Amid Hydroxychloroquine Hopes, Lupus Patients Face Shortages
For almost a quarter century, Julie Powers, a 48-year-old non-profit professional from Maryland, has been taking the same medication for her lupus — and until recently, she never worried that her supply would run out. Now she’s terrified that she might lose access to a drug that prevents her immune system from attacking her heart, lungs, and skin. She describes a feeling akin to being underwater, near drowning: “That’s what my life would be like,” she said. “I’ll suffocate.”
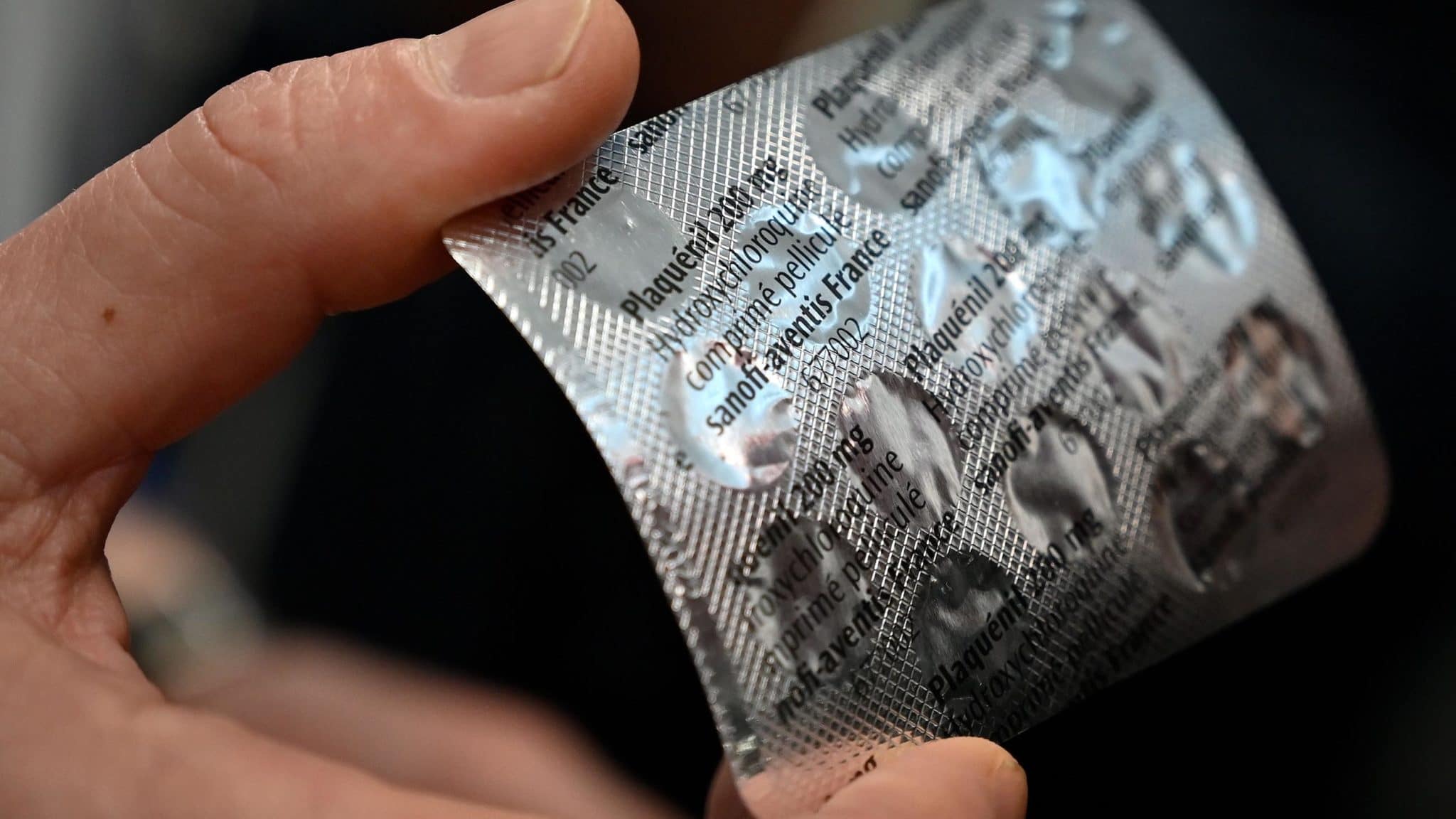
Powers’ concerns began roughly a week ago when she learned that her lupus drug, hydroxychloroquine (hi-DROCK-see-KLORA-quin), may be helpful in the treatment of Covid-19, the illness caused by the SARS-CoV-2 virus now racing across the planet. The medication was already being used around world to treat Covid-19 patients, but evidence of its effectiveness was largely anecdotal. Then, on Monday, March 16, a renowned infectious disease specialist, Didier Raoult, announced the results of a small clinical trial in France showing that patients receiving a combination of hydroxychloroquine and the common antibiotic azithromycin had notably lower levels of the virus in their bloodstream than those who did not receive the medication.
