Evidence and Orthodontics: Does Your Child Really Need Braces?
Editor’s Note: The original version of this article failed to disclose that some of the quoted critics of orthodontics have financial ties to alternative, direct-to-consumer therapies. While the criticisms raised by these experts pre-date these financial ties by decades, and Undark’s reporting — both prior to and after publication — supports the story’s premise that there is disagreement within the discipline over many of the purported medical benefits of traditional orthodontics, these relationships should have been acknowledged in the original article. They have now been added, along with a response from the individual experts involved.
Peter Vig didn’t go into orthodontics looking to take on the entire field. When he entered the profession in 1963 as an academic, he optimistically saw orthodontics as a way to apply his knowledge to benefit patients. He would go on to receive his Ph.D. in facial morphology at the University of London, conduct research at a number of universities, and earn 18 grants from the National Institutes of Health. These feats propelled him, in the eyes of other orthodontists, to the status of research legend. But as his career took off, he became more disillusioned. The more time he spent entrenched in orthodontic research, the more he questioned what he had been taught in dental school: that orthodontic treatment was necessary for health.
Over the years, Vig submitted letters to academic journals, bemoaning a lack of strong evidence for the health benefits of orthodontic treatment and questioning what he calls “the prevailing dogma” of orthodontics. He once testified as an expert witness in a lawsuit against a fellow orthodontist. At one point, the American Journal of Orthodontics, now the American Journal of Orthodontics and Dentofacial Orthopedics, for whom he was a reviewer, was set to reject Vig’s own paper because editors feared that the results, which questioned the efficacy of diagnosis and variability in treatment, reflected poorly on the orthodontic profession. In response, Vig threatened to write an article about the ethics of orthodontic journals. (When contacted by Undark, the editor in chief of the American Journal of Orthodontics and Dentofacial Orthopedics declined to comment.)
Eventually, the editors did agree to publish the paper. But by that point, Vig had come to view the disagreement as yet another example of a lack of scientific integrity in orthodontics. “Shortly after that,” he said, “I quit.”
Vig is now semi-retired. Much has changed in the field of orthodontics since the height of his career. But according to him, orthodontic organizations haven’t stopped making claims unfounded in research. Orthodontics is largely considered a medical specialty, not just a cosmetic one. From small clinics to the American Association of Orthodontists (AAO), advertisements promise to prevent a host of ills ranging from cavities to jaw pain. Today, the AAO advises parents that all children should have an orthodontic consultation by age seven in order to identify potential problems and develop a treatment plan. According to the organization’s website, a lack of treatment can lead to tooth decay, gum disease, broken front teeth, and loss of bone tissue that holds teeth in place. Many orthodontic clinics additionally warn of persistent jaw pain and headaches.
A small group of dentists and orthodontists across the globe, including Vig, have looked carefully at the evidence underpinning these claims and found it lacking. Although some individual studies suggest that orthodontic treatment improves oral health, such studies are often fraught with bias and often don’t control for variables like socioeconomic status. Further, when the results of multiple studies are analyzed together, they do not provide evidence that orthodontic treatment decreases one’s likelihood of developing conditions such as gum disease and jaw pain.
Since the 1940s, there has been a steady increase in the percentage of children who receive orthodontic treatment. From 2010 to 2012, 16.8 percent of U.S. children between 10 and 14 years of age visited an orthodontist. And the proportion who see an orthodontist at any point throughout their childhood is likely much greater. Based on past data, it’s likely that around half of U.S. children today receive orthodontic treatment, according to Philippe Hujoel, an oral health epidemiologist at the University of Washington. Meanwhile, out-of-pocket spending on orthodontic treatments costs $5.4 billion per year. Private insurance and Medicaid cover an additional $4.2 billion of that care, and some nonprofits cover treatments for families in need when Medicaid deems treatment medically unnecessary.
