A New Approach to Stopping Ticks — With an Old Drug
It turns out that eating ivermectin is good for something after all. If you’re a deer, that is. And if the goal is to kill the ticks that are biting you — ticks that carry diseases that threaten humans.
The antiparasitic drug, which is mostly used on animals, gained a raucous following during the Covid pandemic after an early search for drugs that could be repurposed to fight it spotted some antiviral activity in a lab assay. But multiple randomized trials could never reproduce the effect in infected people — including a study published in February that followed more than 1,200 U.S. Covid patients for months. After overwhelming politically driven enthusiasm, ivermectin dwindled to a niche interest.
This story was originally published by WIRED and is reproduced here as part of the Climate Desk collaboration.
Now, a team of scientists working within the Connecticut state government has found a new application for something ivermectin was always good at: killing parasites that live in or on animals. In a small study, they found that feeding deer corn dosed with an ivermectin derivative builds up enough drug in their blood that ticks biting them will (probably) die.
This will be good news, if the finding holds up while the researchers expand the study into more, and larger, sites. That’s because drinking blood from deer is what gives adult female ticks the boost they need to lay thousands of eggs that will turn into more ticks — and because the combination of erupting deer populations and expanding tick ranges is driving an explosion of tick-borne diseases across the U.S.
Killing the ticks as they are taking their blood meal should prevent those eggs from being laid. And over time, if deer remain dosed at the right level, it could push down the number of ticks that live within a geographic area, reducing the long-term risks to humans.
That’s the thinking, anyway. There are a number of experimental steps still to go — and not everyone in the world of ticks is convinced it’s a practical approach.
“This was a proof-of-concept study,” says lead author Scott Williams, a wildlife ecologist and chief scientist at the Connecticut Agricultural Experiment Station in New Haven. “We wanted to see if deer would eat the corn coated with this product, and they did consume it. And we wanted to see what serum levels would be within the blood of the animals, and 83 percent were at or above the threshold of lethality.”
Before we go any further: This is not an argument for eating ivermectin to protect yourself against the 16 different diseases that ticks carry. Yes, ivermectin is approved for some human uses: It is used to cure parasitic diseases that mostly occur in low-income countries, such as river blindness and liver flukes. But it doesn’t work against viruses and bacteria in people’s systems, whether they are SARS-CoV-2 or the ones that ticks transmit. And while you hypothetically could consume enough of the drug to make yourself toxic to a tick, you’d be risking side effects without preventing infection — because the tick would inject the pathogens it carries before the ivermectin in your blood did anything to harm the tick. As the Food and Drug Administration posted on its Twitter account during the ivermectin craze: You are not a horse, you are not a cow. (The agency added: “Seriously, y’all.”)
Back to the study. The Connecticut group chose a site where they could monitor a small, contained deer herd: a peninsula jutting into Long Island Sound where the property surrounding a decommissioned power plant is returning to a wild state. They deployed a feeder that would regularly scatter a small amount of corn — enough to dope the animals, but not to fatten them up — and dosed the bait with moxidectin, a second-generation ivermectin that comes in a veterinary formula. Then, with the help of the wildlife-management nonprofit White Buffalo, they drugged and captured deer periodically through 2021 and 2022, tagging them, taking blood samples, and counting the ticks on their bodies.
