The Challenge of Providing Treatment for Children With Anorexia
Tess Olmsted stopped eating sugar when she was just 12 years old. She had previously been treated for obsessive compulsive disorder, or OCD, and soon found herself following rituals around eating. “For me it was never, ‘Oh I need to get skinnier,’” she recalls. Once she started to diet, she simply couldn’t stop.
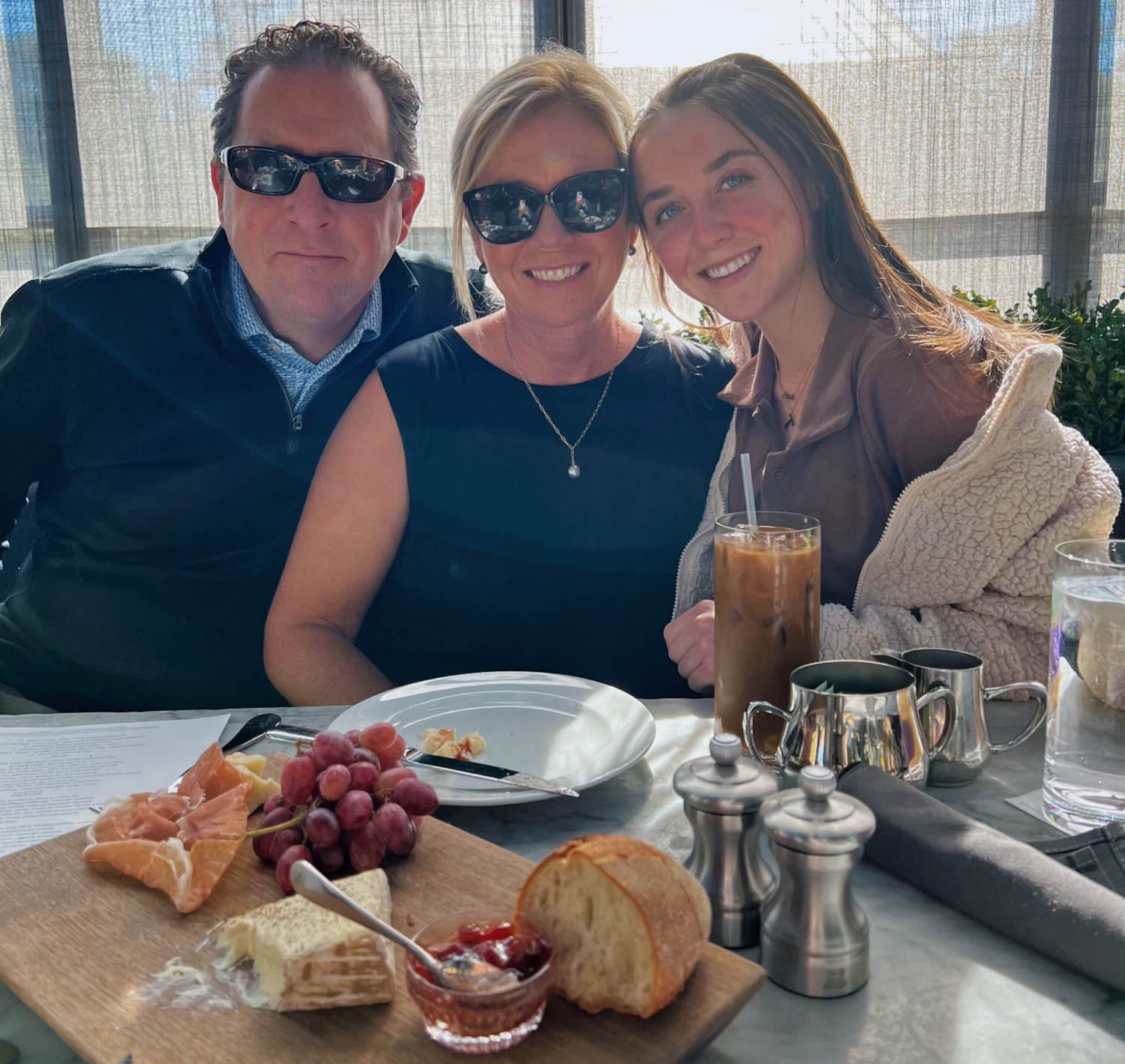
Two years later, on a summer day in 2019, her father saw her on the family’s patio wearing a loose-fitting swimsuit. He soon noticed how little Tess was eating and insisted she see the pediatrician. During a subsequent appointment with a specialist, he recalls, the family learned that Tess’s blood pressure and heart rate were dangerously low. She was admitted to a hospital in life-threatening condition.
