A New Japanese Stem Cell Treatment Raises Hopes — And Ethical Questions
In 2015, Shinji Kusachi, a 47-year-old teacher living in the Japanese prefecture of Okayama, was high-diving at a local pool — a passion he had developed in his 30s — when a tricky dive went awry. “I hit my head on the bottom,” Kusachi recalled of the incident that damaged his spinal cord and left him mostly paralyzed. “They said I couldn’t use my arms and legs. I was really in despair.”
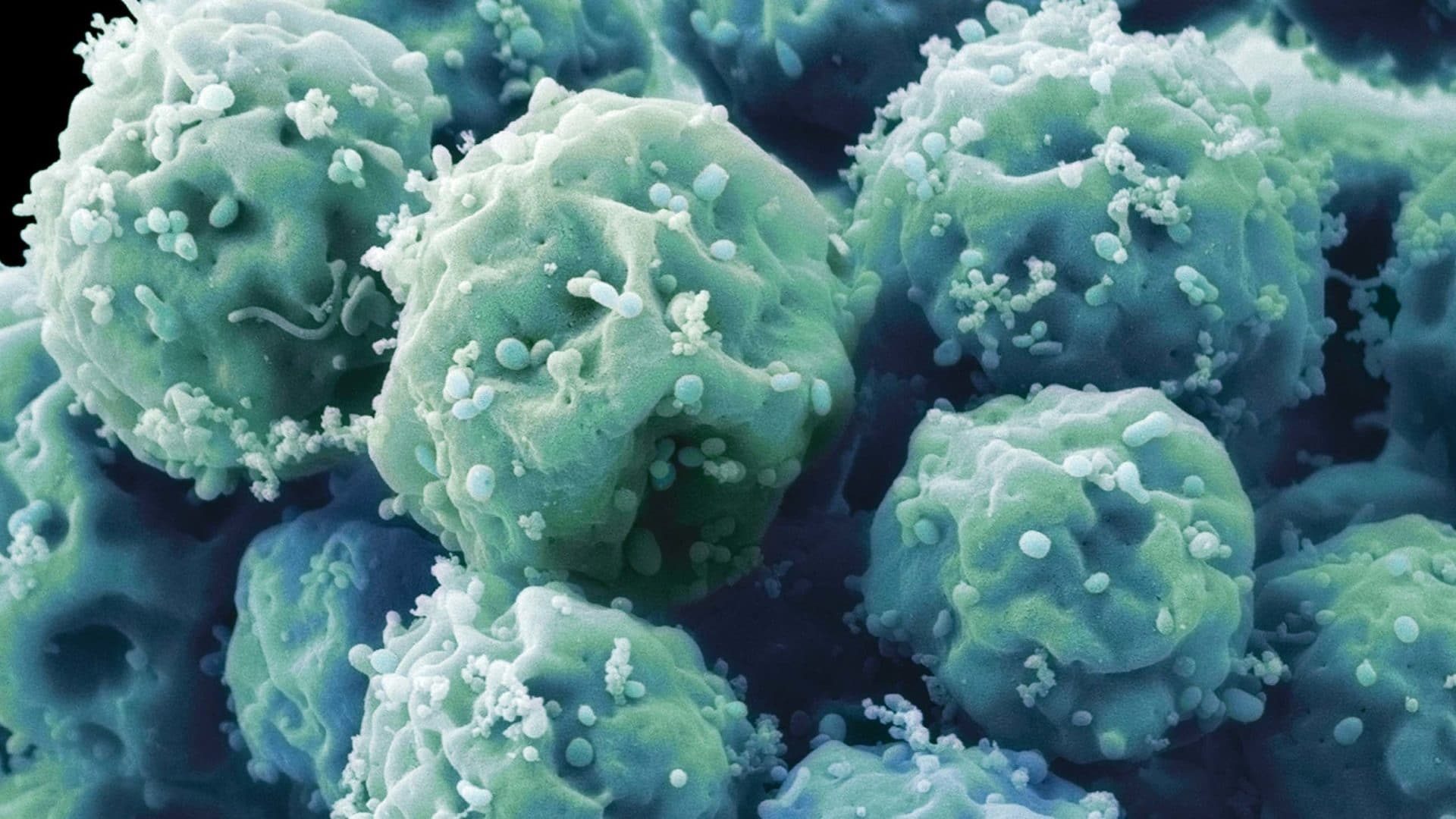
But Kusachi soon joined a clinical trial for a new treatment for spinal cord injuries called Stemirac. Researchers at Sapporo Medical University drew fluid from his bone marrow, isolated a type of stem cell found there, multiplied the cells in the lab, and infused them back into his bloodstream intravenously. The day after the treatment, Kusachi dramatically improved. “That was a real surprise to us,” said Toshihiko Yamashita, an orthopedic surgeon at the university. “In the afternoon, he could rise up from his bed and sit. In the evening, he was getting around in a wheelchair.”
