Malaria Prevention Pushes Forward in Africa Despite Pandemic
On April 23, as lockdowns and Covid-19 cases spread, the World Health Organization warned that one of sub-Saharan Africa’s biggest killers was still at large.
Malaria killed 384,000 people in Africa in 2019. That number could double, warned two modeling studies — one first released by WHO-affiliated scientists in April, and a second by scientists at Imperial College London in August — if the pandemic were allowed to disrupt the continent’s ongoing malaria control efforts.
The WHO highlighted the worst-case scenarios as it called on nations and nongovernmental organizations to continue essential malaria prevention initiatives, including making malaria-preventive medicines available, distributing insecticide-treated bed nets, and spraying the walls of people’s homes. Researchers also emphasized the importance of outreach so that patients with malaria would not avoid visiting health care facilities during the pandemic.
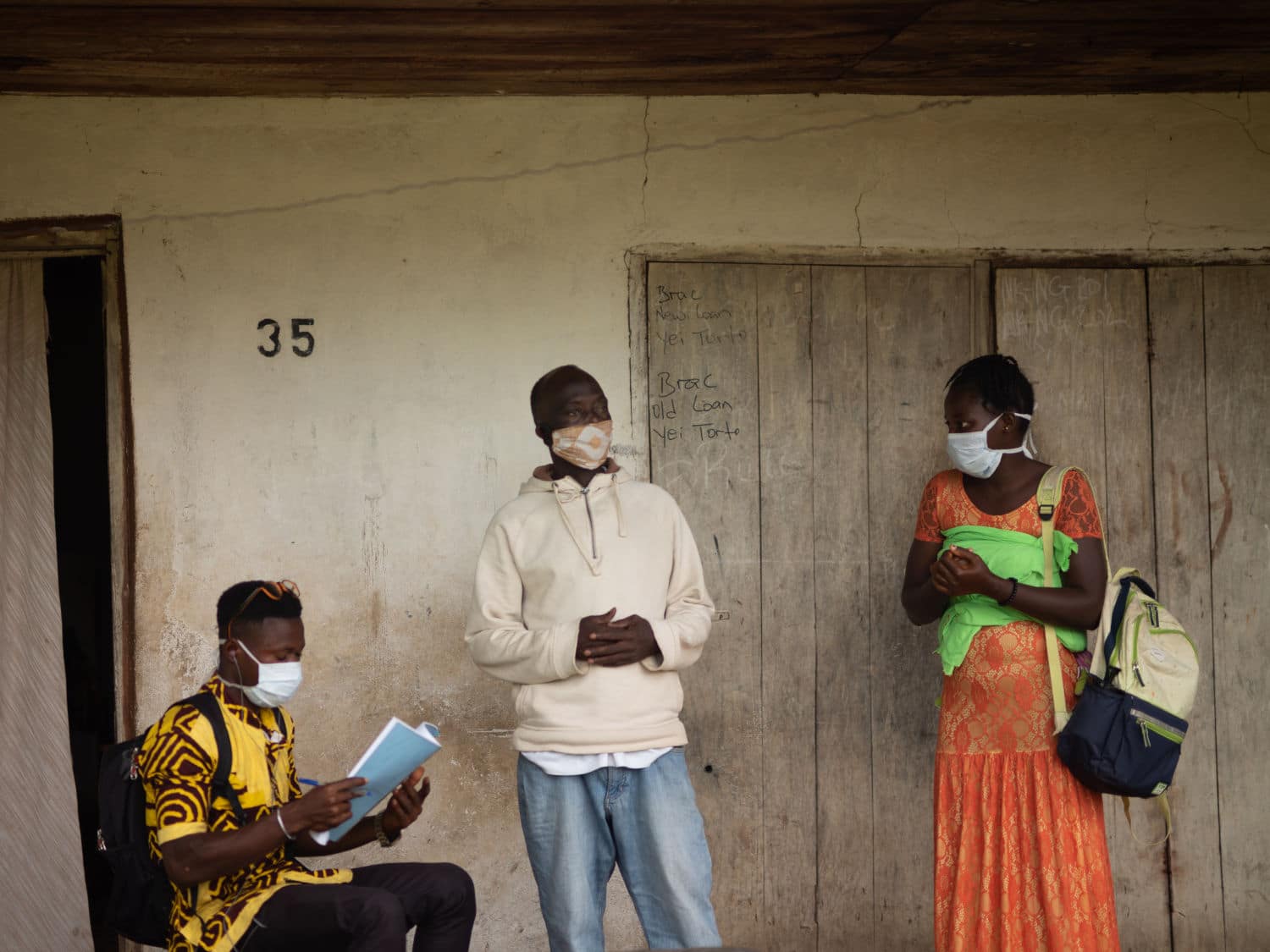
In response, the international public health community has been shifting its tactics, sending aid workers door-to-door to deliver bed nets and accurate information about Covid-19. Perhaps most importantly, health organizations are tackling the mundane issues of manufacturing and shipping logistics to ensure that necessary supplies remain available.

