of the fetal monitor strip, which showed absent variability and recurrent late decelerations. At delivery, the placenta was noted to be small in size (which made me realize the reason I had been having preterm labor was that the placenta was basically telling us that it was done and couldn’t support this baby any longer), and it had a short cord and abnormal cord insertion. My daughter weighed 1190 grams. The path report later also revealed a 4-vessel cord (3 arteries and 1 vein). I am extremely grateful that my pregnancy did not end with a fetal demise, but I hope that with more research and knowledge of placental function, more advanced monitoring, and increased pregnancy surveillance, that we can achieve better pregnancy outcomes in this country.