The improvement continued. Seven months after the injection, Kusachi left the hospital under his own power. Today, although control of his hands and feet is still clumsy, he cooks, drives, and teaches math online — all thanks, he says, to Stemirac.
The Japanese health ministry approved Stemirac last December, and the treatment is now available to the Japanese public, with most of the $140,000 cost covered by the country’s universal National Health Insurance. It’s arguably the world’s most ambitious approved stem cell treatment and should have been a cause for celebration: a long-awaited breakthrough for the field of regenerative medicine — using modern biological tools to repair the body — and a harbinger of more impressive medicines.
Instead, the therapy has been met with a heated debate. On one side, many experts have slammed Stemirac’s approval in uncommonly direct terms, saying there isn’t enough evidence to show it is effective or even safe. The treatment went through an expedited approval unique to Japan: After short, small clinical trials that suggest safety and efficacy, regulators can approve stem cell treatments on a conditional basis — allowing use of the treatments for seven years, while sponsors gather additional evidence to support a full approval.
Critics also say Japan’s approach is far too soft — that early approvals allow patients to take experimental therapies that could be ineffective or dangerous, at a high cost to both patients and insurance providers. “This is essentially an unproven therapy,” said Arnold Kriegstein, a stem cell researcher at the University of California, San Francisco. “I’m very surprised this is happening in a country like Japan.” Doug Sipp, a policy researcher at the RIKEN Center for Biosystems Dynamics Research in Kobe, and a colleague at the University of Sussex argued in the August 16th issue of Science that the new approval system is the result of countries competing to approve therapies faster, which raises the risk of mistakes.

Meanwhile, proponents of the new approval system, especially libertarian critics of traditional drug regulation, say it points to the future of medical innovation not only in Japan but also in the United States and other technologically advanced countries.
On one level, the debate would seem to hinge on an empirical question: What is the fastest, surest way to identify the safest, most effective treatments and medicines? But critics of Japan’s approach suggest that the answers aren’t always so simple, and that health care systems, by definition, need to more carefully weigh the many tradeoffs between safety and innovation, as well as who gets to decide which matters more.
Japan’s conditional approval system traces a spiritual lineage to American libertarian thought, like the Nobel Prize-winning economist Milton Friedman’s 1979 book ”Free to Choose: A Personal Statement,” co-authored with his wife Rose. Friedman later summarized one of his more controversial arguments: “The [Food and Drug Administration (FDA)] has already done enormous harm to the health of the American public by greatly increasing the costs of pharmaceutical research, thereby reducing the supply of new and effective drugs, and by delaying the approval of such drugs as survive the tortuous FDA process.”
Subsequent libertarian writers put a finer point on Friedman’s argument. Daniel Klein, an economist at George Mason University, said the FDA erred by barring pharma companies from advertising aspirin to prevent heart attacks. “The FDA surely killed tens, and quite possibly hundreds, of thousands of Americans by this restriction alone,” he wrote in 2000.
A decade later, free market advocate Bartley Madden advanced a proposal for speeding the drug-approval process in a book called “Free to Choose Medicine,” published by the Heartland Institute, a libertarian think tank. The centerpiece: a system of expedited, conditional approvals based on small clinical trials hinting at safety and efficacy. Masaru Uchiyama, the president of the right-leaning advocacy group Japanese for Tax Reform, had the proposal translated into Japanese and sent 800 copies to government officials, health care professionals, researchers, and patient groups. Soon, the staff of Japan’s drug regulating agency were mentioning the idea in presentations, according to Sipp.