Across the United States, up to 2 million adults have had anorexia, a mental health condition in which a person severely restricts their food intake, often due to an intense fear of gaining weight. Almost 1 percent of all U.S. women will experience anorexia at some point in their lives. Patients are developing the condition increasingly early in life — sometimes as young as 8 years old — and new figures suggest that symptoms in children worsened during the Covid-19 pandemic, leading to increased numbers of hospitalizations. At one treatment center in Michigan, the admission rate of young people aged 10 to 23 more than doubled during the pandemic’s first year.
These sobering developments are due, in part, to the fact that there are no drugs or devices approved by the U.S. Food and Drug Administration to treat the condition. For adults, there are three first-line treatments: an adapted form of cognitive behavioral therapy, known as CBT-E; a structured psychotherapy designed with patient input; and an approach that combines psychotherapy with nutritional support. Studies have shown that these approaches can help more than 50 percent of patients. But experts acknowledge that the studies are not high quality. Patients with anorexia are hard to engage in treatment, and as a result, studies are small and drop-out rates are high.
For patients younger than 18, one psychological intervention — family-based treatment, or FBT — has emerged as a leading evidence-based treatment in randomized clinical trials. The approach takes up to a year, and for part of that time, parents assume total control over planning, preparing, and supervising the child’s meals. In one clinical trial, nearly half of patients maintained a full recovery a year after follow-up.
Almost 1 percent of all U.S. women will experience anorexia at some point in their lives. Patients are developing the condition increasingly early in life — sometimes as young as 8 years old.
Since family-based treatment was rolled out in the U.S., the United Kingdom, and elsewhere, many families say that this intervention has helped their children. Even so, some experts warn that it’s not for everyone. Parents may be ill-suited for acting as full-time chefs and meal-planners, and they may not be financially able to take time away from work to do the therapy. And critics point out that the approach blurs the boundaries between home and hospital while failing to probe the condition’s psychological causes.
“At least in my case, FBT definitely backfired,” said a 19-year-old from Texas, who said her mental health got worse while she was in treatment. (The young woman asked to remain anonymous due to the stigma that surrounds eating disorders.)
When the Olmsteds eventually tried FBT, they also struggled with the demands of the protocol, which sparked fighting, tension, and even calls to the police. But Tess and her parents say the end result was worth the tribulation: Family-based treatment really worked. “I don’t want to go overboard,” Tess’s dad, Kevin, said. “But it probably saved her.”
Anorexia nervosa occurs when a person loses more than 20 percent of their body weight within a six-month period or has a BMI of less than 18.5 in adults (although BMI is increasingly seen as a flawed criterion for assessing health). The condition can disrupt menstrual periods and cause a soft light hair, called lanugo, to grow on the body. Anorexia can lead to kidney and heart problems, and even death. The condition is distinct from bulimia nervosa, a condition in which patients overeat and then empty their stomachs by vomiting or using laxatives. But patients can slip from one condition to the other with time.
Anorexia is one of the hardest psychiatric illnesses to treat, partly because of what psychologists call its “egosyntonic” nature — it offers those who suffer from it unique rewards, which make them value their illness. In one study, for example, patients said the weight-loss allowed them to feel safe, structured, and in control. Others described their dieting as a unique skill that made them special, even superior to other people.