The American Association of Orthodontists declined to comment to Undark. But many orthodontists stand by the association’s claims, and some have raised questions about the motives of some of the discipline’s critics — including Vig, who recently joined the clinical advisory board of, and will accept money from, a direct-to-consumer teeth-alignment company that is marketed as an alternative to traditional orthodontics. (Vig acknowledged his relationship with the company, but in an email noted that his academic work critiquing orthodontics precedes that relationship by decades.) Other experts, including Peter Greco, a clinical professor of orthodontics at the University of Pennsylvania and an associate editor of The American Journal of Orthodontics and Dentofacial Orthopedics, point out that orthodontic treatments are uniquely difficult to experimentally test, and so treatment decisions are often based on traditional knowledge and an orthodontist’s clinical experience, rather than on scientific evidence.
“That’s pretty much where the predominance of information is,” Greco said. But, he adds, the field is becoming more evidence-based as time goes on.
Some orthodontists who question their field’s claims about oral health do continue to treat patients. As they see it, clear communication of evidence — or lack thereof — is key. “If you tell a lay person” that a child has “mandibular hypoplasia, or maxillary deficiency, or adenoidal facies — it sounds bad,” said Vig. Parents don’t necessarily know what they’re signing up for. “That,” he says, “is a problem.”
Since antiquity, dentists from Egypt to Greece have sought the perfect bite. Mummies have been found buried in tombs with bands around their teeth. Even the Roman philosopher Pliny the Elder recommended that people file their teeth to bring them into proper alignment. By the early 18th century, French dentist Pierre Fauchard was strapping patients’ teeth to metal arches to wrangle crooked smiles into submission. Early in the 19th century, British dental surgeon Joseph Fox devoted four chapters of his book “The Natural History and Diseases of the Human Teeth” to the correction of crooked teeth and misaligned jaws.
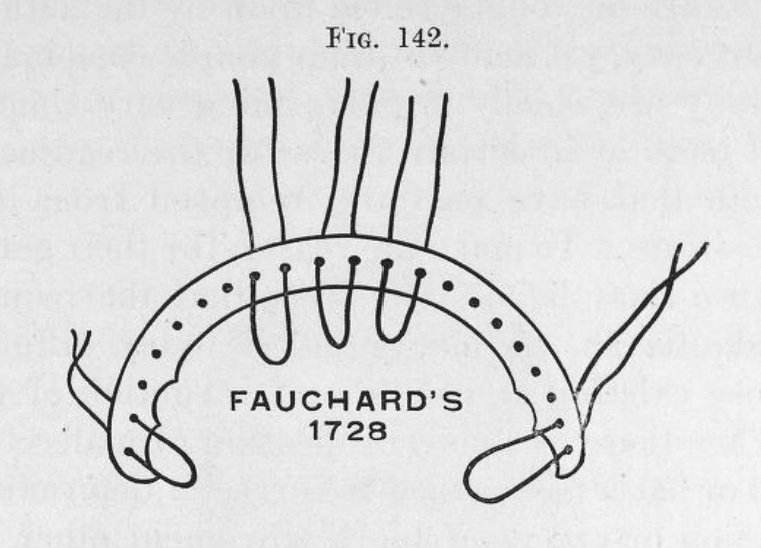
Pierre Fauchard’s “bandeau” — essentially a thin metal strip — was strapped onto patients’ teeth in the 18th century.
The end goal of these treatments, however, wasn’t to prevent health problems, but to create a more attractive profile, said Marc Ackerman, an orthodontist and medical ethicist in Boston. Norman Kingsley, considered one of the early fathers of orthodontics, was a classically trained sculptor. During his day job as a dentist in New York, he applied his understanding of facial symmetry to the faces of patients, diagnosing what he referred to as “irregularities” and “deformities.”