In Japan, “Free to Choose Medicine” found a welcome home: a country looking for a comeback. While remaining a prosperous country with the world’s third-largest economy, Japan is in something of an economic malaise that’s lasted for much of three decades. The population is the second-oldest in the world, behind Monaco, and it’s shrinking; the economy trundles through what Bank of Japan Governor Haruhiko Kuroda dubbed a “deflationary mindset” stemming from what are often referred to as the “lost decades” after the post-war boom; and after pacing the technology world in the 1980s, Japan was late to tech revolutions like the personal computer and smartphone.
But in 2007, an opportunity opened when Kyoto University researcher Shinya Yamanaka showed how to reprogram adult skin cells to potentially become almost any part of the body. His discovery of this capability in mice the previous year would go on to win Yamanaka a Nobel Prize.
This made-in-Japan discovery provided a technological edge. “Stem cells were relatively new, and the Japanese government was very excited to hear about iPS cells for humans,” said University of Tokyo medical sociologist Kaori Muto. Yamanaka’s “cells were the great hope for Japanese government and scientists to become number one again.” When Shinzo Abe became prime minister in 2012, the government prioritized stem cell science, pledging to commit more than a billion dollars to relevant research. The treatments would be useful worldwide but especially so in aging Japan; successful biotech businesses would help goose the economy; and a scientific triumph would help restore the nation’s technical reputation and confidence.

But creating and testing stem cell treatments promised to be long and expensive. So in 2014, the government adopted an accelerated approval system for regenerative medicines, much like the proposal in “Free to Choose Medicine.” The approach has already succeeded in one goal: drawing the attention of pharmaceutical and biotech companies with the promise to get drugs on the market quickly.
“Instead of having to go to the market, saying, ‘Hey investors, can you pony up an extra $50 million to fund our clinical trial?’, companies can get conditional approval far more easily,” said Colin Lee Novick, a regenerative medicine consultant at CJ Partners in Tokyo. “It’s an extremely attractive proposition to a small biotech.” Already, foreign companies, including Athersys, TiGenix, and Pluristem, are looking to debut new drugs in Japan and collaborating with companies there to create new regenerative medicines.
So far, only three treatments have earned conditional approval, but the government aims to add to the list. Japan’s economic development ministry has estimated that regenerative medicine will be a $10 billion market in the country by 2030.
As Japan opened the door wide for regenerative medicines, it also let in a flood of criticism. A news piece in Nature in January revealed the depth of the concerns, pulling together stunned reactions from 10 experts. The researchers criticized multiple aspects of the trial: its small size (13 patients), its lack of blinding and placebos (everyone involved knew the subjects received an experimental treatment), its unconvincing explanation (one supposed mechanism was discounted by researchers years ago), and the fact that its results, while publicized in the media, were not published in a journal.
“This approval is an unfortunate step away from everything researchers have learned over the past 70 years about how to conduct a valid clinical trial,” James Guest, a neurosurgeon at the University of Miami, told Nature.
What’s more, UCLA neurologist Bruce Dobkin told Undark, the results briefly reported in the media may suggest the treatment doesn’t even work. Dobkin pointed to previous trials testing other potential treatments for spinal cord injuries, and the Stemirac findings “are exactly the results we found in patients in randomized controlled trials — in the control groups,” he said. That is, patients injected with Stemirac seemed to do as well as patients who got placebos in these earlier trials. He says people who have recently suffered spinal cord injuries, like Kusachi, the injured high diver, and the others in the Stemirac trial, often have significant natural improvement over the next several months — exactly the period covered by the trial. It’s possible the patients were simply healing naturally, he says, but without a control group and double-blinding, it is hard to tell.
Sipp said this problem was preventable. The researchers “could have easily used a placebo,” he said. “Stemirac is an infusion” — simple to fake for a placebo group. “Why didn’t they? They said they didn’t need to do it to get conditional approval.”
Japan’s approval system also lacked transparency, which invited more criticism. “The most serious problem of the Sapporo Medical [University] group is that they have not published enough data about the spinal cord injury treatment,” said Norio Nakatsuji, a long-time stem cell researcher at Kyoto University. “In any case, treatment has been carried out only in one hospital by one group. The conditionally approved trial will be also at only the same hospital. Thus, lack of transparency and opportunity of critical examination and discussion of the medical data is worrying.”
