Why Singapore Is Breeding Millions of Mosquitoes
At Singapore’s National Environment Agency, more than a million mosquitoes buzz inside plastic boxes in a breeding room that smells of fermented sugar. The male insects, which don’t bite, feed on plant juices in the wild, but here, they nourish themselves on sugar water. Meanwhile, their female counterparts lay eggs on paper-like strips half submerged in trays of water. Each week, the insects inside this facility produce 24 million tiny black eggs.
The NEA’s mosquitoes are all Aedes aegypti, a species that can transmit viruses to humans, including dengue — a growing global threat which, by some estimates, infects 100 to 400 million and kills about 21,000 people each year. These captive insects are disease-free, however, and they are being bred to stop the spread of the viral illness. Specifically, the insects in the NEA lab have been infected with a bacterium called Wolbachia, which they will pass on to the next generation of mosquitoes.
The Wolbachia bacterium is ubiquitous in nature: It can be found in as many as 60 percent of insect species, from butterflies and wasps, to bees, dragonflies, and some species of mosquito. However, these bacteria do not naturally occur in Aedes aegypti. When scientists infect Aedes aegypti with Wolbachia, the insects no longer transmit dengue readily to humans. Additionally, under some circumstances, the bacterium can interfere with mosquitoes’ ability to reproduce. (The precise mechanisms behind these changes are not fully understood.)
Wolbachia-based protocols for insect control have been used in countries across the globe for more than a decade, and in many cases, they have reduced the incidence of mosquito-related disease. But scientists are still learning the best ways to employ these methods at scale. Wolbachia-infected insects are difficult to mass produce, and NEA’s researchers have responded by automating some of the steps that were previously done by hand. Even so, it would be tough to cover “the billions of people, living in the 10,000s of towns and cities in more than 100 countries, that are at risk of dengue,” Jérémie Gilles, the director of production development and supply at the not-for-profit World Mosquito Program, said in an emailed response to Undark.
The WMP and other research organizations use an alternative Wolbachia-based approach — one that doesn’t require such large numbers of lab-bred insects. Thus far, the approach has been effective and cost-efficient, though more time is needed to monitor the long-term outcomes, including the possibility that dengue may evolve to evade the bacterium.

Despite the challenges, officials in Singapore have been game to try Wolbachia to fight dengue — a common scourge in this densely-populated city-state that offers a perfect breeding ground for Aedes aegypti, which favor urban environments and warm climates. Singapore’s National Environment Agency has fought the virus for decades: spraying insecticides, advising people to avoid getting bitten, providing detailed instructions for preventing mosquitoes from reproducing inside one’s home, and fining those who fail to comply. Yet all these efforts are like chasing a runaway train, experts say, which is why the government turned to Wolbachia.
Since 2016, NEA scientists have been setting free male Wolbachia-carrying mosquitoes around Singapore. Though the program started small, by 2019, the NEA was releasing up to 2 million insects per week. Thanks to automation, that number increased to as many as 5 million per week in 2022. So far, at intervention sites, this has led to dramatic reductions of wild Aedes aegypti populations — and far less dengue.
Once the insects have laid their eggs in the mosquito breeding room, the NEA researchers move the millions of tiny black dots down the hall to a hatchery — a bright, hot, humid place that stinks of fish. The eggs are placed in small, water-filled trays, waiting to hatch into larvae.