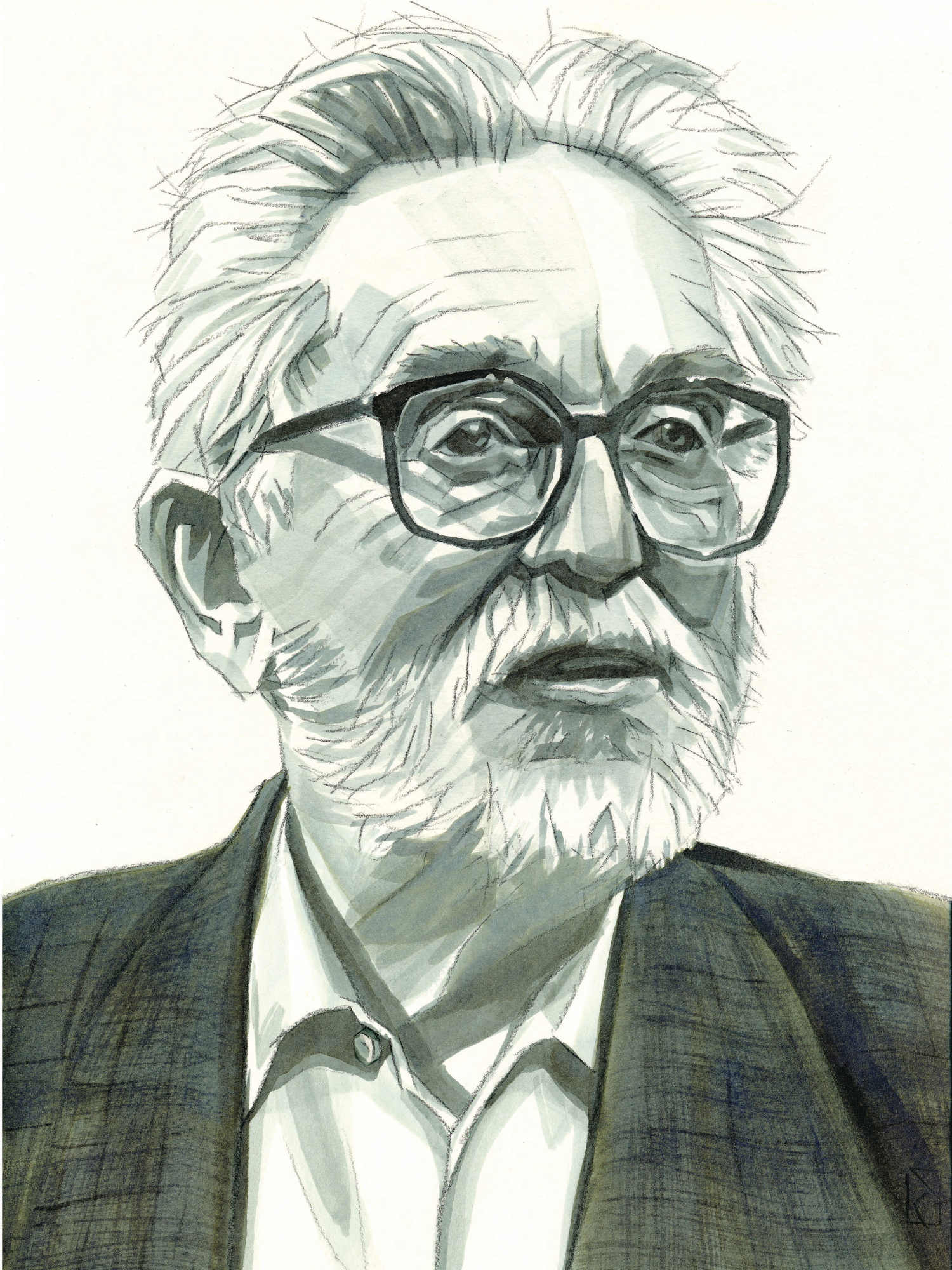
“When you have someone who’s successfully restricting, they don’t necessarily see too many downsides of it,” said Zafra Cooper, a professor of psychiatry at Yale School of Medicine and an emeritus professor of clinical psychology for the University of Oxford Department of Psychiatry.
“At least in my case, FBT definitely backfired,” said a 19-year-old from Texas.