The Sapporo researchers declined to publish their results at the request of the Japanese health ministry, reportedly because officials said doing so could constitute promotion of the treatment. Yet the Stemirac researchers and trial patients — including Kusachi — participated in a documentary on NHK, Japan’s public broadcaster, hailing the treatment as a wondrous medical revolution. The documentary closes with a narrator saying: “What was once lost has been recovered. The era of regenerative medicine is here.”
Some experts were unimpressed or even alarmed by the documentary. For instance, Jun Takahashi, a stem cell researcher at Kyoto University, tweeted that “the treatment of the science-related content seems indulgent and overly optimistic,” before launching into a tweet thread criticizing various parts of the Stemirac study. A Nature editorial published in January said that publicly promoting Stemirac while declining to publish the data in a journal was “Kafkaesque.”
Considering the lack of solid evidence in initial fast-track studies, their success may come down to how well drugs are studied after the conditional approval, when researchers are supposed to justify permanent approval. But this approach has a spotty track record. “Post-marketing study is a pain in the ass, and it’s rightly called PMS,” said Novick. Last year, an Undark investigation found that drugmakers frequently fail to perform the follow-up studies they promise to, while “the FDA seems to be paying scant attention.” The Japanese government has laid out some principles for studying regenerative medicines after conditional approval, but the process doesn’t seem to require large randomized controlled trials.
Historically, without those trials, it’s been difficult to resolve questions about whether a drug truly works. For instance, decades after the FDA’s initial opposition to advertising aspirin for heart health, a series of clinical studies finally bore out the agency’s position. The FDA’s ban on advertising aspirin didn’t, it seems, kill tens of thousands of people, as Klein argued in 2000. And in 2004, Merck had to pull the popular pain medication Vioxx off the market when a new randomized, controlled trial with more than 2,500 subjects showed that it nearly doubled the likelihood of heart attacks and strokes. An official in the FDA’s Office of Drug Safety estimated that Vioxx killed up to 55,000 people.
If regenerative medicines like Stemirac don’t go through similar large, controlled studies, it’s possible that the public will never know whether they truly work or have any side effects.
Though the specifics of Japan’s fast-track system are unique, the country isn’t alone in relaxing drug regulations. Ever since Friedman questioned the need for the FDA in the 1970s, the agency has faced a rising drumbeat of calls to get out of the way. This reached a crescendo in the 1980s, when patients were desperate for any treatment that could slow the progression of AIDS. After sharp and public criticism, the FDA created Parallel Track, a scheme that let patients with AIDS take experimental drugs, and launched a similar program called Expanded Access — often referred to as compassionate use — for other terminal diseases.
Since then, the FDA has created a patchwork of alternative pathways to speed up drug approval: Fast Track, Priority Review, Breakthrough Therapy, and Accelerated Approval, the last of which shares features with Japan’s conditional approval structure. Congress has also picked up the deregulatory banner. In 2016, for instance, it passed the 21st Century Cures Act, which created a new category for promising regenerative medicines and may accelerate commercialization. And last year, President Trump signed the Right to Try Act, which, like compassionate use, aims to provide experimental medicines to people with hard-to-treat diseases.
These changes are part of a broader shift away from regulation, as the FDA has dramatically loosened rules on dietary supplements, drug advertising, and stem cell clinics, the latter of which have spread across the country with barely any regulatory oversight. The treatments have little research backing and most experts think they’re wholly ineffective.
“What breaks my heart is that people who are hard-working are doing crowdfunding, asking their neighbors, their families and friends for money to go down to the mall, to clinics where stem cells are advertised in the newspaper, and get their osteoarthritis treated, or indeed their migraines, or their kid’s autism, or cerebral palsy,” University of Sydney stem cell researcher John Rasko told Medscape in February. “They’re treated at $5,000, $10,000, $20,000 a pop.” By absorbing those health care dollars, bunk treatments can crowd out effective ones. “If you’re spending it on futile therapeutics that have never been proven, then you ain’t spending it on things that I would suggest are going to do better,” Rasko said.