According to the WHO’s 2020 World Malaria Report, which published at the end of November and included a special chapter on malaria and the Covid-19 pandemic, the quick implementation of these efforts may have prevented the worst-case scenarios from materializing. “It’s just been a really good example of a determined set of partners figuring out how to manage through this challenge using a combination of innovation, flexibility, pragmatism,” said David McGuire, who directs the access program for the Innovative Vector Control Consortium (IVCC), a not-for-profit involved in managing the market dynamics of insecticide-treated nets. “The situation is not quite as bad as we had feared.”
But the Covid-19 pandemic will still leave a mark when it comes to malaria. While the worst of the model predictions may not unfold, Africa is still likely to see an increase in malaria deaths according to the RBM Partnership to End Malaria, a group with more than 500 partners including the WHO. Pedro Alonso, director of the WHO’s Global Malaria Program, said in a November press conference that while supply deliveries have been successful, the effect of the slowed pace of medical care is still unclear and could be considerable, especially for children under 5 who account for 67 percent of malaria deaths worldwide. Malaria prevention efforts in Africa are mostly driven by global health organizations headquartered in Europe and the U.S., with much of the on-the-ground implementation carried out by African health care workers.
“At the beginning of 2020, malaria deaths were at the lowest point ever, culminating two decades of global commitment and action that put the world on a path to end malaria,” a spokesperson for the RBM Partnership to End Malaria wrote in a statement to Undark. “By spreading to all corners of the globe, Covid-19 presented a major threat to millions of families at risk of malaria, fragile health systems in malaria-affected-countries, and decades of progress against the disease.”
Malaria is caused by a parasite spread by the female Anopheles mosquito. When the insect bites an infected human — one who already has the parasite circling in their bloodstream from a previous mosquito bite — it becomes infected itself and can continue the cycle by delivering a bite to another person. “When you have a population of people with malaria, the more people who have malaria, the more chance there is that a mosquito can become infected,” said Ellie Sherrard-Smith, an epidemiologist, parasitologist, and mathematical modeler who helped lead the modeling efforts at Imperial College London. The group published their results in Nature Medicine.
Controlling the spread of the disease requires multiple tactics, including chemoprevention, where children are treated with preventative malaria drugs during the rainy season when the mosquito populations are at their peak. As these mosquitoes are most active at night, insecticide-treated bed nets are also distributed to protect people while they sleep. Indoor residual spraying involves treating the inside of people’s homes with an insecticide that remains there for several months; when a mosquito rests on one of the walls after feeding, the chemicals kill it. Treating malaria patients is another important prevention tactic; mosquitoes can’t pass on the parasite from people who no longer have it.
The Imperial College London study explored the effects of these malaria-fighting measures through two models. The first was an already-validated malaria transmission model developed in 2010. The second was a Covid-19 model that included four different pandemic scenarios, which ranged from widespread, concerted efforts to stop the spread of the virus to no coordinated public health response at all.
