It’s Time to Begin Socializing Drug Development
My daughter lay prostrate and feverish on the floor of the hut, deep in Iban territory in Borneo and far from any modern medical facilities. Our interpreter informed us that one of the guides was a shaman. If we were agreeable, he would be honored to treat Leah. But first we should give him money. It was not payment for services — it was to make the medicine more powerful.

We might smile at such a primitive notion, but faith in the power of money pervades our modern medical system. All good capitalists believe devoutly in an Invisible Hand which wisely guides our choices in drug development. Nowhere is this faith more misplaced than for the development of medicines that treat and prevent infectious diseases.
Even today, as infectious diseases kill more than 9 million people worldwide each year, antibiotic development is moribund, abandoned by Big Pharma as a money-losing enterprise. New antivirals are being developed, but with ungodly price tags. Vaccine development has been revived, but only through an unstable combination of nonprofit efforts, government incentives and unprecedented prices. Pharmaceutical companies aren’t evil (usually). They just choose to make the most profitable drugs, not the drugs of greatest value to society. That’s why it’s time to begin socializing drug development — and we only need to look back at the trajectory of disease discovery and medicine development to see why.
Once the Malthusian Trap was sprung and the Industrial Revolution launched, control of contagion was required to sustain a culture of growth. The critical mass of modern cities was first purchased with the lives of dispossessed peasants: deaths from urban infectious diseases outpaced births, and cities’ populations were sustained only by continual immigration. Fortunately, we discovered germs and learned to tame them before we ran out of peasants. Clean water, vaccines and, eventually, antibiotics cut deaths from infection by a factor of 20 and enabled the demographic transition.
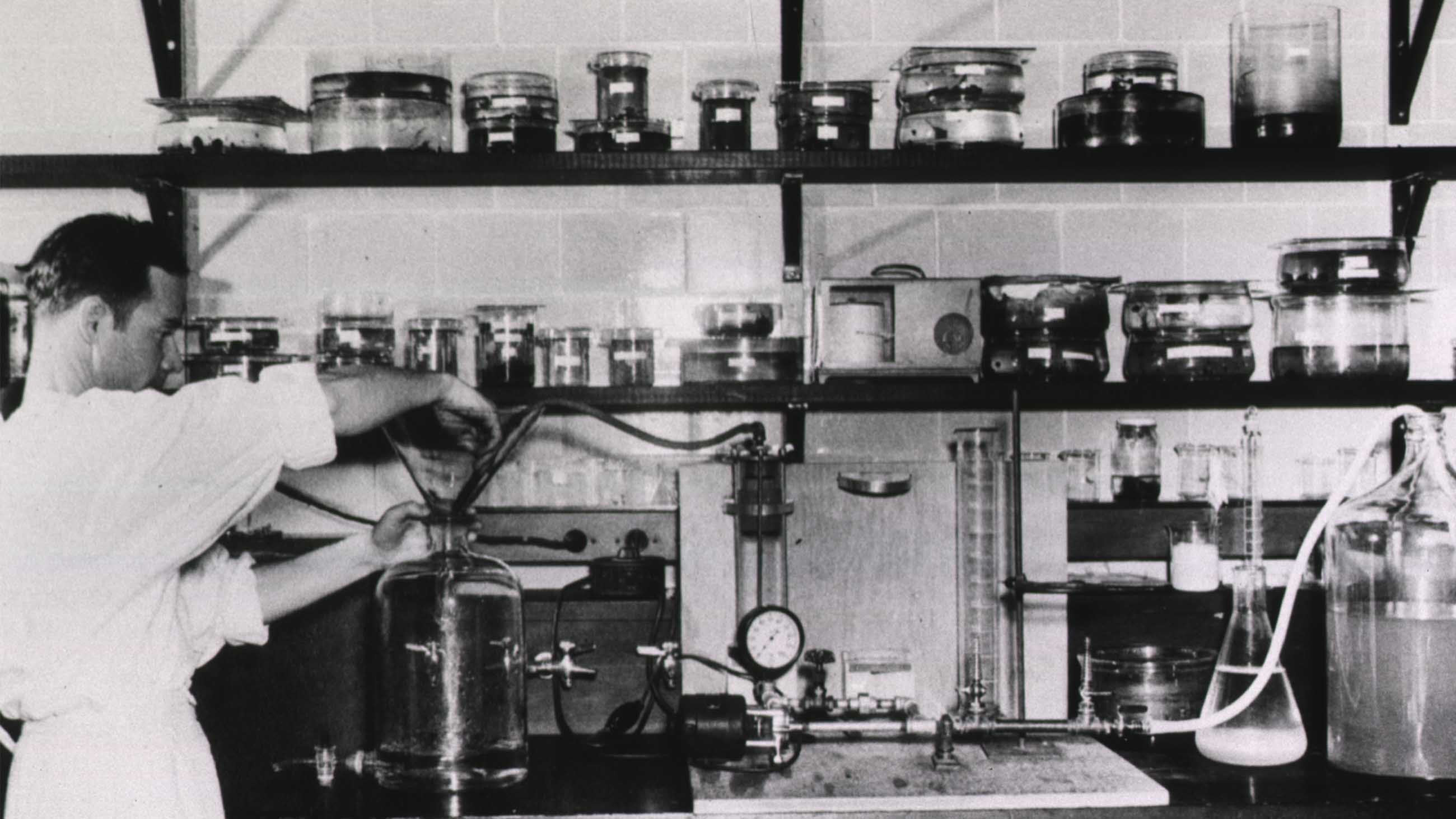
Free markets and profits were directly responsible for exactly none of these world-changing advances.