Deregulation has also changed people’s relationships to medicine. Patients are now health care consumers and have more say over their medical decisions than at any other time in the modern era, giving the freedom to pursue pointless treatments and a powerful voice to demand them. “Recently I’ve gotten many emails that reflect almost entitlement. ‘Why do I have to go to Mexico? Why can’t I do this in the U.S.?” said Kriegstein. “Patients feel they have a right to these treatments even before they’ve been shown to be effective. I think that kind of attitude can actually change policy on a federal level, and I see this as a very alarming trend.”
The freedom to choose medicine also comes with the freedom of providers to market specious drugs, which “engenders false hope in miracle cures and leads to cynicism about the value of research,” wrote Sipp, Rasko, and another colleague in a comment in Nature in 2017.
Considering the trends toward individual choice, the move toward deregulation won’t likely abate anytime soon. Yoshihide Esaki, a senior member of the Japanese economic development ministry who helped create the expedited system, says the government is looking to expand it to all medicines. “This time we focused on regenerative medicine, but this was only a first step to changing the medical field,” he said in an interview at an industry conference in 2015. “Our next target is changing the total system for clinical trials.”
Free market advocates are using Japan’s example to try to open up the American system even more. “The U.S. can continue to pass occasional legislation that does not encounter much political opposition and makes small incremental improvements. If so, we can get ready for worldwide leadership in biopharmaceutical research to begin shifting to Japan,” wrote Madden, the author of “Free to Choose Medicine,” and Nobel-winning economist Vernon Smith in a 2015 Forbes column.
The free market advocacy is gaining traction. In a Heartland Institute policy brief published in March, Edward Hudgins called on the FDA to enact Free to Choose Medicine, which would, among other things, effectively expand the AIDS Parallel Track and get experimental drugs to patients with “debilitating diseases” like “Alzheimer’s, ALS, Parkinson’s, cancers of various kinds.” Soon after, Ted Cruz and three other U.S. Senators wrote a letter to the FDA calling on it to expand the AIDS Parallel Track to get experimental drugs to patients with “devastating diseases” like “Alzheimer’s disease, cancer, and amyotrophic lateral sclerosis (ALS).”
It’s hard to say how far this change will go in Japan or in the U.S., but it’s clear the balance is tipping from skepticism and a focus on patients toward boosterism and a focus on consumers. “If the U.S. ramps up approvals, Japan might respond with more,” said Sipp. “A race to the bottom would be serious and very bad; we could go back to the days when most medical products didn’t work.”
Amos Zeeberg is a freelance journalist based in Phnom Penh, Cambodia, whose work has appeared in publications including The New Yorker, The Atlantic, and Discover.
Reporting for this story was supported by the Abe Fellowship for Journalists, a reporting grant from the Social Science Research Council, and the Japan Foundation Center for Global Partnership.










Comments are automatically closed one year after article publication. Archived comments are below.
I want stem cell therapy for my daughter who is diagnosed ASD.Where should I contact in Japan . Please help me. Does the government health insurance of japan cover the cost in actual..please reply.
Call the Mayo Clinic, both Rochester and Florida campuses. The Spine Center.
Why don’t you contact the Mayo Clinic? Doctor Wenchen Qu treated a paralyzed Australian surfer back in 2015. You can see the testimonials on YouTube. The Mayo Clinic has done many different trials with pretty good results. The Japanese treatment was also in cooperation with Yale.
My husband was diagnosed with ALS when he was 63 years. we visited Mayaka Natural Clinic Website and ordered their ALS/MND Formula, i am happy to report the treatment effectively treated and reversed his Amyotrophic Lateral Sclerosis (ALS), most of the symptoms stopped, he is able to walk and able to ride his treadmill again, he is pretty active now. visit www. mayakanaturalclinic .com
I see no contact information for either the Japanese researchers or anyone doing this or similar work in the U.S.. anyone know who to contact, preferably in the States? Polio survivor from 1955.
My husband is suffering from optic nerve atrophy in both the eyes. Do you also do stem cells for the eyes. Please reply.