The condition was first described by a Parisian neuropsychiatrist, Ernest-Charles Lasègue, in 1873. He described an illness he called hysterical anorexia, in which a female patient gripped by emotional suffering, would abstain from food. Around the same time, a British doctor, William Withey Gull, described a similar condition occurring primarily in young women and characterized by “extreme emaciation.” Gull prescribed milky foods, soup, eggs, fish, or chicken every two hours accompanied with a shot of brandy.
Doctors came to view parents as having a pernicious role in the illness and urged their exclusion from care. This is perhaps not surprising, said Daniel Le Grange, a professor in the psychiatry department at the University of California, San Francisco. The mental health field has a long history of blaming parents, mothers in particular, for a child’s diagnosis, he said. Practitioners even developed a specialized vocabulary to express this supposed problem: “the ‘schizophreno-genic mother,’ ‘autisto-genic mother,’ ‘anorexi-genic mother,’ and so on.”
By the 1960s, anorexia was thought to affect about 1 in 10,000 women, although under-reporting and lack of awareness are likely to distort any long-term surveys. At the time, information about the illness was still not available in medical schools, said Patricia Santucci, who has been a fellow of the American Psychiatric Association and is a founding member of the Academy for Eating Disorders. This left practitioners ill-prepared for what they would encounter, she added: “All of a sudden, you got out in practice. And you said, ‘What’s going on here? What is this thing?’”
The mental health field has a long history of blaming parents, mothers in particular, for a child’s diagnosis.
Providers would try to reshape patients’ behavior through punishments and rewards, according to Andrea Marks, a pediatrician who published a paper on the history of anorexia treatments in the Journal of Clinical Psychology in 2019. Throughout the 1980s, struggling patients would typically be hospitalized and put on a feeding tube. As they gained weight and started feeding themselves, they could earn privileges such as unsupervised time in the bathroom and visits from friends and family. Still, Marks writes, patients often found themselves stuck in a cycle of recovery, relapse, and return to the hospital.