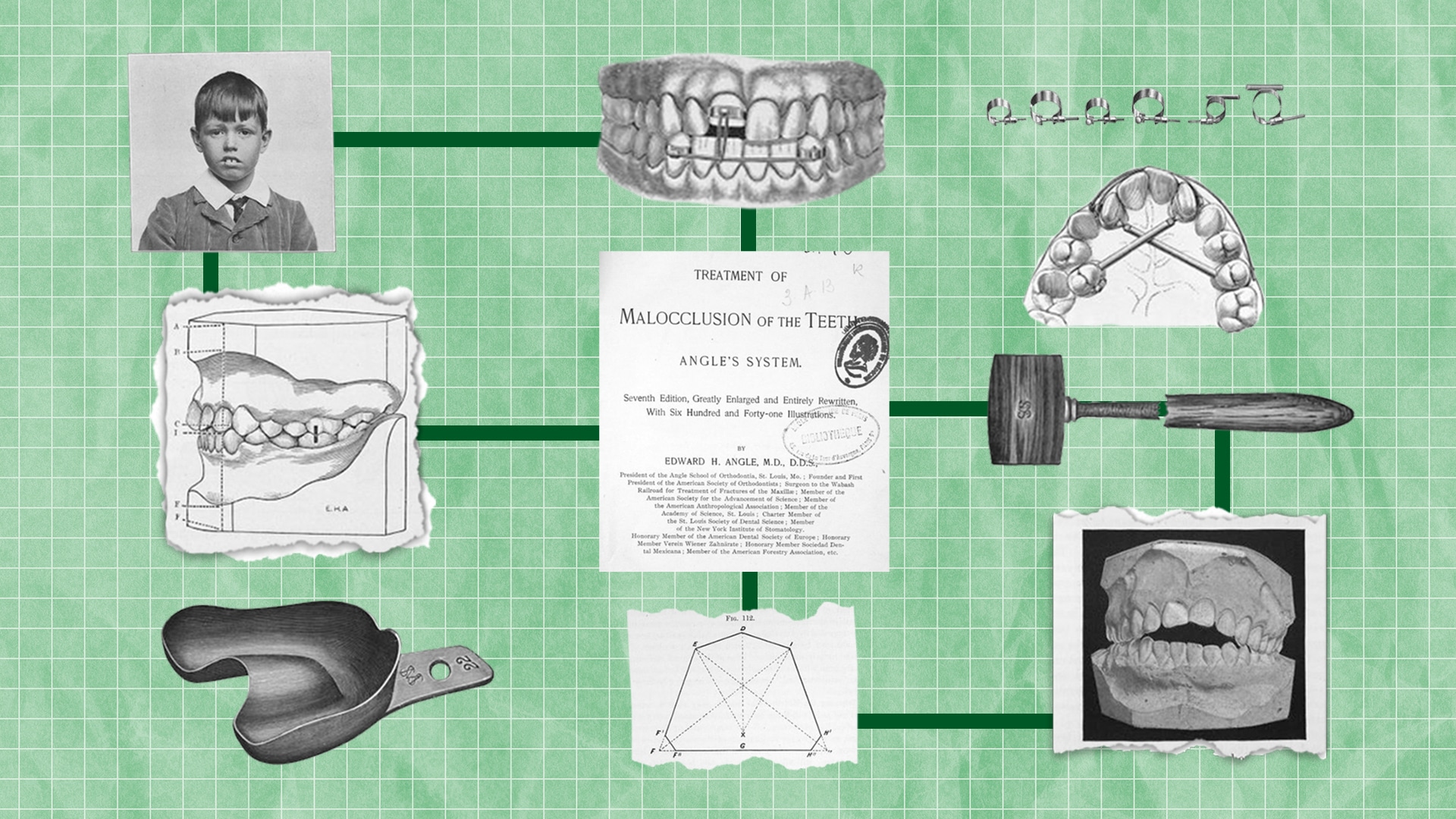
It wasn’t until the turn of the 20th century that an American dentist named Edward Angle transformed dentistry’s obsession with straight teeth into the modern science of orthodontics. In his treatise titled “Treatment of Malocclusion of the Teeth,” Angle laid out the precise parameters of a perfect bite, down to the millimeter. He based this ideal on the relative positions of the upper and lower first molars, which he believed should fit cleanly into one another, the crest of the top tooth into the divet in the middle of the bottom tooth. Any bite that deviated from this proposed ideal Angle deemed a “malocclusion” — Latin for “bad close.”