Upon hearing this news — and anticipating a possible drug shortage — Powers called her rheumatologist that same day and requested a prescription for a refill. She was lucky to get it.
In the last week, this once obscure drug has been thrust into the national spotlight with everyone from doctors, to laypeople, to the U.S. president weighing in. The attention has so dramatically driven up demand that pharmacists are reporting depleted stocks of the drug, leaving many of the roughly 1.5 million lupus patients across the country unable to get their prescriptions filled. They now face an uncertain future as the public clings to one of the first signs of hope to appear since the coronavirus began sweeping across the U.S.
But scientists and physicians caution that this hope is based on studies that have been conducted outside of traditional scientific timelines. “The paper is interesting and certainly would warrant future more definitive studies,” Jeff Sparks, a rheumatologist and researcher at Harvard Medical School, said of the French study. “It might even be enough data to use the regimen off-label for sick and hospitalized patients.
“However,” he added, “it does not prove that the regimen actually works.”
This has not stopped widespread promotion of the drug cocktail — including by U.S. President Donald Trump, who has helped to stoke demand for hydroxychloroquine by invoking it during his daily coronavirus press briefings. In a tweet on Saturday, the president described the regimen as possibly one of the “biggest game changers in the history of medicine.” (Anthony Fauci, the infectious disease expert spearheading the U.S. response to the coronavirus pandemic, called the evidence for the treatment anecdotal. “You really can’t make any definitive statement about it,” he told reporters Saturday.)
Despite efforts to pin blame for the shortages on Trump alone, however, hydroxychloroquine scarcity was already setting in weeks ago, as doctors began responding on their own to percolating and preliminary research. Some evidence suggests that many doctors are now writing prescriptions prophylactically for patients with no known illness — as well as for themselves and family members — prompting at least one state pharmacy board to call an emergency meeting, scheduled for Sunday morning. The board planned to bar pharmacists from dispensing chloroquine or hydroxychloroquine for anyone other than confirmed Covid-19 patients without approval of the board’s director.
A prolonged shortfall in supplies would likely have grave implications for people who depend on it — including Powers, who believes that she would not be alive today without the drug. “I guarantee you, it has saved my life,” she said. “It’s the only thing that’s protecting my organs. There’s nothing else.” Like others, she hopes that pharmaceutical companies that manufacture versions of the drug will be able to quickly ramp up production — something several have already promised to do. In the meantime, Powers has a message for the American public — one echoed by most lupus doctors: When it comes to hydroxychloroquine: “If you don’t need it, don’t get it.”
The origins of hydroxychloroquine can be traced back hundreds of years to South America, where the bark of the cinchona tree appears to have been used by Andean populations to treat shivering. European missionaries eventually brought the bark to Europe, where it was used to treat malaria. In 1820, French researchers isolated the substance in the bark responsible for its beneficial effects. They named it “quinine.” When the supply from South America began to dry up, the British and Dutch decided to grow the tree on plantations.
Over time, synthetic versions were developed, including a drug called chloroquine, which was created in the midst of World War II in an effort to spare overseas American troops from malaria. As it turned out, troops with rashes and arthritis saw an improvement in symptoms after using this anti-malarial medication. After the war, a related drug was created, one with fewer side-effects when taken long-term: hydroxychloroquine. It went on to be used to treat many types of autoimmune diseases, including rheumatoid arthritis and lupus. The latter, which disproportionately affects women, used to cut lives short — typically from failure of the kidneys. Those numbers have been reduced with strict management of the disease, but the Lupus Foundation of America estimates that 10 to 15 percent of patients die prematurely due to complications of the disease.
Right now, hydroxychloroquine is one of the few FDA-approved drugs for lupus, said Ashira Blazer, a rheumatologist and researcher at NYU Langone Health. The medication is a staple of lupus treatment because it has been shown to decrease symptom flare-ups, or “flares.” Over time, this leads to better health and less organ damage, Blazer said. Patients who take hydroxychloroquine are less likely to develop diabetes, kidney disease, and early heart disease, among other benefits. Because so many lupus patients are doing well on hydroxychloroquine, Blazer said, “we don’t want them to have to go without.”