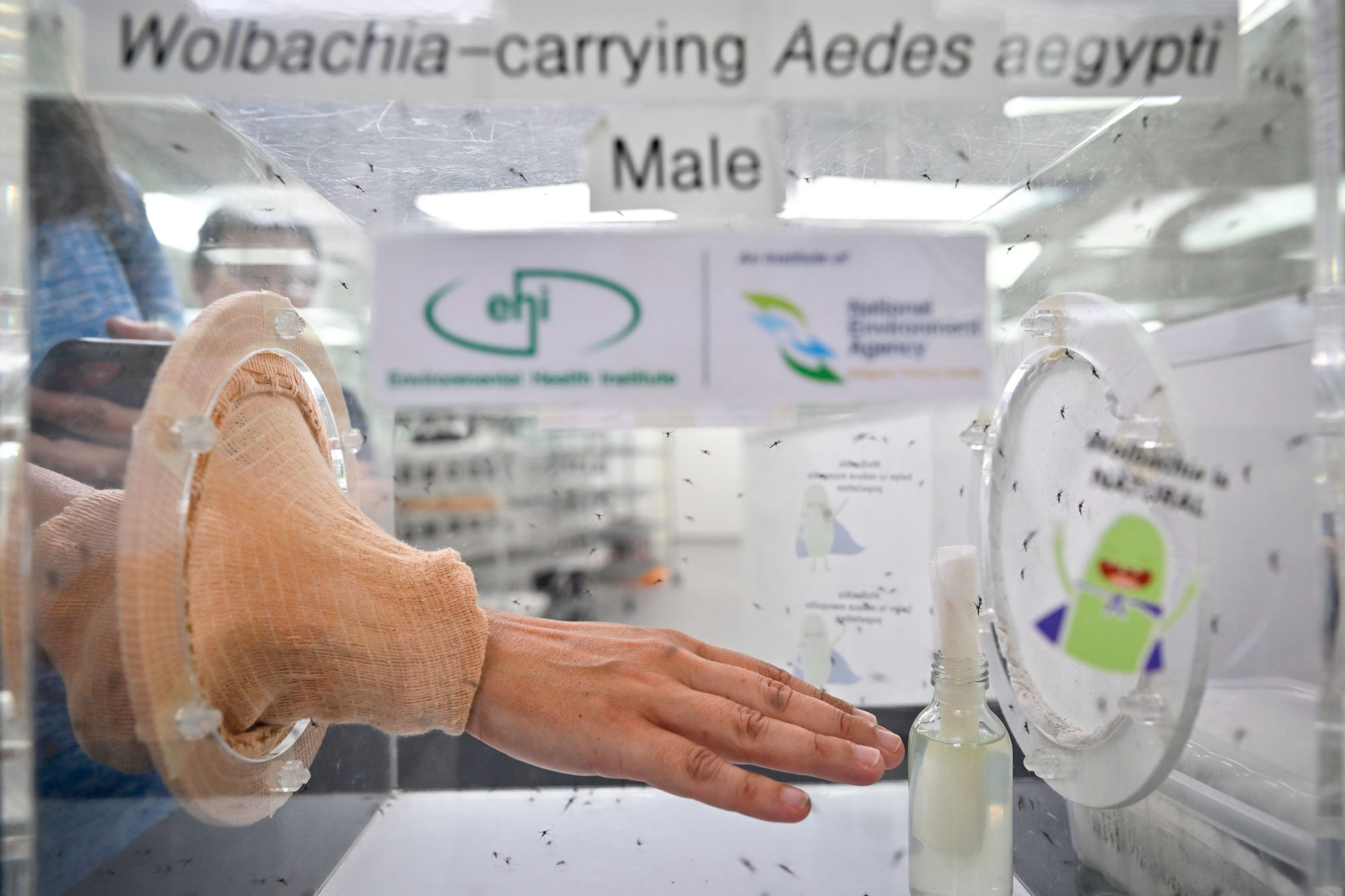
By releasing male Wolbachia-infected mosquitoes into the community, Singapore is following a protocol that aims to suppress the population of native mosquitoes. When such males mate with local Wolbachia-free females, the females lay eggs that won’t hatch, and in time the number of mosquitoes decreases. This suppression method is tricky. As it happens — and for reasons that are not well understood — mosquitoes can successfully breed when both partners are infected with Wolbachia. To prevent this, NEA scientists separate the females from the males before the latter are released.
But first, the larvae need to be counted and transferred to a rack with larger trays, each holding precisely 26,000 larvae. The exact number is important for keeping the rearing conditions constant, and initially, NEA staff would manually count all the hatched larvae. It took a sharp-sighted lab assistant two hours to count just 4,000 larvae, said the NEA’s senior research officer, Deng Lu. Now, the tally is automated: Pour millions of larvae into a machine, and within minutes it will count the 26,000 needed to fill one tray.