In the 1980s, an innovative approach emerged. Salvador Minuchin, the famed Argentine-born therapist who cared for troubled teens by focusing on their families, had devised a model for treating anorexia, as had a group of therapists in Italy. Gerald Russell, a psychiatrist at the Institute of Psychiatry and the Maudsley Hospital in London, wanted to verify the two groups’ claims in a clinical trial, hoping to figure out if families might be able to help their loved ones achieve a more durable recovery.
Russell developed an approach that lasted 12 months or longer that included all members of the household. The treatment steps used in that trial later evolved into family-based therapy’s three main phases: The first is re-feeding, in which parents are tasked with making all decisions about the child’s food consumption and exercise. After the child has regained the weight, they are able to assume responsibility for their own eating — a change that marks phase two. In phase three, the family and psychologist review the outcome.
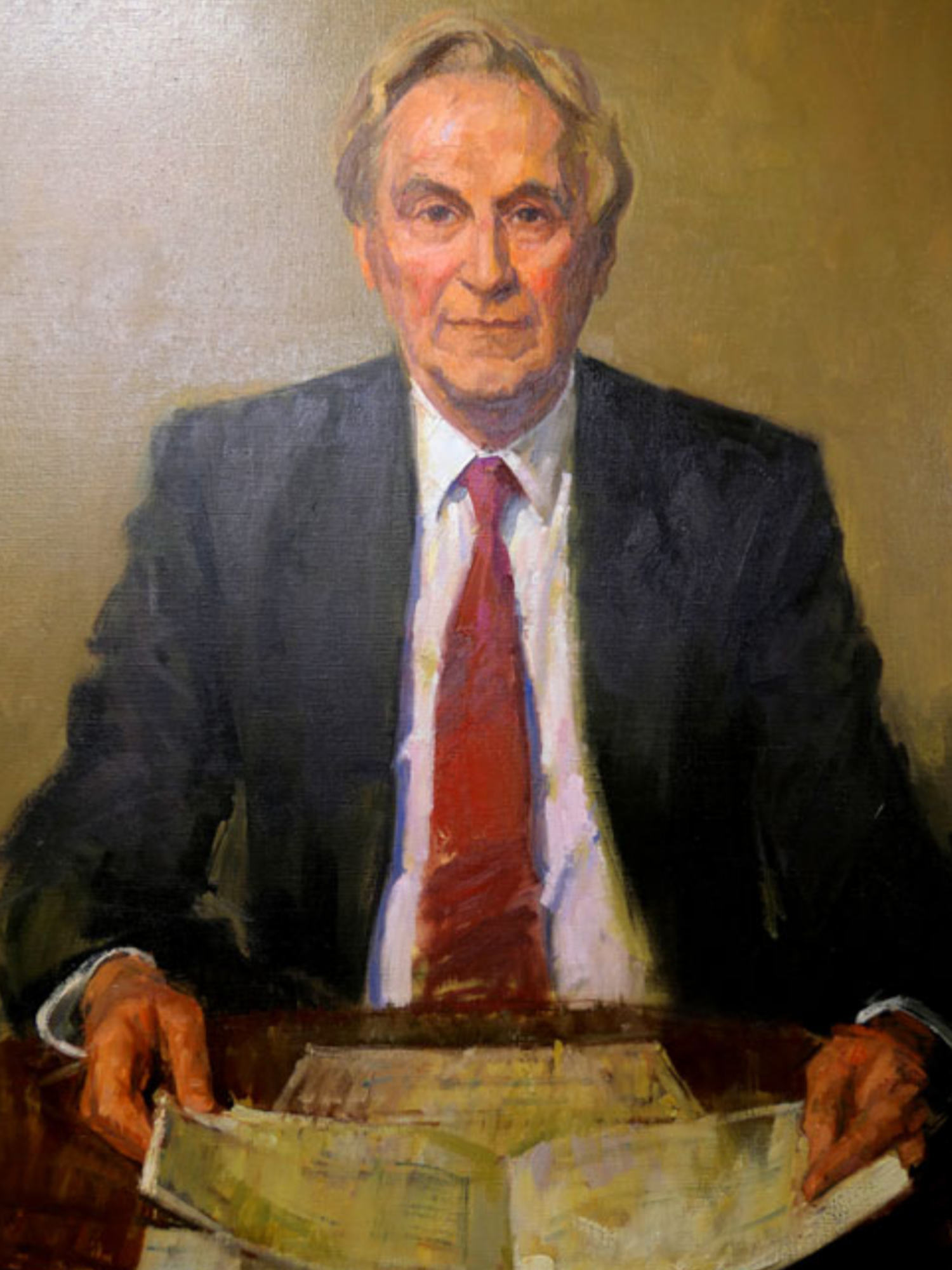
In family-based therapy, anorexia is viewed as an external threat, akin to a medical illness that must be vanquished. Parents are called on as helpers while therapists guide them through the process. Professionals do not try to explore what caused the illness, and above all, they must not suggest that it’s the parents’ fault. This refusal to place blame on parents “was really a profound sea change in our field,” said Le Grange, who joined the Maudsley Hospital team in 1986 just as Russell and his colleagues were preparing to analyze the results of a pivotal study comparing FBT with individual therapy.
Russell’s study was a randomized controlled trial of 80 patients between the ages of 14 and 55. Fifty-seven had anorexia and 23 had bulimia. As it turned out, patients who had developed anorexia when they were younger than 18 and had lived with the condition for less than three years and then received family therapy showed markedly better outcomes than their peers who had been randomized to individual therapy: six out of 10 had a “good” outcome, according to the authors, compared with one out of 11 in the individual-therapy group. The results were published in 1987.

The Maudsley Method was named after the institution where it originated — Maudsley Hospital in London. The method is known as family-based treatment, or FBT, in the U.S.
Visual: SLaMNHSFT/Wikimedia Commons
Five years on, the team revisited the 80 patients. Some did not want to participate and three had died, but many were doing better, the team found. Although differences between the two approaches had diminished over time, the early onset patients allocated to family therapy maintained a slightly higher weight and more regular menstrual periods than those who’d had individual treatment.