Jinoos Yazdany, a researcher and chief of the Division of Rheumatology at Zuckerberg San Francisco General Hospital, added that there is strong clinical trial data demonstrating that taking a group of lupus patients off of hydroxychloroquine results in lupus flares. “I am less concerned about a short interruption of a few weeks,” she said in an email message, “but anything longer than a month puts patients at risk.”
Whether or not that will happen is unclear, but Sparks said he has been receiving a raft queries from both lupus and non-lupus patients eager to know more about — and access — hydroxychloroquine: “Can I use this? Should I stockpile it? Can I get refills?” Sparks compares the current medication shortage to the ventilator shortage, where manufacturers make just enough of a certain supply to meet the demand. “We don’t have stockpiles of hydroxychloroquine sitting around,” he said.
Demand is surging. Antonio Ciaccia, the chief executive of 46brooklyn Research, a non-profit drug pricing research organization, says that the combination of new studies and interest from the Trump administration created “a magnetic pull” for people, even for those who don’t currently have an illness. Ciaccia, who has been communicating with industry contacts and hospital pharmacists, says new demand is coming from doctors writing prescriptions for themselves, their family members, and their colleagues. Ciaccia declined to say whether a physician should or should not self-prescribe. But he does have an opinion on family members and colleagues filling prescriptions without any symptoms or known exposure to the virus. “I would throw that in the bucket of totally unethical,” he said.
Blazer understands that people are scared and says it’s natural that they would want to protect themselves. But she said, the medicine is a limited resource and should be reserved for people with a rheumatological disease or active Covid-19 infection. In order to minimize fallout from the pandemic, she says, “we all have to function as a community.”
As it turns out, there is an extreme paucity of data when it comes to hydroxychloroquine and Covid-19. On March 10, the Journal of Critical Care published online a systematic review of the safety and the effectiveness of hydroxychloroquine and chloroquine in treating Covid-19. The authors’ goal was to identify and summarize all available scientific evidence as of March 1 by searching scientific databases. They found six articles. (In contrast, a search of the database PubMed for hydroxychloroquine and lupus yields 1,654 results.)
“The articles themselves were kind of a menagerie of things that you don’t want to get data from,” said Michael Putman, a rheumatologist at Northwestern University, McGaw Medical Center, in his rheumatology podcast. The study authors found one narrative letter, one test tube study, one editorial, two national guidelines, and one expert consensus paper from China. Conspicuously missing were randomized controlled trials, which randomly assign human participants to an experimental group or a control group, with the experimental group receiving the treatment in question.
“It is kind of scary that that is all the data we had until March 1, for a drug that we are currently talking about rolling out en masse to the world,” said Putman.
Shortly after the systematic review appeared online, Didier Raoult announced the results of his team’s clinical trial. (The paper is now available online.) At first blush, the results are striking. Six days into the study, 70 percent of patients who received hydroxychloroquine were “virologically cured,” as evidenced from samples taken from the back of each patient’s nose. In contrast, just 12.5 percent of the control group, which did not receive the drug cocktail, were free of the virus.
 |
Got questions or thoughts to share on Covid-19? |
But experts who have looked more closely at the study have begun raising questions about whether the medication is responsible for the groups’ different outcomes. Alfred Kim, a rheumatologist, researcher, and director of the Washington University Lupus Clinic, noted that the French study was small, with just 42 total participants, and only 26 patients actually receiving the medication. Six patients also ended up dropping out of the study — all of them from the group receiving hydroxychloroquine. Among these, three were transferred to the intensive care unit, one died, one left the hospital, and one stopped the treatment because of nausea. Kim suggested some of these could be viewed as failures of the drug to work against the virus.
A second potential issue: Patients who refused the treatment or had exclusion criteria served as controls. “It’s hard for me to describe just how problematic this is,” said Putman in his podcast. Ideally patients would be randomly assigned to one of the two treatment groups, said Putman. Patients with exclusion criteria — those unable to take the medication — are not the same as patients who are able to take it, he says. And the same is true for patients who refuse a drug vs. those who don’t.
Whether these and other potential problems with the research will prove salient in coming weeks and months is impossible to know — and most researchers concede that even amid lingering uncertainties, time is of the essence in the frantic hunt to find ways to slow the fast-moving Covid-19 pandemic. “A lot of this,” Kim said, “is the rush of trying to get something out.” On Friday, the University of Minnesota announced the launch of a 1,500-person trial aimed at further exploring the efficacy of hydroxychloroquine against SARS-CoV-2. And drug makers Novartis, Mylan, and Teva announced last week that they were fast-tracking production, with additional plans to donate hundreds of millions of tablets to hospitals around the country to help combat Covid-19 infections.
