Autopsy Rates Were Falling for Years. Then Covid-19 Came Along.
N ormally, when James Stone, a pathologist at Massachusetts General Hospital, does autopsies, he has an audience — a dozen or so students, pathology fellows, assistants, and even attending physicians, hoping to learn from his work. But since the Covid-19 pandemic began, Stone has done autopsies on Covid-19 victims with just one or two other colleagues in the room. Instead of the usual gloves, mask, goggles, apron and other gear that pathologists don during autopsies, he wears what he calls “full-hazmat-style gear” as he makes a Y-shaped incision in the deceased patient’s body, slicing from each shoulder toward the sternum and then straight down to the belly button. Stone or a technician then peels back the skin, ribs, and chest plate to see the organs inside.
Sometimes, Stone can tell organs are damaged just by looking at them. But the most useful insights come when he places pieces of tissue under the microscope, searching for the effects of Covid-19.
In past generations, Stone would have had more colleagues in other hospitals investigating the consequences of a mysterious new virus. But these days, his setup is less common. After years of nationwide cuts, Massachusetts General is one of a limited number of hospitals left in the U.S. that has its own dedicated autopsy suite. And, early in the pandemic, Stone was one of the few pathologists willing to risk performing autopsies on Covid-19 patients amid concerns that doing so would transmit SARS-CoV-2, the virus that causes the disease.
Still, Stone and other pathologists willing and able to examine Covid-19 victims have made discoveries that may lead to better treatments for current patients. In the process, their work has helped illuminate the effects of a sometimes mystifying virus — even as it highlights longstanding declines in autopsy rates.
Indeed, since 1950, pathologists in the U.S. have gone from conducting autopsies on nearly half of all patients who died in hospitals to less than 5 percent of them. In part, that’s because advances in imaging technology have given physicians more confidence in their diagnoses. But “our ability to determine the cause of death is pretty bad unless you do an autopsy,” says Mary Fowkes, a pathologist at Mount Sinai Hospital in New York. She says about a quarter of autopsies reveal something the clinician did not know about the patient’s cause of death.
Sometimes families also find comfort in learning about their loved ones’ final days. One woman recently told physicians at Massachusetts General that the autopsy of her mother, who died from Covid-19, made her feel “part of something bigger.”
“Families need to know that they have the right to be able to ask for an autopsy,” says Fowkes.
Most experts point to 1970 as a turning point. Autopsy rates had begun to decline a decade earlier, so in 1965, the Joint Commission, an organization that evaluates and accredits hospitals and other medical facilities and personnel, began requiring that hospitals autopsy at least 20 percent of their patients who died to identify opportunities to improve care. In 1970, the Joint Commission removed the requirement. At least some doctors welcomed the change: One physician, for example, explained in a letter to the Journal of the American Medical Association that hospitals were wasting time conducting autopsies simply to meet the metrics, rather than selecting valuable cases and using them to learn.
Autopsy rates declined dramatically. Recent policy changes threaten to push the number of autopsies even lower: In 2019, the Centers for Medicare and Medicaid Services (CMS), under pressure from President Donald J. Trump’s administration to cut regulations, removed a requirement that hospitals attempt to secure an autopsy in cases where deaths were unusual or could serve an educational purpose like teaching physicians about how a particular disease kills patients. “I don’t think that CMS really recognizes what they’ve done,” says Victor Weedn, a forensic pathologist at The George Washington University. But, he says, the previous autopsy requirement “was so diluted at that point — so disemboweled, so emasculated, that it really had very little meaning anymore.”

Stephen Hewitt in full PPE, prepared to conduct an autopsy on a Covid-19 patient.
Visual: Courtesy of Stephen Hewitt
Shrinking operating margins have also imperiled the practice. Insurance doesn’t generally cover autopsies. “As medicine has become closer to the bottom line, community hospitals don’t want to perform the autopsies because they’re not getting any functional reimbursement for them,” says Stephen Hewitt, a pathologist at the National Cancer Institute. Hospitals usually have to cover the expenses themselves — anywhere from $1,000 to $5,000 per patient — or pass the cost along to the patient’s family.
Autopsy rates have dropped in other countries, too. In a 2016 survey at a hospital in the Netherlands, the most common reason doctors and families gave for not performing an autopsy was that they believed they already knew the cause of death.
But pathologists say autopsies offer a level of detail that doctors can’t see in the living. “When you’re able to see what’s happening at the level of the cells, you just have a broader picture of the potential mechanism by which the disease is happening,” says Amy Rapkiewicz, a pathologist at NYU Langone Health.
Those benefits could seem especially important with the onset of Covid-19 — a novel illness with effects on the body that scientists and physicians are still scrambling to understand.