“This was probably the cornerstone of the medicalization in orthodontics,” said Alexander Spassov, an orthodontist and researcher in Greifswald, Germany. Angle’s criteria gave orthodontists a measure that could supposedly identify which bites needed treatment and which didn’t. Still, the transformation of orthodontics into a medical specialty was gradual and hard to trace back to a specific moment in history, Spassov said. For example, although Angle did help establish the specialty by founding both the first orthodontic school and the American Society of Orthodontists (today the AAO), he made no mention of health benefits, Spassov added. It was only later, perhaps after World War II, that orthodontics began to be seen as a preventative treatment for various ills, according to Ackerman.
More than 120 years after he waxed poetic about the “artistic harmony” of properly aligned teeth, Angle’s concept of an ideal bite is still the basis used to determine whether patients need orthodontic treatment. Orthodontists measure the overlap between patients’ jaws, the width of their palate, the crowding of their teeth. These measurements are compared to the ideal, then categorized by how they deviate in measurement. Class I malocclusions are the least severe; Class II and III, the most.
This process of systematically measuring teeth and pointing out the way they diverge from ideal is essential in creating demand, said Anette Wickström, a medical anthropologist at Linköping University in Sweden. Wickström studies medical procedures that normalize the appearance of children, such as gender-normalization surgeries performed on intersex children.
“Sometimes we see the medical domain as something that is neutral, just fixing problems. But at the same time, the medical domain is also enacting norms,” Wickström said. From measuring patients’ bites to communicating treatment goals, everyday orthodontic practices send a message that teeth should conform to a very narrow ideal — and anything less is abnormal.
According to a 2015 survey published in The Journal of Clinical Pediatric Dentistry, 57 percent of families seek orthodontic care primarily to give their child straight teeth. The same study also found that nearly 85 percent of parents who opted for treatment for their children did so due to a referral from the dentist. Dentists don’t typically refer patients to the orthodontist to treat an existing medical condition. Instead, the assumption is that getting teeth straightened out will prevent future ills, wrote Ackerman in a 2010 article for The Journal of Medical Ethics.
For parents, this referral carries the implicit message that treatment is both “necessary and worthwhile” for their child’s health, writes Bill Shaw, a professor of orthodontics and dentofacial development at the University of Manchester in the U.K., in an article published in the academic journal Seminars in Orthodontics. Shaw argues that a dentist’s referral to the orthodontist will initiate “a conveyor belt of entry into orthodontic treatment, with little or no reflection or discussion.”
Similar to Peter Vig, Alexander Spassov began his career under the assumption that orthodontic treatment improves oral health. In dental school at the University of Greifswald, the evidence behind this assumption was never questioned. After completing his residency there, Spassov took a job as a clinical lecturer and researcher in the medical school. Immersed in an academic environment, he saw his colleagues in other disciplines spend each day combing through research literature. These colleagues were engaging in what’s widely known as evidence-based medicine. Developed about 30 years ago, this medical paradigm emphasizes the use of high-quality research in medical decision-making, although in recent years, some experts have moved away from the term and has been much disagreement about what it means.
Following the lead of his medical colleagues, Spassov delved into the orthodontics research. When he found little to support the use of orthodontics as a preventative treatment for oral health, he was deeply troubled. In fact, he began to feel that the lack of evidence presented a “conflict with my professional and ethical principles.”