Once in their new, larger trays, the larvae are kept at a water temperature of 80 degrees Fahrenheit and fed a customized mixture of fish meal, carbohydrates, and fats (hence the smell). In nature, male pupae are generally smaller than females, but the difference is not large and it can be hard to distinguish males from females. To solve this issue and make separation by sex a bit easier, NEA scientists have perfected the larvae-rearing process. The diet, the temperature, and the humidity have to be kept perfectly constant, Deng said, to ensure that the females and males end up as different in size as possible.

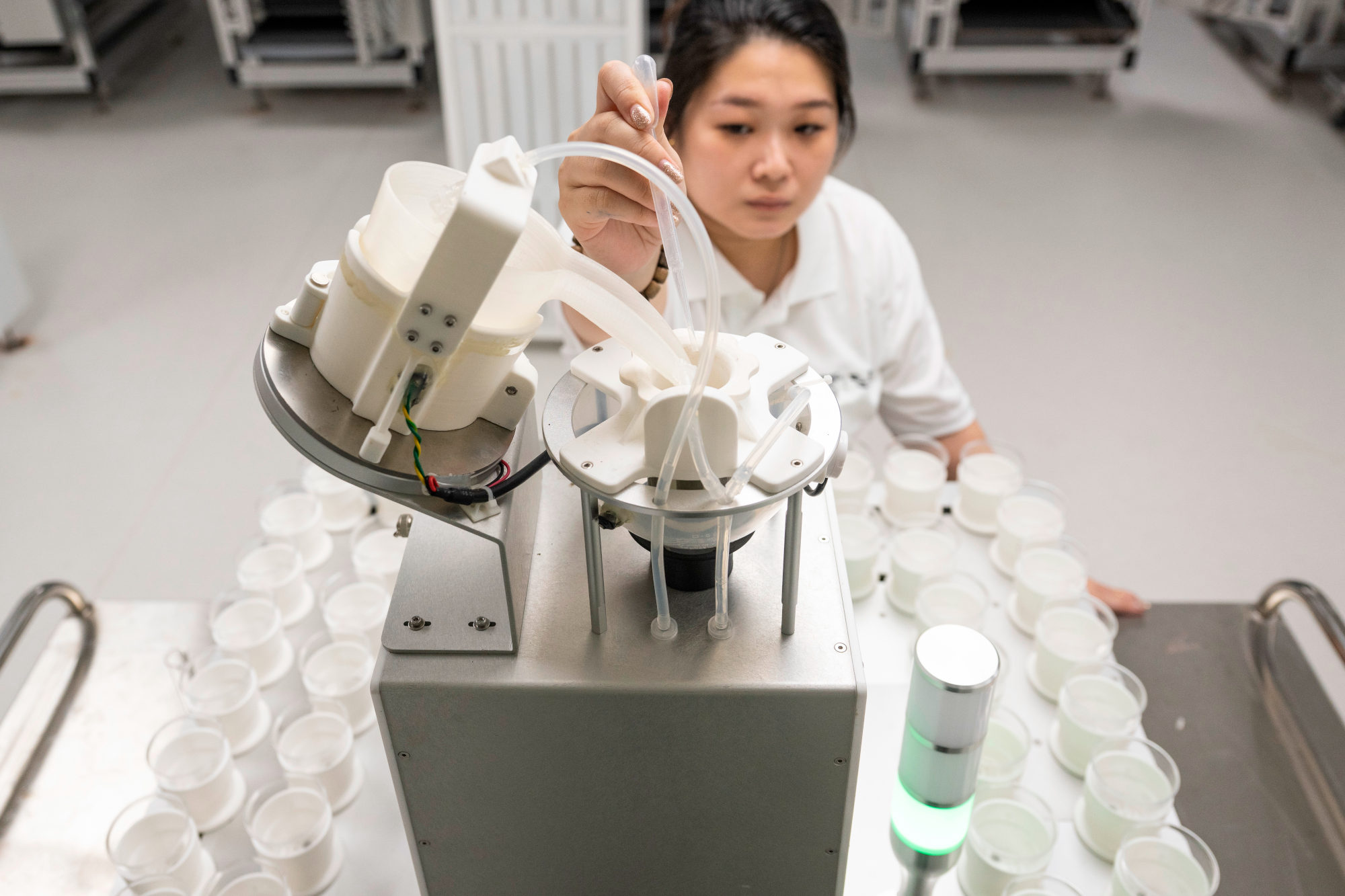



Separating male from female pupae also used to be done by hand, a job that was both tedious and prone to error. Now, however, NEA scientists are helped by another new technology: the pupae sex sorter. Here, the process starts with scanning a batch of pupae — basically, taking pictures of each individual and gathering its measurements. An AI-based computer system will then draw a type of graph called a distribution curve. If everything up to now has been done correctly, the graph on the screen will show two clearly separated peaks: a small upward curve indicating males to the left and then another, larger bump, indicating females, to the right.