Indeed, in addition to hallmark symptoms like a fever, cough, and shortness of breath, Covid-19 can generate a wide range of symptoms, some more rare than others, including loss of smell and taste, altered brain function, heart problems, kidney damage, rashes, swollen toes, pink eye, vomiting, and diarrhea.
But as cases spiked this spring, a shortage of protective equipment and concerns about the possibility of catching the novel coronavirus from patients’ tissue initially kept autopsy rates low. Fowkes, whose New York City-area hospital was overwhelmed with Covid-19 patients in the first months of the pandemic, says that, out of 28 pathologists in her department, she was one of only four who initially volunteered to autopsy patients positive for SARS-CoV-2.
“There was a lot of fear,” she says.
Earlier this year, the Centers for Disease Control and Prevention and the College of American Pathologists published guidelines for safely conducting the procedures, requiring full-body protection and recommending the use of specially ventilated chambers that most hospitals don’t have.
As a result, “most institutions were not prepared” to do autopsies of Covid-19 patients, says Hewitt, and “even the groups that were willing to do the autopsies scaled back their protocols,” to look at specific organs instead of the whole body.
How Covid Affects the Body
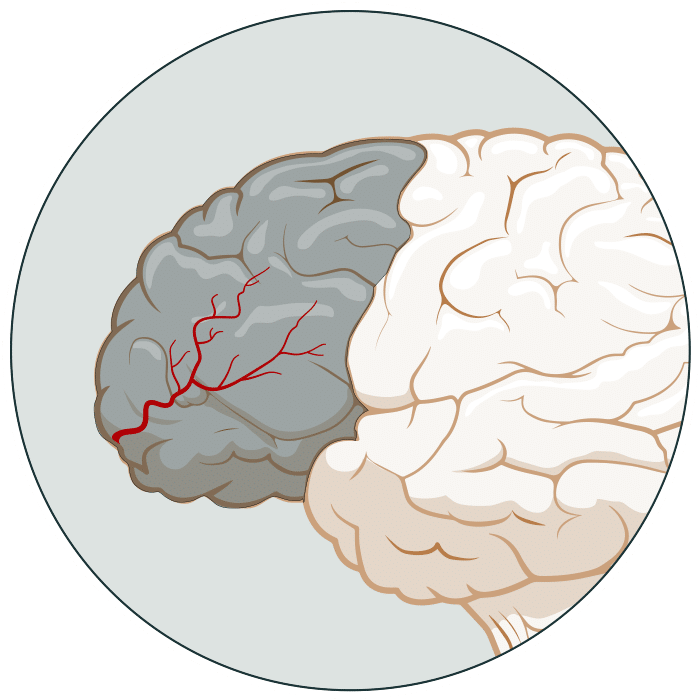
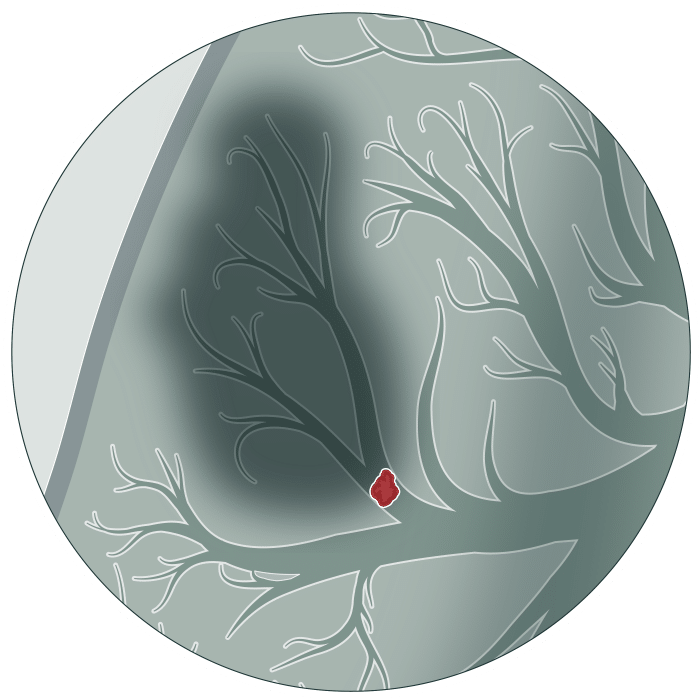
Early reports on Covid-19 characterized the new illness as a respiratory infection. Since then, though, physicians and researchers have documented impacts from Covid-19 throughout the body. Autopsies have played an important role in chronicling the myriad effects of a mysterious new disease.