While continuing to teach orthodontics, Spassov began dialoging with colleagues in the university’s history, bioethics, and philosophy departments, sharing his concerns about offering treatment with weak evidence. In 2014, they published an article on the subject, in a prestigious German medical ethics journal. They pointed out that according to some estimates, fewer than 5 percent of the population fit Angle’s criteria for ideal occlusion (others estimate this proportion could be as high as 25 to 50 percent), and questioned the necessity of treatment, arguing that treatment decisions are often based on incomplete information provided to the patient, overemphasizing questionable benefits. The article cited studies demonstrating that simply brushing and flossing had a greater impact on oral health than orthodontic treatment.
Views like Spassov’s and Vig’s are outnumbered by orthodontists who say their treatments are medically useful. And as with Vig, some orthodontists suggested to Undark that Ackerman’s views are conflicted, given that he also has financial ties to a direct-to-consumer alternative to traditional orthodontics, which falls under the broader and controversial field of teledentistry. In an email message, Ackerman insisted that his advocacy on these issues preceded his financial relationship to teledentistry by several years, with his earliest critiques of orthodontics dating as far back as 2004. Still, many orthodontists stand firm on the discipline’s medical benefits. “Dental health is definitely enhanced by orthodontic therapy, and I stand firm on that,” said Greco, who added that he has seen the positive effects of orthodontic treatment in his own practice. As long as an orthodontist has received proper training and accreditation, Greco trusts them to make beneficial treatment decisions based on their knowledge and clinical experience.
Greco supports evidence-based orthodontics in theory, but putting it into practice takes effort, he said. The gold standard for research on humans is the randomized controlled trial, an experiment in which one group gets the treatment — say, braces — and the other gets a placebo, a varied duration of braces, or some other form of treatment. To eliminate bias, the groups are randomly assigned. At the end of the experiment, researchers compare the results for each group to see if the treatment really worked.
According to Greco, these kinds of studies are uniquely difficult to conduct for orthodontic treatments. For one thing, it’s hard to gather a large enough pool of study subjects to generate meaningful results, and the variation between patients makes it difficult to standardize the procedures. Together, these characteristics make it very difficult to conduct clinical trials where variables are controlled and treatment groups are randomly selected, Greco said. As a result, the majority of research simply compares people receiving orthodontic treatment, without controlling for other variables.
Clinical experience is one component of evidence-based medicine, said Hujoel, but alone it’s not enough. Clinical experience will tell you that a patient can come into the office with crooked teeth and walk out a few years later with a straight smile, Hujoel said. But to claim that changing tooth position has long-term health benefits? “That’s a huge claim to make without clinical trials,” Hujoel said.
Some individual studies do suggest that people with crowded teeth are more likely to have dental problems. For example, a 2000 study found that patients with crowded teeth had more plaque and pathogenic bacteria. And a study published in 2017 found that among nearly 15,000 participants, people who hadn’t received orthodontic treatment were more likely to have a serious gum infection called periodontitis. But because neither study was randomized, it’s difficult to know whether variables like socioeconomic class — a well-known factor in oral health — swayed the findings.