Scientists can calculate the male-female size differential in a particular mosquito batch by measuring the distance between the two peaks. “In this batch, the male and female distance is about 200 microns,” Deng said. “So we actually can do the female separation.” Based on that 200-micron distance, he picked up a sieve that would only let the smaller pupae through and inserted it into the sorter, a white machine shaped like a mini-fridge. After the pupae are poured in, the females will stay on the sieve while the males pass through into a container underneath. The whole process takes about 10 to 12 minutes.
Singapore is not the only country that fights dengue by releasing Wolbachia-infected male mosquitoes. A facility run by Verily Life Sciences — formerly Google Life Sciences — which bred mosquitoes for release in a trial in Fresno, California, can produce close to 3 million males per week, also with the help of AI and automation. The world’s largest mosquito factory in Guangzhou, China, can churn out even 10 times as much.
Automation and AI may have allowed some laboratories to produce huge batches of mosquitoes, but these tools are not cheap. (The NEA would not divulge its budget.) This is one reason why many efforts use a different Wolbachia-based method, known as population replacement, which does not require sex sorting and can work with fewer factory-bred mosquitoes. This method aims to replace native populations with one that is unable to transmit dengue.
Scientists begin by infecting both male and female mosquitoes with Wolbachia. For reasons that are so far unclear to scientists, the bacterium impairs females’ ability to transmit certain viruses, dengue included. A non-randomized study conducted in Yogyakarta City, Indonesia, showed that two years after initiating a population-replacement protocol, dengue incidence in the intervention area fell by 73 percent compared to a control area. A similar study conducted in Brazil showed a 69 percent reduction in dengue incidence and a 56 percent reduction in cases of another virus called chikungunya.
Though male mosquitoes do not bite — and therefore can’t spread dengue — it’s still important to infect them with Wolbachia and release them along with the infected females. When Wolbachia males mate with wild infection-free females, the eggs will not hatch, and over time, there are fewer infection-free females to compete with their lab-produced counterparts. At the same time, as the Wolbachia females mate with both wild and lab-bred males, the eggs will hatch and the offspring will carry Wolbachia. The hope is that ultimately the native Aedes aegypti mosquito population will be made up of individuals infected with the bacterium.
This makes the approach simpler than Singapore’s because there’s no need for sex sorting.
Additionally, population replacement requires considerably fewer lab-grown mosquitoes. “The aim is to get Wolbachia to spread into that population rather than to suppress it, and so the numbers of mosquitoes that need to be released are an order of magnitude lower than with a male-only suppression program,” said Steven Sinkins, a professor of microbiology and tropical medicine at University of Glasgow.
In the Yogyakarta City study, only 1.7 million mosquitoes were released over a 7-month period — compared to Singapore’s 5 million per week. This makes the method more affordable. “Where the budget is restricted, the health budget, we would definitely be recommending the replacement approach because of the smaller scale of releases needed,” Sinkins said.
What also potentially makes the replacement method easier to employ is that it’s designed to be self-sustaining. “If you’ve done it correctly, it will be a discreet period of releases and then you can stop. The Wolbachia will be at a high stable frequency and it will stay there and block dengue transmission long term,” Sinkins said. In Australia, where Wolbachia-mosquito releases to fight dengue were conducted in 2011, the first replacement project in the world, the bacterium was still stable in the Aedes aegypti population nine years later.
The simplicity and affordability of the replacement method is one reason why it was chosen by the World Mosquito Program, which has launched Wolbachia programs in 12 countries, from Brazil and Mexico to Vietnam and Australia. “We aim to simplify our production process as much as possible,” Gilles wrote in an email. “We try to minimize automation throughout our program.”