The Maudsley Method, named after the institution where it originated, was born. In Britain it’s known as Maudsley family therapy and in the U.S., where, with some minor differences, it was championed by Le Grange, as FBT. Forty years after its inception, FBT remains the leading evidence-based treatment for young people under 18.
The therapy has obvious advantages over alternatives such as hospitalization, practitioners say. For one, kids can stay in school and continue to live with their families, allowing for a more normal adolescence. There’s also much to be gained from giving parents a bigger role in their child’s recovery, said Renee Rienecke, who trained with Le Grange and is now the research director for the Eating Recovery Center and an adjunct professor at Northwestern University in Illinois: Parents “can really use the best weapon against the eating disorder, which is their love for their children.”
But with roughly 70 clinicians certified in family-based treatment, the U.S. is not in a position to provide FBT to the hundreds of thousands of teens with anorexia, experts say. And even when FBT works, the process is not easy — for kids, parents, or therapists.
Christina Olmsted decided to take temporary leave from her job as a marketing executive, and Kevin Olmsted quit his role at a wine company to become his daughter’s main carer. In 2020, he wrote a book about helping Tess recover, “Scared Dad Feeding” (an homage to the FBT classic, “Brave Girl Eating”). Kevin describes how under FBT his daughter was obliged to eat whatever he and his wife put on her plate. One of her parents sat with her during every meal and for an hour afterwards to make sure she didn’t purge what she had eaten or hide the food away. She ate five times a day — three meals and two snacks — and had to gain 1 to 2 pounds per week.
In family-based therapy, anorexia is viewed as an external threat, akin to a medical illness. Professionals do not try to explore what caused the illness, and above all, they must not suggest that it’s the parents’ fault.
Kevin went to elaborate lengths to boost her diet. He’d add an extra yolk to omelets, mix in two tablespoons of heavy whipped cream and an ounce and a half of Benecalorie, then fry the mixture in two tablespoons of butter. “Once I came to know that the demon of anorexia was a terrorist, who would stop at nothing to kill my daughter, who would know nothing of compromise or diplomacy, I then knew no amount of fighting dirty was off the table,” he wrote.
The Olmsteds shut the world out and disappeared for six months, something not every family is able to do. “It’s a luxury to treat this, just so we’re clear,” Kevin said to Undark. “Just to be able to swing at a pitch in this ballpark takes so many resources it’s ridiculous.”
The process was rough for Tess, who still recalls how it felt to be so closely monitored. Sometimes she would butt heads with her mother. She was too preoccupied with the illness to engage with her friends during senior year of high school and wasn’t able to play on the lacrosse team. “It was just a really difficult time,” she said.
Therapists can struggle, too. During the first phase of FBT, the clinician weighs the child at the start of each session. This practice, along with the need to offer dietary advice, makes some professionals uncomfortable. The family must also eat a meal together at the clinician’s office. “You have to be ready for anything,” said Rienecke, “for food being thrown across the room, for kids screaming and running out of the office. For a lot — a lot — of crying.” She continued, “oftentimes the kid just hates you at the beginning of treatment.”
In online discussions, young people sometimes vent their frustration with the approach. Family-based therapy “is the WORST” wrote one person on an eating disorder support forum. “I don’t understand how this could work,” the post continued. “When people control me and suffocate me, it triggers me tenfold.”
And sometimes parents’ desire to save — and control — their child goes too far, according to therapists and patients.
The 19-year-old from Texas said she began FBT in 2022. She had already been hospitalized once and relapsed while doing stints with different outpatient psychotherapists. She had experienced anorexia for four years and was almost 18, too old for family-based treatment. Nevertheless, her parents were able to sign up for a virtual program.
“Family-based therapy became more like family-based trauma,” the woman wrote on a Reddit forum for anonymously discussing eating disorders earlier this year. As her parents assumed the roles of dieticians and therapists, home started to feel like a hospital, she later told Undark. Her father was heavily involved in her care, even though she believes his earlier comments about her physical appearance had helped trigger her disorder. She said that during the therapy, her mental health deteriorated. She had thoughts of suicide and she started to self-harm.