The WHO’s analysis, which was formally published in The Lancet Infectious Diseases in September, took a different approach. Global Malaria Program researchers collaborated with researchers from the Malaria Atlas Project at the University of Oxford and elsewhere to map how sub-Saharan Africa would fare with decreased insecticide-treated net coverage and lowered access to malaria treatment. The most optimistic of the researchers’ scenarios — a 25 percent reduction in insecticide-treated net distributions — still showed an increase of more than 25,000 deaths from the baseline. The most pessimistic scenario estimated more than 380,000 additional deaths.
Health care workers at Koidu Government Hospital, the only hospital in Sierra Leone’s rural Kono District, and the Wellbody Clinic, one of its few primary care clinics, began to see the effects of the Covid-19 pandemic almost immediately. When the country’s first lockdown was implemented in April, visits plummeted. “We saw immediately a sharp decline, almost a halving of the number of patients,” said Jourdan McGinn, former director of policy and partnerships in Sierra Leone for Partners in Health, a Boston-based nonprofit that assists at the hospital and runs the clinic. (McGinn is now the organization’s deputy executive director.) Overall, they saw a 21 percent drop in outpatient visits and a 46 percent drop in children’s primary care visits compared to the previous year.
McGinn says that many of the children who were brought in for malaria treatment were in much worse condition than they would have been before the pandemic. Koidu Government Hospital has actually seen a decrease in childhood malaria deaths, but McGinn suggested these data — rather than being reassuring — could point to a tragic trend.
“The reason for that is not that kids aren’t dying, it’s just that they’re not coming to the hospital,” she said. “They’re dying in their communities because they never reached the facility in the first place.”

The Covid-19 pandemic has brought unwelcome memories of the Ebola outbreak that devastated the country in 2014 and 2015. During that epidemic, more people died due to reductions in treatment of tuberculosis, HIV, and malaria than from the Ebola virus itself. The WHO’s Alonso warned in the November press conference that the same could be true again — the increase in malaria deaths brought on by the pandemic have the potential to eclipse Covid-19 deaths in sub-Saharan Africa.
Now, most patients who come to the hospital or clinic are screened for both malaria and Covid-19. (In a typical year, 30 percent of patients have malaria as their primary diagnosis, according to McGinn.) Partners in Health and government officials are using lessons learned during the Ebola outbreak to combat misinformation and to make sure patients still get necessary care for illnesses other than Covid-19.
“Barriers to care are more pronounced during outbreaks because things like transport is less available or there’s lockdowns,” said McGinn. “Or, people have less money because they earn daily wages to afford the fees to pay the motorcycle to get to the facility.”
To ensure that information about seeking health care during the pandemic would get out despite these challenges, Partners in Health hired 125 people to go door-to-door and reach out to community members. The strategy seems to be working. McGinn said that while patient numbers at the hospital haven’t completely returned to normal, they are much closer to what the facility would usually expect to see at this time of year.