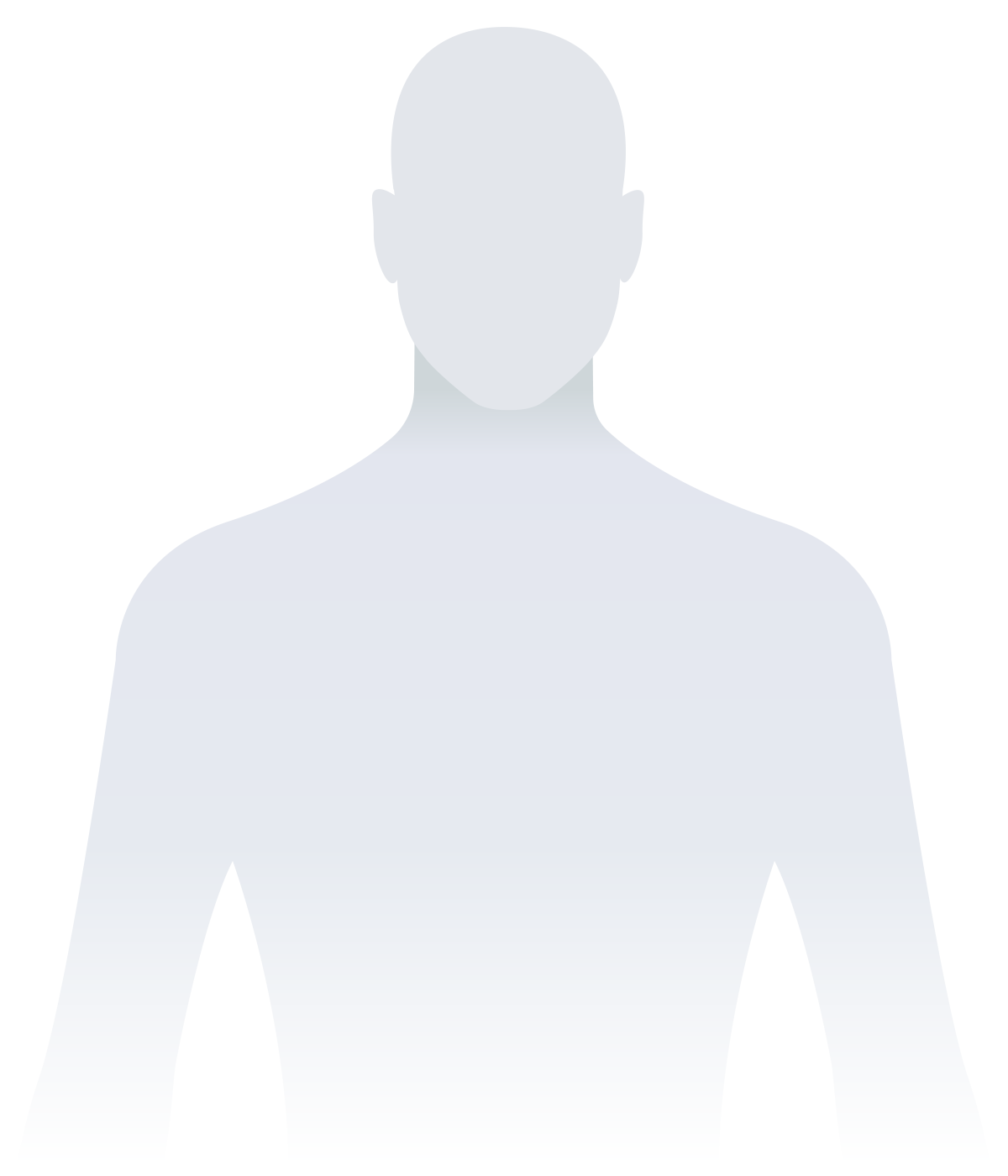

Click on the panels below to learn more
Brain
Brain
Autopsies have found SARS-CoV-2 in the frontal lobe of the brain and the lining of the brain’s blood vessels, adding to a growing body of evidence that Covid-19 can affect the nervous system.
Blood clots
Blood clots
Early in the pandemic, autopsies found blood clots throughout the bodies of Covid-19 patients. Especially alarming was the prevalence of pulmonary emboli: blood clots in the lungs that can be fatal.
Heart
Heart
Physicians have reported symptoms of myocarditis, a type of heart inflammation often caused by viral infections, in some Covid-19 patients. Autopsies have indeed found signs of Covid-related heart damage — but less evidence that myocarditis is the immediate cause.
Vascular system
Vascular system
Pathologists have found clues that SARS-CoV-2 may linger in blood vessels throughout the body. From there, some experts fear, it could potentially reignite infection.
Secondary infections
Secondary infections
As the immune system struggles to fend off the SARS-CoV-2 virus, other infections can spin out of control. One pathologist reports that three-quarters of patients he autopsied died from the secondary bacterial infections that emerge alongside Covid-19.