Still, reports of shortages are mounting. “It’s gone. It’s not in the pharmacy now,” a physician in Queens told The Washington Post on Friday. The doctor admitted taking the drug himself in the hope of staving off infection, and that he’d prescribed it to 30 patients as a prophylactic.
These sorts of fast-multiplying, ad hoc transactions, are what worry lupus patients like Julie Powers. For now, she says she has enough hydroxychloroquine to last 90 days, and she added that her pharmacist in the Washington, D.C. area is currently hiding the medicine to be sure her regular lupus patients can get their prescriptions refilled.
Powers sounds almost amazed when she describes what that means to her: “I can walk outside,” she said, “and I can live.”
Sara Talpos is a senior editor at Undark and a freelance writer whose recent work has been published in Science, Mosaic, and the Kenyon Review’s special issue on science writing.
Disclosure: The author’s spouse is a rheumatologist at Michigan Medicine.
UPDATES: This story has been updated to clarify Alfred Kim’s view on several patients who dropped out of a small French study on the efficacy of using hydroxychloroquine to treat Covid-19 cases. The piece was also edited to include information noting that one state pharmacy board is now taking steps to curtail prescriptions of hydroxychloroquine and chloroquine for Covid-19 prophylaxis.









Comments are automatically closed one year after article publication. Archived comments are below.
I’m sorry. But this lady does not need to be worried about losing a drug for a very short time to cater to people who are losing their life. I myself have taken hydrochlorquine for my arthritis and know that there are different options out there to use if this drug no longer becomes available. I myself would give up using the drug for months if it were to save someone else’s life. I even stopped the use of hydrochlorquine by lowering dramatically sugar and carbs from my diet to feel better quickly. I would do this to help humankind. So should this lady. Stop trying to make the use of Hydroxychloroquine a bad deed. This is just another price of crap to help the Americans die because of politics.
Kill yourself faster with toxic medications. Having lived in a number of malaria zones I know these drugs have negative impact on kidneys and liver, both critical to good health. When will people realise the only thing which keeps and gets them well is a healthy body and immune function and not a pill or vaccine?
I have SLE, the same disease my 45 yr. old sister died from, I can’t get my scripts filled anywhere, everyone is out of the very drug that keeps me alive, I’m guessing when it does become available, it will have quite an increase in price! Knowing I have an autoimmune disease, I’ve been staying home & mostly alone, but without my meds, if Coronavirus doesn’t kill me, my SLE will, shame on these drug Companies!
Plaquenil has 1/2 life of 32-50 days. In layman’s terms this means that if you took your last dose for lupus or RA today then you should be relatively fine until pharmacies restock in a few weeks. It is scary as a patient and I empathize with the concerns. I also understand the desire to have hope in this very well established and relatively safe (across a broad range of healthy people and patients with comorbitities). As Anthony Fauci points out we need better data from randomized, double blinded placebo controlled studies to feel scientifically secure. But speaking from a position of “scientific-based intuition “ I feel a great sense of hope for this medication against the worlds most formidable and unprecedented infectious diseases….of all time in recorded human history.
Well most people buy a 30 or 90 day supply. and if a run on the drug hit right at the end of your 30-day supply perhaps it is tight give the drugstores a couple days to restock. I’m at least two major drug companies have already agreed to put into the supply as soon as possible at least 10 million doses of the drug
I am a person diagnosed with Lupus. I went to Walgreen to purchase my medication for Lupus. The pharmacist informed me there was none. So what are people who need this medication to do?
Ask your doctor to prescribe another medication.
This is outrageous that patients who have been on Hydroxychloroquine now may need to do without. I am currently on Methotrexate injections once week and also take Hydroxychloroquine every day. I understand the need to research any possible cure for this virus…but please consider those who need this on a daily basis. Maybe this needs to be monitored more closely to make sure this drug is not being handed out to those who don’t really need it.
I have Lupus and no one knows.
I use cannabis.
It’s an anti-inflammatory & anti-viral.
Both my doctors advised me against it. My rheumatologist conferenced called my dermatologist during my appointment. The Plaquenil made me feel like I was on cocaine.
The choice was easy.
I am Canadian. Cannabis is legal.
Perhaps time for Lupus patients to officially ” trade up” for more than one reason.
Two companies said they’re going to be turning it out as fast as possible.
I also have Lupus. I am scared I will not be able to get it. I have enough for 15 days. That is not good.