Why did Singapore choose the suppression method, then? One reason, according to Ng Lee Ching, director of NEA’s Environmental Health Institute, is the issue of bites. To replace a mosquito population, researchers need to release those pesky females. “Our people are not used — not comfortable with mosquito bites, so I think the public acceptance for the replacement approach would not be as high,” she said. After decades of various mosquito control programs on the island, there simply aren’t many mosquitoes flying around Singapore anymore. And for reasons that will be obvious to anyone who has ever been swarmed, local residents are not keen to bring the insects back.
On a November morning, Matthew Verkaik arrived in the Singaporean town of Yishun to release about 4,400 lab-reared male Aedes aegypti. Yishun used to be a dengue hotspot, brimming with mosquitoes. Now, after six years of releases, the local Aedes aegypti population is down by as much as 98 percent, and dengue cases are down by 88 percent. “The before and after is very startling,” said Verkaik, a senior research officer at the National Environment Agency. “You don’t pay attention until you are like, ‘Okay, wait. There’s no mosquitoes. What’s going on?’”
He picked up a basket containing 22 black canisters, each filled with about 200 Wolbachia-infected males, and walked to the first release spot located at the back of a 12-floor apartment block. The place was not random — Verkaik chooses these spots carefully. In general, he freed about six mosquitoes per inhabitant, and did so at even intervals alongside the buildings, both on the ground floor and on higher ones, too.
Standing by the building’s trash chutes, Verkaik grabbed a canister, opened the lid, and gave it a shake. The insects emerged as a cloud of tiny black shapes. A few open containers later and the mosquitoes were everywhere: buzzing around, sitting on walls. In general, the locals seemed not to mind, as the program has strong community support. In a 2021 study, 92 percent of households reported no concerns with releases in their neighborhoods.




According to Sinkins, replacement projects also tend to be welcomed by the public, biting females notwithstanding. “I think mainly because we’ve been targeting areas that have high dengue transmission rates,” he said. “The community acceptance has been very good because nothing else has really been working.”
Reducing mosquito bites, however, is not the only reason why Singapore chose the suppression method over population replacement. The other one is the potential risk of viral evolution, Ng said. Just like Covid-19, dengue is caused by an RNA virus that can evolve relatively quickly. Replacement areas still have a lot of mosquitoes, and there is always the risk of sporadic dengue infections occurring in a small number of the insects. Such breakthrough infections might provide opportunities for dengue viruses to evolve and adapt to the bacterium.
Virus evolution is something that concerns some experts. “It’s a risk, ” said Kat Edenborough, a microbiology research fellow at Monash University in Australia, the institution that owns the World Mosquito Program. “It’s something that we’ll be actively surveying.” She noted, however, that unlike SARS-CoV-2, which can evolve as it spreads person-to-person, dengue needs two species to serve as hosts: the mosquito and the human. This, according to Edenborough, should slow down the viral evolution. A recent study in which researchers passed the dengue virus 10 times through Wolbachia-infected cells of Aedes aegypti did not show signs of the virus adapting.
While Wolbachia programs have gained momentum over the last few years, there is still a lot of ground to cover. Scientists want to understand how exactly Wolbachia works inside mosquitoes, how it evolves, and whether it pushes viruses to fight back. And researchers want to find out if Wolbachia can help fight other diseases, such as malaria. (There are some indications that it might.) The World Health Organization has set a goal to lower the incidence of dengue by 2030 by 60 percent compared to 2016 numbers. “To get to that point,” Edenborough said, “we need to just be using everything that we can.”
UPDATE: A previous version of this piece incorrectly stated that the male mosquitoes at Singapore’s National Environment Agency are infected with Wolbachia after they are sorted from the female mosquitoes. In fact, the males are infected with the bacteria prior to this sorting. The story has been corrected.
Marta Zaraska is a Polish-Canadian science journalist. Her work has appeared in the Washington Post, Scientific American, New Scientist, The Atlantic, and Discover, among others.
Caroline Chia is an award-winning commercial and editorial photographer based in Singapore.