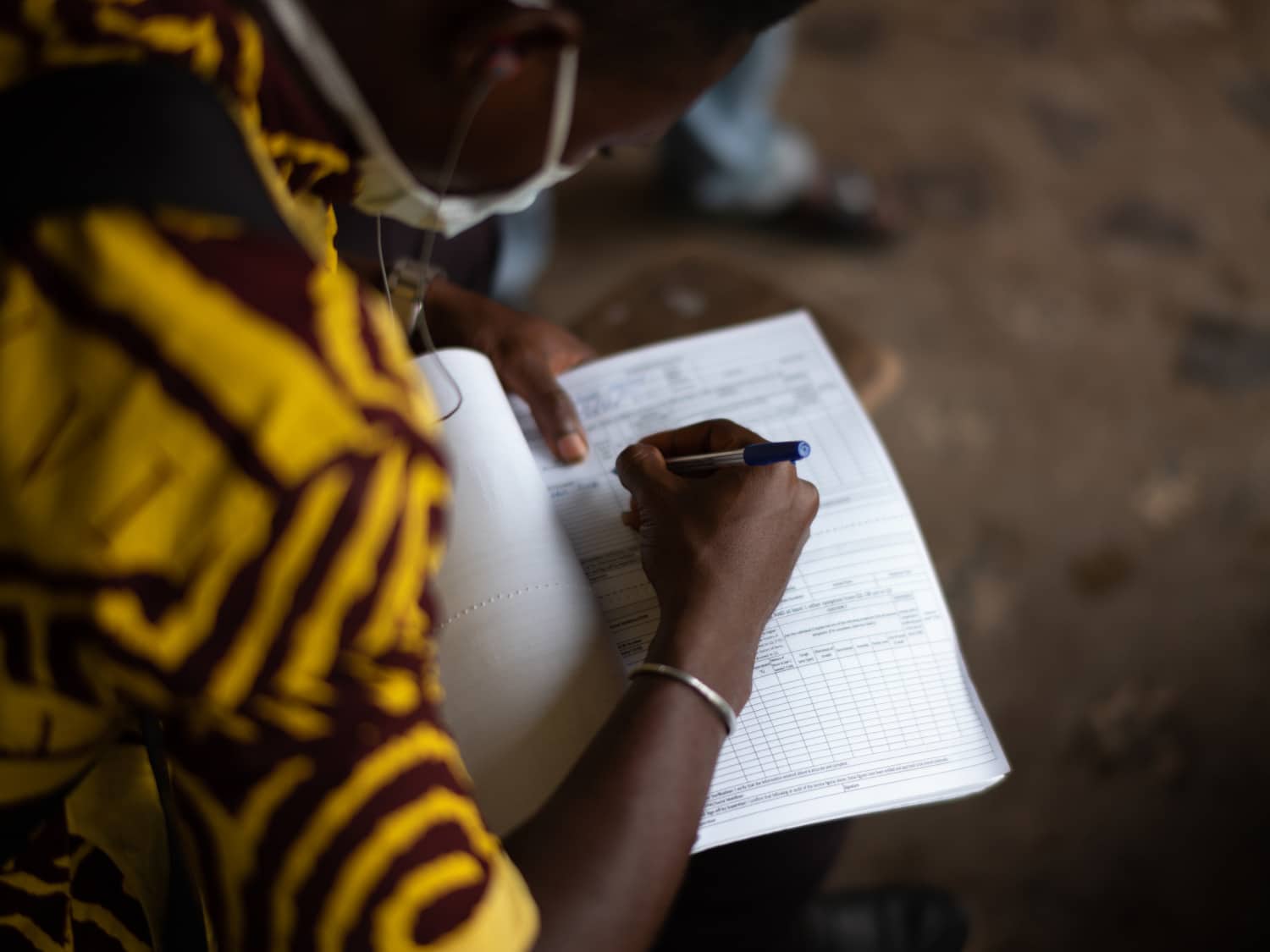

As the pandemic progresses, McGinn said that a major concern is ensuring that supplies remain available. Early in the pandemic, when much of the world was focused on ramping up Covid-19 testing capacity, malaria test kits were also in short supply due to lockdown-related disruptions to the global supply chain.
“A key component is making sure that we literally have the medication and the test kits and that we didn’t burn through the stock that was in-country,” she added. “Delays in the delivery of new items would mean we’d have stock-outs.”
Multiple organizations are working hard to prevent those shortages from materializing. For example, Pierre Hugo, who helps manage malaria drug supply chains for Medicines for Malaria Venture (MMV), a Switzerland-based not-for-profit, confirmed that they were on track to deliver chemoprevention drugs this year in spite of logistical problems caused by the pandemic, both on and off the continent.