I am a 51 year old female that just found out I have Motor Neuron Disease Parkinson’s about a year and half, but I have been having signs of it for years, tremors, depression, body weakness. ECT. I honestly don’t think my doctor was reading the signs because of my gender and age. A few years ago I had my shoulder lock up on me and I was sent to a P.T since x-rays didn’t show any physical damage. My shaking was getting worse and I began falling. Only when my speech became so bad that it brought concern to my dentist was Parkinson’s even considered. He phoned my doctor with his concerns about my shaking and balance problems. By this time I was forgoing shots in the back of my neck for back and neck pain to which once again I was sent to a P.T (although x-rays showed no damage) I was told I had a few spurs which were most likely causing the pain. Here I was feeling like my whole body was falling apart and doctor could not find anything wrong, maybe in was all in my head? My doctor even seemed annoyed with me and things just kept progressing and I just kept it to myself, why bother going through testing and them finding nothing? Well, it was after my second P.T called my doctor about the weakness in my legs and arms, by this time I have developed a gait in my walk and I fell more frequently. Only then did my doctor send me to a specialist and it was found that I had Parkinson’s, and that I have had it for awhile. I think because I was a woman that my signs and symptoms weren’t taken seriously and therefor left untreated for so long,I was taking pramipexole dihydrochloride three times daily, I Was on carbidopa levodopa but only lasted 90 minutes then wore off.I found that none of the current medications worked effective for me.I got tired of using those medication so I decided to apply natural herbs formula that was prescribed to me by my second P.T, i purchase the herbal formula from totalcureherbsfoundation. com, There has been huge progression ever since I start the treatment plan which will last for 15 weeks usage.all the symptoms and sign has begin to disappear .
To Amos Zeeberg,
Thanks for a great article giving the proper scientific balance to the opposing views.
We dont see this often enough.
There is no substitute for trials that randomly allocate patients to treatment and placebo groups with neither the patients nor those conducting the trial being aware who is in which group.
Thanks for stating this point so clearly.
Ant deviation simply results in time money and effort wasted on treatments that almost certainly do not work and almost certainly have unknown side effects. A large majority of treatments that go through RCTs are either shown to be useless and/or have unacceptable side-effects. There is no reason this would not be true for treatments that never go through this process.
Do you think that the stem cells could help healing from the rare genetic disease HIBM? Is there any chance?
I have the adipose stem cells treatment and my knees and my knees pain are from 8 to 1. If it is due placebos effect, then I am happy about that.
Hello I’m Bharat from India. I have brain stroke right side paralysis.
My son: Silvan Prayogo is Biotech Scientist.
Under Grad in Mol Bio and Bio Chem of Colorado State Univ. Fort Collins/USA (2003) and MASTER in mammalian Cells Culture from Univ.of New South Wales Australia (2005)
This moment/since 5 YEARS ago live in TOKYO.
He could speak Japanese.
This moment he work in Berlitz Company as Private English Teacher.
He is still looking work in Biotech’s field (improve knowledge and business) , and possibly as volunteer.
He is interested study /learn about IPS Cells , but not yet get the opportunity.
I am very happy supposed Company / University in Japan/ Tokyo could help him using his knowledge to work for humanity (non profit work etc) to avoid his effort study in Biotech field become useless……….
Let me know or contact his email:……[email protected]………/my email:…[email protected]……
Dr Harry Prayogo
Contact your state and federal representatives via phone, email and social media immediately. Tell them you want stem cell therapy available and covered by Medicare NOW. Contact the FDA and do the same. We cannot wait to be healed. Keep contacting them until you get a response. Tell everyone you know to do the same. Be relentless. Change can happen sooner than you think.
“Ever since Friedman questioned the need for the FDA in the 1970s, the agency has faced a rising drumbeat of calls to get out of the way. This reached a crescendo in the 1980s, when patients were desperate for any treatment that could slow the progression of AIDS. After sharp and public criticism, the FDA created Parallel Track, a scheme that let patients with AIDS take experimental drugs, and launched a similar program called Expanded Access — often referred to as compassionate use — for other terminal diseases.”
In fact, FDA has allowed access to unapproved drugs, outside of clinical trials for the purpose of treatment of cancer and cardiac disease since the 1970s – prior to the AIDS epidemic. “Expanded access” was codified in FDA’s regulations in 1987 to treat patients with serious or life-threatening diseases (including HIV/AIDS), who had exhausted or were intolerant of approved therapies – if companies were able and willing to provide the investigational therapeutic product.