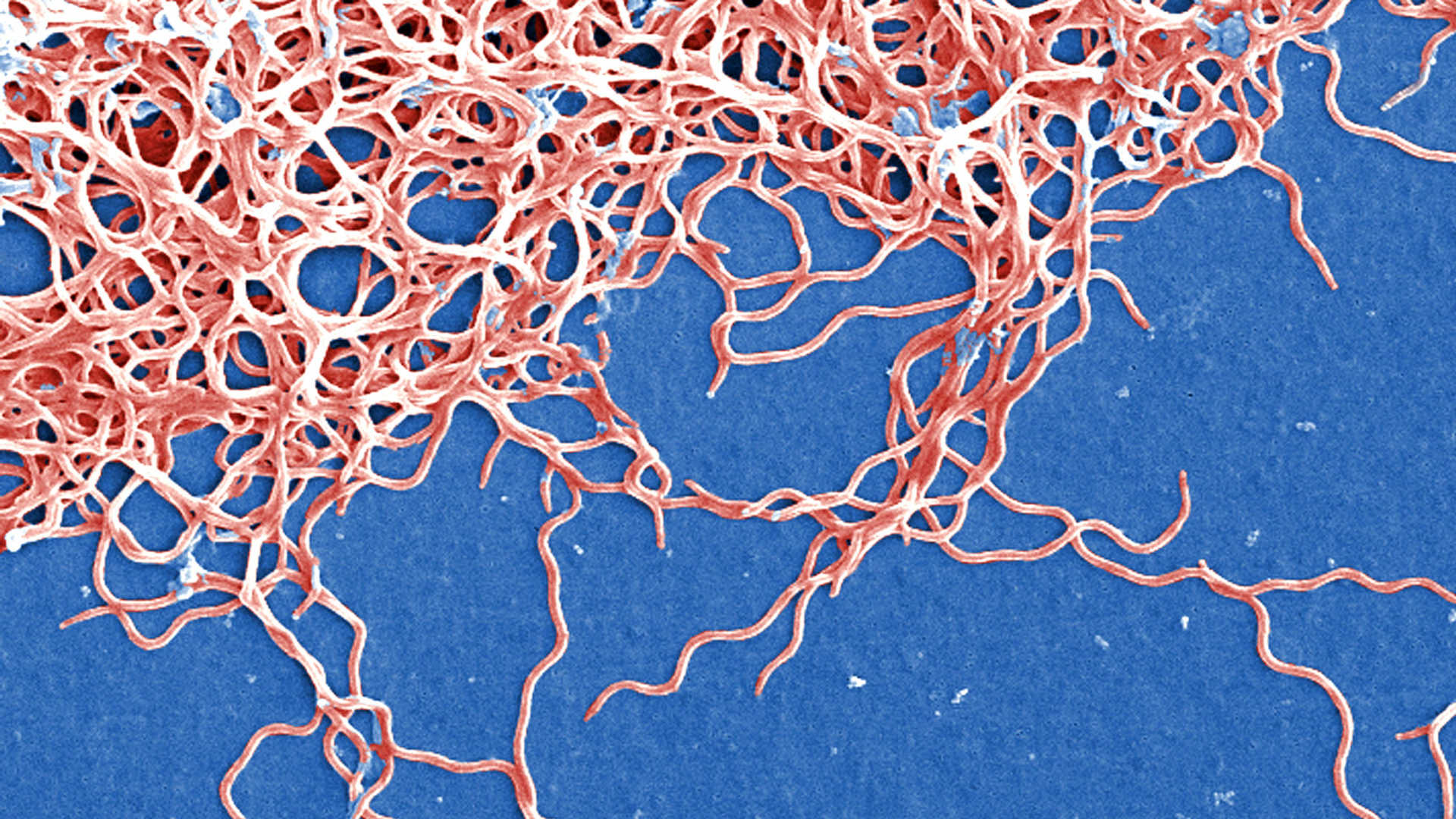
They focused on the lone star tick, Amblyomma americanum, which can transmit ehrlichiosis, borreliosis, Bourbon and Heartland viruses, and the meat allergy known as alpha-gal syndrome. That tick prefers to feed on white-tailed deer, while the type that spreads Lyme disease also preys on rodents. (For both species, humans are opportunistic targets. Ticks don’t have good eyesight, but they detect exhaled carbon dioxide — so when we blunder by them as they perch on vegetation, they sense us and attack.)
In this first study round, the researchers found that the number of ticks crawling on an individual deer did not change with blood levels of the drug — which makes sense, because the ticks wouldn’t know before biting whether a deer was dosed or not. However, the amount of latched-on, blood-engorged ticks declined as the level of the drug rose in a deer’s blood. “As the serum level increases, ticks don’t have to consume as much before they get paralyzed and fall off,” Williams says. “You wouldn’t see ticks engorged and feeding on animals with higher serum levels, because it would impact them much quicker.”
The work has attracted the interest of the Centers for Disease Control and Prevention, whose Division of Vector-Borne Diseases has given the group a five-year grant. “The preliminary work looked good at the proof-of-concept stage,” says Lars Eisen, a research entomologist in the Vector-Borne Diseases Division. “This is additional funding to do a larger-scale field trial in Connecticut, in an inland setting, and an island setting in Maine.”