What FBT failed to account for, the woman recently told Undark, is that for nearly five years, her eating disorder had actually given her some relief from difficult emotions. Her parents seemed to believe that weight regain alone would erase any feelings of depression and anxiety, she said. Weight gain is important, she acknowledged, but not without psychological healing.
Le Grange is aware that FBT has been carried too far by some parents but said it is fortunately rare. “Clinicians should always be on the lookout for a parent who takes a license to be critical and unkind to the young person.”
A survey by Australian researchers suggests that some parents also have doubts about FBT. In an interview, one father noted that the treatment’s focus was entirely on food. In his experience, however, his child’s restrictive eating was a symptom of a deeper problem. “What’s going on underneath?” he asked. “What’s causing all this?”
There are other criticisms, too. The therapy is “based on the idea that the young patient has no control,” said Riccardo Dalle Grave, who is head of a department of eating and weight disorders in Villa Garda Hospital in northern Italy. “The goal is to engage the parents, not the young patient. I was always in doubt about this.”
And yet some patients find that weight regain offers a path toward improved wellbeing. As Tess gained back weight, she was able to think more clearly. Eating an extra portion or a snack no longer felt like a catastrophe. “I really just figured out, such minor things didn’t mean as much as I used to think they did when I was younger,” she said.
Around the same time as the Maudsley Method emerged in London, researchers at Oxford University began working on a different model, focusing on adults. Cognitive behavioral therapy, or CBT, was developed in the 1970s by Aaron Beck, a researcher in Pennsylvania. It probes patients’ reactions to specific situations and posits that their interpretations of reality may be maladaptive or distorted. In the U.K., CBT has been approved for treating conditions ranging from childhood anxiety to adult schizophrenia, and it is recognized as clinically effective by the National Institute for Health and Care Excellence, the government approval body.
In 1981 Christopher Fairburn, a now-retired lecturer at Oxford, had shown CBT’s possible efficacy for bulimia. He applied it to anorexia, with results he described as “mixed.” Over time, Fairburn and his colleagues realized that anorexia tended to migrate. Patients might start out restricting food but then develop symptoms of bulimia, for example, if a patient’s psychological issues went unresolved. So they developed an approach that could work across different eating disorders, adding modules as necessary to target core problems like poor body image, perfectionism, or low self-esteem, and described this type of CBT as “enhanced.” In the U.K., CBT-E, as it’s known, is a second line treatment for teens, to be tried when family therapy fails.

Zafra Cooper is a professor of psychiatry at Yale School of Medicine and an emeritus professor of clinical psychology for the University of Oxford Department of Psychiatry.
Visual: Courtesy of Zafra Cooper
While cognitive therapy typically has a timeframe of 20 weeks, CBT-E can take longer, up to 40 weeks to allow for weight regain. Clinicians and patients may explore the pros and cons of the need for change. Patients may say things like, “‘I don’t know who I’ll be, I won’t have control,’ all those sorts of things — ‘I’ll lose my identity,’” said Cooper, who was recently given a Lifetime Achievement Award from the Academy of Eating Disorders.
CBT-E also has three phases, but it inverts their emphasis: The first phase involves helping patients think afresh about their condition and analyze the pros and cons of change. Only then are patients urged to address their eating habits. Under this model, parents are viewed as helpers, said Dalle Grave, the director of the eating disorder unit at Villa Garda Hospital.
Cara Lisette, who is 33 and lives in the U.K., suffered from anorexia for 20 years, cycling through hospitalization, in-patient care, and outpatient support. She first encountered CBT-E in 2011, but had no rapport with her therapist. When another clinician suggested CBT-E three years ago, Lisette decided to give it another try. This psychologist seemed to understand her better and was kind. Lisette said she was older and in a better position to be receptive.
Lisette describes how enhanced CBT was tailored to her illness. “Stuff like the body image distortions and things that people get when they have anorexia are quite unique,” she said. “I think it really takes into account just how people’s brains work a little bit differently when they have an eating disorder compared to something like anxiety disorder.”
While still finishing her own treatment, Lisette began her own training as a CBT therapist, and now uses cognitive therapy with children.