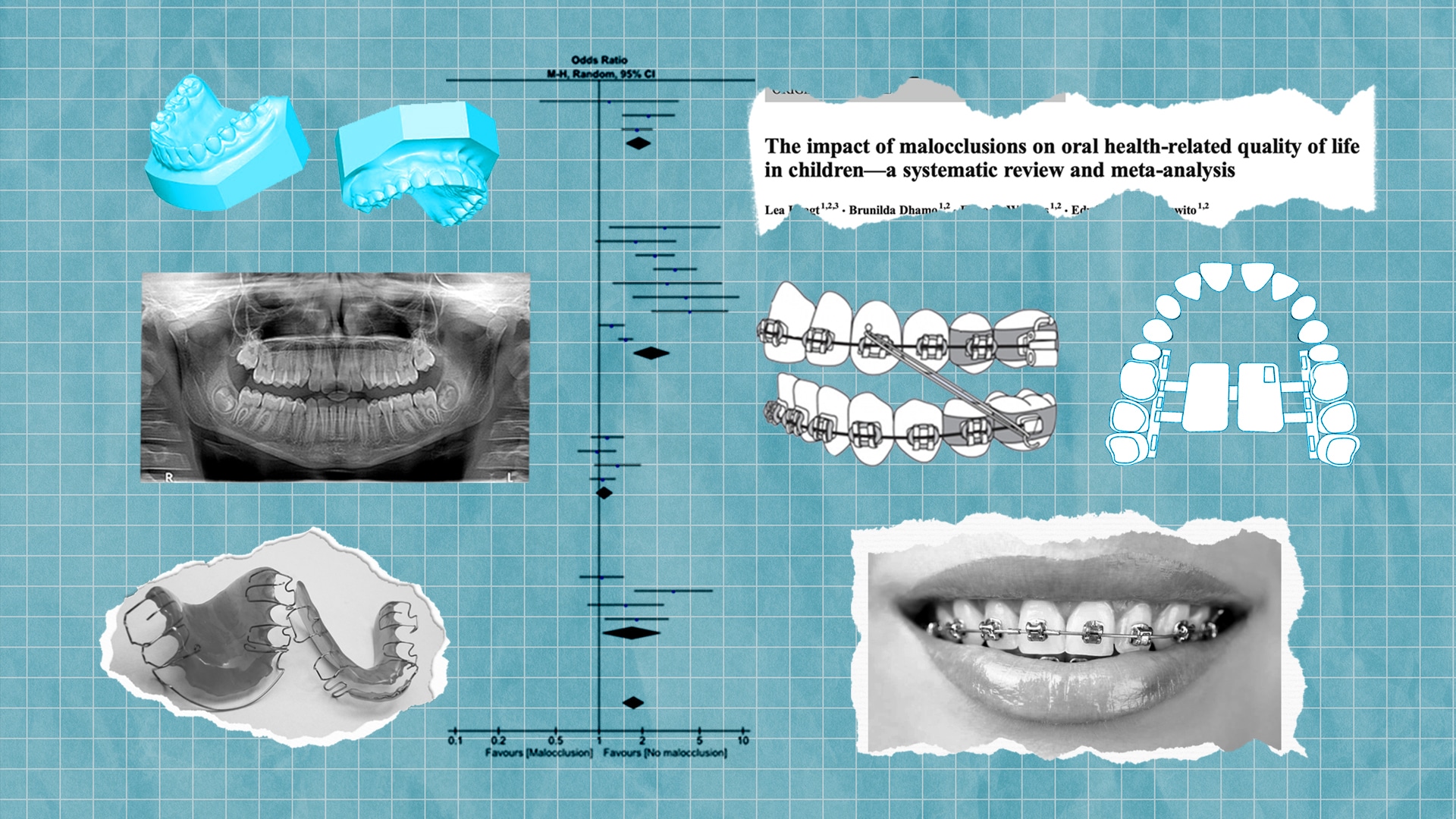
Further, when looked at as a whole, the research paints a troubling picture. Scientists from the University of Washington School of Dentistry carefully selected 12 studies on orthodontics and dental health. The group’s research, published in 2008 in The Journal of the American Dental Association, found that the dental health of individuals who received orthodontic treatment actually worsened slightly over the long term. A more recent study published in the June 2020 issue of The American Journal of Orthodontics and Dentofacial Orthopedics analyzed 7 studies on orthodontics and oral health. While this study didn’t find any evidence for worsened oral health, it came to a similar conclusion: The authors couldn’t find sufficient evidence in the scientific literature for the health benefits of orthodontic treatment.
Treatments aside, it’s not even clear that malocclusion causes bad health outcomes. While some individual studies find risks associated with malocclusion — jaw pain, for example — analyses of the larger body of literature tend to come up short. The 2020 study published in The American Journal of Orthodontics and Dentofacial Orthopedics also analyzed 87 studies on the effects of malocclusion on oral health and didn’t find enough evidence to suggest that crooked teeth lead to poor health outcomes.