Other Covid effects
Other Covid effects
Along with well-known symptoms like fever, cough, and shortness of breath, Covid-19 can produce a range of other issues, including loss of smell and taste, rashes, swollen toes, pink eye, kidney damage, vomiting, and diarrhea.
As those autopsies began, though, pathologists started to make discoveries that could change the way physicians and researchers understand the effects of Covid-19 on the body. “When you look at autopsies now,” National Institute of Allergy and Infectious Diseases director Anthony Fauci told CNN in April, “we’re seeing things that we didn’t expect.”
In particular, early autopsies showed that Covid-19 was causing blood clots all over the body. Some were fatal: Fowkes says that in the first 17 patients her team autopsied, four had died from pulmonary emboli, blockages in the blood vessels of the lungs. Jeffrey Jhang, a pathologist at Mount Sinai who runs laboratory tests for living patients, had noticed some large clots in blood samples he received early on. As autopsies also demonstrated the pervasiveness of clotting, the team at Mount Sinai decided they should treat Covid-19 patients with blood thinners and regularly test for signs of clotting.
It seemed to work: Out of the next 83 Covid-19 patients Fowkes’ team autopsied, only one had died from a pulmonary embolus. Based on autopsy reports and other findings, anticoagulants are being tested in several randomized trials, and some national treatment guidelines now call for doctors to give clot-reducing medication to most Covid-19 patients.
Still, doctors are debating whether the treatment is beneficial for all hospitalized Covid-19 patients — barring those with certain underlying conditions — and at what dose. Some experts have criticized physicians at Mount Sinai for not conducting a randomized controlled trial when they adjusted their protocol, in order to better gauge its effects.
Autopsies have also built on observations made by physicians. As patients exhibited neurological symptoms like confusion and loss of smell, Fowkes and her team found the virus in the frontal lobe of a patient’s brain. The finding, published in the Journal of Medical Virology in April, provided some of the earliest evidence of the virus invading the central nervous system. But she was surprised to also find the virus in the lining of the brain’s blood vessels. The pathologists continued searching other organs for signs of SARS-CoV-2 infiltration and found clues that the virus may hide in vasculature throughout the body. She and her team now wonder if some patients may have low levels of virus “hanging around in the body” with the potential to reignite infection — a question that has inspired extensive debate among experts.
In some cases, autopsies may push physicians to rethink diagnoses. Rapkiewicz says many doctors have reported Covid-19 patients exhibiting signs of myocarditis, a dangerous type of heart inflammation often associated with viral infections. But, she says, “there really isn’t a lot of data from autopsies that has shown that’s actually the mechanism.” Instead, pathologists have begun to see evidence that the heart damage is caused by a variety of factors, including blood clots, ventricular strain — a condition in which part of the heart becomes deformed and struggles to pump blood efficiently — and stress. Each issue would require a different treatment.

Through autopsies, pathologists have also uncovered illnesses that sneak in behind Covid-19. Of the samples his team are analyzing, Hewitt says, about three quarters of patients are actually dying from secondary bacterial infections, rather than from Covid-19 itself. When the immune system is battered from fighting Covid-19, simple bacterial and fungal infections can become fatal. “I’ve got one right now on my desk where the patient was in the hospital for about two days,” says Hewitt. During that time, the medical team never realized that the patient had what Hewitt describes as “an overwhelming bronchopneumonia,” caused by a secondary infection.
Hewitt hopes autopsies will also help experts understand the lingering symptoms that haunt some Covid-19 patients for months. “What you see at autopsy represents an effective catalogue of the injury that occurs in patients who have Covid,” he says, “and it gives you an understanding and a basis to try and forecast forward what we’re going to see in post-Covid syndrome.”
These kinds of findings have led more hospitals with the resources to increase autopsies of Covid-19 patients to do so. “My impression from discussions with my colleagues around the country is that more and more centers are realizing that that there is value and importance to doing autopsies on patients with Covid-19,” says Stone.
Many pathologists hope that renewed respect for their work will have lasting consequences. Rapkiewicz, though, is not optimistic. Unless “there’s more of an operational change” she says, like reinstating policies that require a certain percentage of patients to be autopsied at each hospital, “I don’t see that there’s going to be a major shift.”
That’s unfortunate, she adds, because without autopsies, when it comes to any individual patient, “you’re really just guessing.”
Emma Yasinski is a freelance science journalist whose work has been published in The Scientist, Discover Magazine, and Kaiser Health News, among other publications.












Comments are automatically closed one year after article publication. Archived comments are below.
Families should understand that routine autopsies do not preclude open-casket funeral services.
Families reluctant to consent to autopsies for their loved ones may be reassured that no facial procedures are involved.