“I think it really takes into account just how people’s brains work a little bit differently when they have an eating disorder compared to something like anxiety disorder.”
Evidence for the effectiveness of CBT-E for young people with anorexia is based on just a couple of non-randomized studies. In 2013, Dalle Grave published an account of 46 young patients with a mean age of 15-and-a-half, aiming to see if they could complete the treatment as out-patients. Almost two-thirds did so and their weight increased substantially, with 13 teens reaching an almost normal weight. The authors saw the findings as making a compelling case for comparing CBT-E and FBT in randomized controlled trials.
In a non-randomized comparative study of 12-to-18-year-old patients, led by Le Grange and Dalle Grave that was published three years ago, FBT and CBT-E came out as just about equally effective.
Le Grange, Dalle Grave, and a Norwegian colleague are now collaborating on the first ever randomized-controlled trial comparing CBT-E and FBT for adolescents with eating disorders, based at Oslo University Hospital. Initial enrollments are in January next year but obtaining a full picture will take years, Le Grange said: “It’s going to be a while.”


“I’m seeing younger and younger and younger patients,” said Suzanne Straebler, a CBT-E eating disorder therapist providing therapy to people with anorexia. “These are babies, right? They are children, and here they are with full blown eating disorders.” In the past, she said, her clinic in New York would occasionally see an 11-year-old patient. Currently, the clinic is treating several 8-year-olds.
Researchers believe the Covid-19 pandemic and protracted school closures are the likely culprits, creating an uncertain environment, where everything seemed out of control. Isolated at home and unable to meaningfully engage with friends, teachers, and the wider society, vulnerable youth trained their focus on exercise and food intake, said Jessica Van Huysse, an assistant professor in the Department of Psychiatry at the University of Michigan. These conditions made it easier to carry out restrictive behaviors, she noted, “and then that’s a rabbit hole, right?”
“Eating disorders tend to thrive in secrecy,” Straebler observed. She is also concerned about the ability of social media to disseminate dieting fads to young people online.
While some children have been able to fully recover through CBT-E or FBT, the consensus is that more research is needed. “Our therapies are okay, they’re an option,” said Straebler, “but they’re not as good as they need to be. So we need more research, more funding.”
“These are babies, right? They are children, and here they are with full blown eating disorders.”
Additionally, clinical trials often enroll people with a single psychological disorder, Cooper said. But in the real world, patients may struggle with multiple conditions. Tess, for example, had a history of OCD and anxiety before she developed anorexia.
Neither FBT nor CBT-E, the researchers admit, is good enough, or sufficient on its own.
“I want to go on paper that I’m not an FBT evangelist. I’m a scientist,” said Le Grange. He estimates that in real world settings, FBT works for 60 to 65 percent of children. He asked: What can be done for those who aren’t helped?
Even those who do gain weight may continue to struggle, said Kevin Olmsted. He compared FBT to pulling a child from the mud and taking them to dry land. The therapy brings patients back to a stable weight where they’re healthy and safe. But they will still have plenty of psychological work to do.
Tess is now 18, and a full recovery remains elusive. In August, as she prepared for college, she noted that she’s in a much better place, but she struggles to balance her social life, schoolwork, and eating. Anorexia can fuel an all-or-nothing approach to life, which can be dangerous, she said: “It’s definitely still a battle — but it’s a different battle.”
If you are struggling with an eating disorder, call or text the National Eating Disorders Association at 1-800-931-2237.











I wonder if transcranial magnetic stimulation (TMS) has been studied as a treatment or might be effective. I believe it can help with OCD. Also, I think ketamine infusions might be studied in this area. In addition, just treating the symptom, the food restriction, without identifying the source(s) of the problem seems somewhat problematic to me.
I totally agree with your last statement (problematic without identifying the source), but I am skeptical about TMS. ECT was a complete waste if not a harmful treatment methodology.
Many of the treatments FBT, CBT, etc seem to me to be analogous to a slot machine gambler winning and then trying to suggest that their superstitious behaviors are really causes. ???