Of course, not everyone visits the orthodontist to prevent cavities. Many go because they hope straight teeth will improve their life, said Stephen Richmond, a professor of orthodontics at Cardiff University in Wales. And there is some evidence to suggest that might be true — at least in children. In 2016, a team of orthodontists in the Netherlands analyzed the results of 40 studies and found that children with more crooked teeth tended to have a lower quality of life than those with straight teeth. However, the researchers didn’t take into account whether the studies controlled for socioeconomic status — a potentially powerful predictor of both quality of life and likelihood of receiving dental health care.
According to some orthodontists, this lack of objective evidence of health benefits is cause for concern. After all, treatment places a financial burden on families and the health care system, and it also poses some health risks. Even very small risks — from adverse reactions associated with surgical interventions to the long-term effects of X-ray exposure — are bound to impact a small but measurable number of patients if enough people are treated, Hujoel said. And millions of kids receive orthodontic treatment each year.
But others see things differently. “The cost-benefit [ratio] there is so low,” said Greco. “If you can readily correct a problem as a patient develops, you’d want to do that to give that patient every opportunity to develop normally, emotionally and mentally, physically,” Greco said.
No one is arguing that individual orthodontists are intentionally misleading patients. The problem is cultural, Ackerman said. Evidence just isn’t valued as highly in orthodontics as tradition and clinical experience. Although the American Dental Association Commission on Dental Accreditation requires an evidence-based curriculum, “It is largely paid lip service,” Ackerman wrote in an email. (The ADA did not respond to requests for comment.) Instead, his residency experience emphasized the classical practice of orthodontics. At one point during residency, Ackerman challenged his chair on a recommendation given to a patient. He still remembers the response he received: “Ackerman — Don’t confuse me with the facts, my mind is made up.”
As a lecturer, Spassov was interested in incorporating a more critical discussion of evidence into his curriculum. However, he said that his colleagues dissuaded him. He says he was warned that incorporating evidence-based principles would confuse students. According to Spassov, it is easier and less confusing to just teach the same content each year. But that shouldn’t justify avoiding the topic entirely, he said. Diverging evidence is “at the core of science and research,” he wrote in an email to Undark.
Orthodontists need to rethink how they communicate treatment needs with their patients, said Richmond. “Health professionals have to be careful what they say sometimes,” he said. “When they say, ‘you may have an issue,’ that gets stuck in your mind.”
Ackerman agrees that patients deserve nuanced and accurate information. In 2007 and again in 2018, he challenged the American Association of Orthodontists about specific claims on its website: namely, that malocclusion can cause loss of teeth, speech impediment, and poor nutrition. When asked for evidence to support these assertions, they dismissed the complaint with no real investigation, Ackerman said.
Around a decade after his first complaint, they finally modified the site — and only slightly. Still, it’s a step in the right direction, said Vig.
The website continues to list other risks of malocclusion without providing evidence. That’s what it’s like to fight back against a prevailing dogma with new evidence, said Vig — it’s wearying. In an ideal world, those making a particular claim should carry the burden of proof, he said. Instead, that burden of proof falls on that minority of orthodontists willing to challenge the status quo — orthodontists like Vig, Ackerman, and Spassov. Each time they publish a paper that risks painting the profession in a negative light, each time they demand evidence for a claim, they meet resistance, Vig said. “It makes us pariahs in our profession.”
Isobel Whitcomb is a science reporter based in the Pacific Northwest. Her work has appeared in Bay Nature Magazine, Hakai, and Atlas Obscura, among other outlets.












Comments are automatically closed one year after article publication. Archived comments are below.
Thank you so much for writing this article. It is incredibly helpful to know that this field does not have the same type of scientific research behind it that other medical fields do. As the parent of a child-patient who has braces and now needs headgear that I’m questioning, I would have liked to have known this from the start, when the dentist made the referral. Bravo for getting this information out there!