The project contains complexities. A 1990s attempt to feed the original formulation of ivermectin to deer foundered on the multiple roles that deer play in the landscape. They are not only free-living wildlife, and not only suburban infringers, either charming or invasive depending on whether they pose in your garden or munch on it. They are also the much-desired target of sport hunters, who spend billions of dollars each year for access to them. Ivermectin carried a regulatory restriction, called a withdrawal period, that forbade consuming meat from a treated animal within 48 days. For hunters, that made the proposal a nonstarter.
That led to the best current method of tick control for deer, a device developed by the U.S. Department of Agriculture called a “4-Poster” for its loose resemblance to that style of bed. A four-poster holds a bin of treated corn, two integrated troughs that the corn falls into, and — this is the poster part — two upright paint rollers, saturated with tick-killing chemicals, on either side of either trough. To get to the corn, the deer have to shove their faces between the rollers. That paints their cheeks and ears with the chemicals, which eventually coat the rest of their bodies — a messy field version of the tick-killing solutions that dog and cat owners squirt onto their pets’ necks.
Four-posters seemed like a solution to hunters’ objections, because the chemicals stayed on the surface of the animals’ bodies. And because deer can transport ticks as they wander, the topical treatment offered the possibility of controlling ticks throughout an area or neighborhood. But scientific reviews have found mixed effectiveness, from huge reductions in ticks to not much impact at all. And in some areas, the devices are effectively illegal: Multiple states either discourage or formally ban group feeding to prevent chronic wasting disease — and now, Covid — from circulating through herds.
Plus, they’re labor-intensive and expensive to maintain. “The four-poster method requires dumping a bushel of corn into one of these devices every two weeks, and removing all of the not-eaten corn at the same time, because it gets moldy,” says Sam Telford III, a professor at Tufts University’s Cummings School of Veterinary Medicine with a career-long specialty in tick ecology. In one positive USDA trial, “they required one every six hectares [almost 15 acres] in order to be effective,” he adds. “That’s essentially a full-time person’s job, just to go around and service the four-posters.”
The new method solves the drug-residue problem because moxidectin, the newer version of ivermectin, has a zero-day withdrawal, at least when used in cattle. It retains the neighborhood-wide influence of the four-poster devices. And it may elide concerns about congregate feeding, because multiple deer aren’t sticking their faces into one device; instead, they’re grazing on grain sprayed over a radius of several yards. That also ought to prevent the dominant bucks from monopolizing the food source, and encourage more members of a herd to consume the drug.
Still, some tick experts have concerns. “It’s rather a blunt instrument,” says Rick Ostfeld, senior scientist at the Cary Institute of Ecosystem Studies in New York’s Hudson Valley. “You’re delivering a systemic antiparasitic drug, which will kill all kinds of internal parasites predominantly, while also doing some damage to the [external] parasites which are your actual target. And you’re delivering it by means of a method that broadcasts it, so non-target hosts consume it; they detected a bunch of species in their wildlife cameras. And we don’t really know how effective it might be.”
Ostfeld and his spouse and collaborator Felicia Keesing, a professor of biology at Bard College, recently concluded a multiyear study in 24 neighborhoods in Dutchess County, New York, to see whether novel means of tick control — bait boxes that administer topical chemicals to small rodents, coupled with sprays of fungal spores that kill ticks — could reduce the arachnids’ presence. (This was aimed at Lyme disease ticks, which feed on mice.) They were successful: Tick incidence in the area, measured by ticks on trapped mice and by complaints from residents, both dropped significantly. But in a just-published paper that reviews their own work and other studies, they open up a larger problem: Forcing down tick counts doesn’t appear to affect the occurrence of tick-borne disease.
It’s an example of how much has yet to be learned about the threats that ticks pose to humans — a field of inquiry that needs to rev up if it is going to keep pace with the wily creatures and the illnesses they cause. “Figuring out new, effective, and safe ways of killing ticks really is only a part of the story,” Ostfeld says. “We need to figure out why so far tick control has not resulted in human health protection.”
Maryn McKenna is a senior writer at WIRED covering health, public health and medicine, including the Covid pandemic, and a faculty member at Emory University’s Center for the Study of Human Health.