“We’re talking huge numbers — nearly a hundred million courses of seasonal malaria chemoprevention drug,” said Hugo, referring to the 2019 delivery of SPAQ-CO (sulfadoxine pyrimethamine and amodiaquine), which reached roughly 24 million children in the countries of the Sahel region, the transition zone between the Sahara Desert to the north and the savannas to the south. The group had planned to expand capacity to deliver 120 million courses of the drug in 2020, but only roughly 100 million will be delivered due to funding issues unrelated to the pandemic.
According to Hugo, some groups have been forced to take drastic measures when it has become clear that necessary supplies for illnesses other than Covid-19 might not arrive in time.
“You’ve got the absolute extremes. You’ve seen the likes of the Global Fund or others actually chartering jumbo jets,” he said, describing how some organizations have stocked entire cargo planes with life-saving medications and other supplies.
But averting disaster has also involved far less cinematic acts of heroism. “The role MMV has played, specifically, is to reduce risk by diversifying supply,” said Hugo. Among other efforts, the not-for-profit worked to bring aboard a second manufacturer of artesunate, an injectable drug used to treat severe cases of malaria, so that supplies of the vital treatment would remain available.
“These are end-stage patients — if they don’t get something, they’ll die,” said Hugo. “The last situation you want to be in is to have a single-source supplier.” The group has also worked to find a second manufacturer for SPAQ-CO, ensuring that enough doses will be available for next year’s seasonal chemoprevention campaign, too. Efforts are ongoing to fine-tune supply chain monitoring tools so that drug distribution or manufacturing bottlenecks don’t happen if lockdowns return or if demand spikes.
As with medications, supply chain interruptions to insecticide-treated bed nets could have had devastating consequences.
“Everyone kind of agreed, we have to get these nets out there,” said McGuire of the Innovative Vector Control Consortium. “We can’t deprive people of malaria prevention tools.” With funding from Unitaid and the Global Fund, the IVCC is leading the New Nets Project, a trial designed to assess the effectiveness of next-generation nets that use a combination of insecticides to combat insect resistance. Though there were delays in delivery of the new nets, the scheduled deliveries were eventually carried out, including 1.1 million to Rwanda and 960,000 to Mali.
Typically, the most efficient way to deliver supplies would be for people to come to a centralized location to pick them up. Realizing the danger of drawing crowds during the pandemic, however, officials used a similar strategy to the Partners in Health outreach campaign and delivered nets directly to people’s doors, according to McGuire.

Although the data are still being processed to assess exactly how specific countries have been affected, early reports seem promising. According to the RBM Partnership to End Malaria, more than 90 percent of global malaria prevention initiatives have gone forward. The organization recently reported that over 200 million insecticide-treated nets were on track for delivery this year. However, only 105 million of the 222 million nets expected to be distributed in 2020 had been delivered by Nov. 23 according to the recently published World Malaria Report.
The WHO also reported that as the pandemic has progressed, 23 of the 47 countries with indoor residual spraying initiatives planned for 2020 had been able to complete their efforts, with another 13 on track to finish spraying by the end of the year. This technique, which is used less widely than other prevention strategies, had already decreased in coverage from 5 percent in 2010 to 2 percent in 2018. In South Africa’s Limpopo Province, officials have reported extending the spraying season in an attempt to mitigate staff shortages that resulted from the Covid-19 pandemic. In Uganda, spraying initiatives were cancelled this year.
“It’s hard to know the extent which Covid-19 will affect malaria eradication efforts; however, as a community we are striving to ensure our progress is not lost,” the RBM Partnership spokesperson wrote to Undark. Although the WHO’s 2020 World Malaria Report provided updated information on how the pandemic has affected to fight to eradicate malaria, it may be years before the true impacts become clear.
“Malaria cases and deaths are still likely to increase this year and next year,” the RBM Partnership statement said. “Therefore, we must sustain the level of urgency to ensure countries can stay on track to deliver planned and ongoing malaria campaigns in 2021.”
Ashley Stumvoll is Durham, North Carolina-based freelance journalist who is trained in ecology. She writes on issues at the intersection of people and the planet.