I am a parent of a 7 year old child who has been wearing braces now for 6 month and was informed she needed to wear them for at least a total of 2 years. I found your article because I wanted to know more about the negative side effects of wearing braces. Since she started wearing braces she developed bad breath. It is clear to me she is now spending more time with her mouth open and brushing her teeth poorly. She didn’t had bad breath before. And she was trained from baby to breath through the nose and brush well her teeth. However the form of the mouth with braces leads to be easier to stay with the mouth open and braces make brushing teeth for a 7 year old more complex, consequently we believe it could promote more bacteria. Our dentist and ortodentist only told us about the benefits (esthetic) and so I need to do my own research to check if there are disadvantages and what to do instead. So thank you for your article.
Beautifully explained, recommendation is to add link to evidences literature like textbooks evidence based orthodontic, recently seen new literature coming out in 2023 like https://orthodonticevidence.com
Dave Batista
DMD MS Orthodontics
I enjoyed your article, Ms. Whitcomb. I found it very informative.
Information on long term outcomes would have been a valuable addition to the material presented. I have not found a very readable, informative source on outcomes. From the tidbits I have read elsewhere, it seems patients’ outcomes post-treatment sometimes revert to initial conditions in some non-trivial fraction of cases. I think this warrants further investigation.
As a third generation orthodontist, one of a handful in the U.S., I am proud and still in awe of orthodontic treatment’s social impact on patients. When I wrote my book, Enhancement Orthodontics (2007), I recommended that we as a specialty adopt a more holistic definition of orthodontic health with an emphasis on crooked teeth’s impact on social health and disability.
One part of the conversation that I had with the author of this piece, which was not included in the article, is the fact that many third-party public payers and some private payers require that orthodontic treatment be medically necessary in order for their subscribers to gain access to the benefit and for the orthodontist to receive their fees. If these payers decided that the literature does not support the contention about medical necessity, it would be economically catastrophic for orthodontists. This is precisely why this topic is so contentious and has generated far more heat than light.
In the end, it comes down to the ethical question of what an orthodontist tells a patient is the reason they need treatment and whether this satisfies the principle of veracity.
— Marc Bernard Ackerman, DMD, MBA
No discussion at all about the causes of crooked teeth. Why do hunter gatherer skulls have excellent teeth compared to modern man? Look into Weston Price for example. Our soft hypercaloric processed diet fails to exercise the jaw muscles properly among other factors. Check out Mike Meeks’s videos https://youtu.be/AyCEY3BvxRg
The article is fair.
But the contentious criticism is fundamentally a “straw man” argument
.
That is, the question it begs is
“So what?”
“True. The “science justification” is minor for most but solid for a few.”
More salient: it takes intelligence and assiduous scholarship to tell the difference in individual cases.
Besides, when have you ever heard:: “I had my teeth straightened and I regret my new smile. I wish my teeth were crooked again.”
Wake up!
It’s not about teeth.
It’s about the attractiveness of the lower half of a innocent child’s FACE at a critical time of development, when permanent self esteem is in jeopardy
That is critical because human face is the key to identity.
Ergo, orthodontic therapy for achieving a beautiful face is, like a rhinoplasty or breast surgery, a psycho-social imperative, viz. mainly art, indulged – by the intellectually misguided – in an endless search for an “unshakable’ scientific justification.
I ask “Why search?”
Beauty (like love or health) – philosophically speaking – is considered ontologically as a “First Principle”
Science is only a tool not a “sine qua non”.
Beauty per se is a construct that needs no scientific justification.
Orthodontic therapy has too little scientific foundation. OK. Fine.
The same can be said about “parachute use.”
Ponder that.
NCM
Neal C. Murphy DDS, MS
Clinical Professor (Ret.)
UCLA 1981-2010
.
Great piece, Ms. Whitcomb! Really well written and enlightening. Thanks for digging into this topic and sharing your findings!