Parallel Track followed, in 1992, and was a policy (not a regulation) – restricted solely to use in AIDS – and was never codified into regulation. It was used only once, for d4T (stavudine).
Accelerated Approval, which is essentially a tentative approval based on surrogate markers likely to predict a clinical benefit was also initiated in 1992, and has been very successful at getting important therapies to market earlier – while drug developers are required to conduct continuing trials to show that the treatment really does have a meaningful clinical outcome for patients. Accelerated Approval contains a component that permits rapid removal from the market of drugs ultimately not shown to be clinically effective.
Free-market libertarians are increasing pressure, and using vulnerable patients as levers to loosen regulatory requirements. As FDA is pushed to further loosen requirements to show safety and effectiveness, the US could become a nation where social media bots will guide people to expensive treatments that don’t work, and to believe it’s their right to access unproven, and sometimes meaningless therapies.
Many patients and families would much rather believe that an unproven therapy will work than face the reality that there are no viable medical options left to them.
Unscrupulous charlatans, rather than patients, are the ones that will reap the benefits from the kind of drug development scenarios described in this article.
Please I require more information about stem cell treatment. Because my husband has a spinal code injury. And his age is too small 37 years.
Try Stem Cell Institute, Dr. Meser in Costa Rica. He has a lot of good testimonials, and two have had spinal cord injuries. I have CIDP, and will be trying it myself next week. What do we have to lose when there is no cure otherwise?
The Mayo Clinic has done a number of trials and does stem cells transplant in the spine. They have a Spine Centered
I’m very sorry to hear about your husband. The treatment mentioned in the article is only available in Japan. I can’t give medical advice and wouldn’t comment about specific treatments, but I can tell you that in general, treatments that are tested rigorously through randomized controlled clinical trials (RCTs) are much more likely to work than ones that haven’t been tested that way.
People who sell stem cell treatments at clinics may have the best of intentions, but they usually don’t have good evidence that those treatments work.
Why don’t you contact the Mayo Clinic? Doctor Wenchen Qu treated a paralyzed Australian surfer back in 2015. You can see the testimonials on YouTube. The Mayo Clinic has done many different trials with pretty good results. The Japanese treatment was also in cooperation with Yale.
Regarding the FDA? Big Pharma and big politics? They work in unison, and not with complete transparency, integrity, nor for the good of mankind -but, self preservation and profit before people.
Spent my lifetime in healthcare, 11 years in the pharmaceutical industry, BS was a premedical curriculum…Just to mention a few of my qualifications to comment.
Thanks for the comment. There are certainly flaws in the US pharma system, but there’s a lot of good that comes out of it, too, and many people working hard to help the ill—such as you, it sounds like.
Money-making scam for charlatans and quacks. Bogus trial to fast-track so they can hook more victims. Stem cell therapy is only approved for blood cancers, nothing else. Seems the majority of these scammers just happen to be chiropractors.
I don’t think so. I have a friend who did a stem cell treatment in her hip several years ago and her MRI shows regrowth. The Mayo Clinic has done extensive research and proven that it works. The main doctor is called Wenchen Qu and is in the Florida campus now. Rochester also does it. The same friend did a knee 3 days ago in Florida. We will see about that. If hyaluronic acid is now accepted as well as PRP, the logic is that stem cells transplant should work.
Yale was involved in the Japan trials, you can find it on Yale News.
please let this be what I’m praying for. I know American spinal cord research is useless because they only focus on making money but this country is very advanced and intelligent.
I’ve been a nurse’s aide for 32 years. And I believe that stem cell therapy is the wave of the future. Saying that I’m begging to be put on any research trial anyways I want any kind of way I want to receive the stem cells please help me my body does not make enough bone marrow so my bones are deteriorating at a rapid pace any help would be greatly appreciated why does it always have to be about money can’t you doctors help just one person just one let it be me I have five children three grands and I know that if I get the stem cell therapy I might have a chance to be able to walk and live a normal life please help me.
I hope something does come through to help you have a satisfying life, Donna. I don’t know if there are any treatments yet for your condition, but there are promising stem cell treatments being tested for some illnesses and a lot of doctors working hard to help cure people.
When will it be available for the public use