Academics discovered the anti-sera that cut deaths from diphtheria and tetanus in half. Produced by urban health departments which maintained stables of retired police horses for this purpose, they were distributed to citizens without regard for ability to pay. Likewise, the city fathers of Frankfurt funded development of the first antibiotic, the anti-syphilitic Salvarsan in 1909. The rich of that era were no nobler than of ours, but knew from personal experience that infectious diseases were no respecters of class
Vaccines, too, have a history of successful socialized development. In 1813, the U.S. Congress decided that all citizens were entitled to protection from smallpox, and could have the vaccine mailed to them free of charge. Nearly all the vaccines that make cities safe and livable — cholera, typhoid, pertussis, diphtheria, polio — were developed by nonprofits and were commonly made available to all. Indeed, Jonas Salk scoffed at the notion that his polio vaccine should even be patented: [It belongs to] “the people … ” he once said. “Could you patent the sun?”
Today, pharmaceutical companies have largely abandoned new antibiotic development on the eminently sensible principle that they are money-losers. Promising narrow-spectrum antibiotics — agents that precisely target pathogens and spare “good” bacteria — languish in development limbo because there is no hope that they might turn a profit. Old but effective antibiotics oscillate through wild price swings as manufacturers drop out and create monopoly pricing opportunities. Antibiotic development suffers from too much market freedom, not from too little.
Antibiotic and vaccine discovery and development are mature sciences; progress is more a matter of hard work than of breakthroughs — with few incentives. Innovation is still important, but not as important as the alignment of development efforts with societal needs. This means creating and providing vaccines to all, so that epidemics do not fulminate among the disadvantaged. It means creating narrow-spectrum antibiotics with small markets but large societal benefits. It means restricting the indiscriminate use of antibiotics so that they retain their potency. Markets fail to address all these needs.
In the U.S., the NIH already sets the agenda of new drug innovation by funding basic research — the phase that is highest-risk and most likely to fail. The subsequent phases of development — preclinical pharmacology and toxicology; chemistry, manufacturing, and control; and clinical testing — are well-defined disciplines. Drug companies perform no magic here but routinely contract out these functions to independent organizations. The NIH is as capable of writing these checks as any for-profit entity. But it, unlike pharma, has a mandate to write checks that improve public health, not private wealth. This approach won’t preclude for-profit drug development by private entities; it will just minimize the market-created gaps in our defenses against contagion.
The coming disruption in pharma will force drug makers to focus even more on short-term profits and their own survival. We cannot sacrifice our freedom from plague to the gods of the market. We need a reliable supply of the medicines that make modern society possible.
And my daughter? She was cured by neither the shaman’s ancient smoke nor by our modern ciprofloxacin. A trip down the river to a government clinic for a dose of milk of magnesia — a nearly 200-year-old concoction never patented outside the U.K. by its inventor — restored her health.
Drew Smith is a molecular biologist and long-distance hiker who has held positions at several biotech and medical technology startups, most recently MicroPhage, Inc., which declared bankruptcy in 2012. He now writes about science and hiking at drewsmithblog.com.










Comments are automatically closed one year after article publication. Archived comments are below.
Cipro may have killed your daughter. I suspect we are all depleted of Magnesium on a cellular level. Big Pharma drugs deplete us from the magnesium…and our food doesn’t have enough in it.
https://www.10news.com/news/team-10/team-10-investigates-san-diegans-describe-popular-antibiotic-causing-devastating-side-effects?fbclid=IwAR0yNGMw3CbiwRaEr5sn5DQkXhYqqHS_b8ZdZuqBcXYzbTvxtYjqbdrgE8Y
In my opinion, in areas of drug development that are/were abandoned by pharmaceutical companies due to the lack of profits (i.e antibiotics), the government should step in and fund the research and development. But for other areas where there are high profits (i.e cancers, orphan diseases etc..), let the pharmaceutical companies invest in it. The reasons are followed;
1. With high profits, more money and talents will pour in to solve the problems and speed up the development process. For examples; twenty years ago HIV was like a death sentence, nowadays people with HIV live a normal life like other people with chronic diseases (diabetes, hypertension etc..). For Hepatitis C, now we have a cure. In cancers, the last few years we have so many drugs approved to prolong the lives of those who suffered. I can say we are near the cusp of curing cancers in the near future with so many pharmaceutical companies working on different targets against cancers.
2. With high profits, there are also high risk of failure; meaning loss of lot and lot of money! It’s better to be more conservative with tax money.
Just an opinion from an biotech investor. I’d lost so much money with a few of antibiotic companies that I had invested in. The drugs got approved but they don’t make profits because hospitals save them for last resorts, and insurers won’t covered them because of the high prices unless patients have tried all other options first. I’ve also lost a lot of money with startup biotech companies developing novel approaches for cancers but they failed in clinical trials. Once in a while, you get one or two successes and I think it’s worth it.
Alan D White, totalitarian China and Russia were such pathological tyrannies that I am not sure how much we could learn from them. A better example might be Cuba, which has a fairly advanced biotech sector, along with a health care delivery system which outperforms that of the US in many metrics. That said, I don’t know much about the details of biotech in Cuba, but maybe I should educate myself. Thanks for the prompt.
Richk, the role of universities – funded almost entirely by the NIH – is to make fundamental discoveries. University researchers typically enable drug development by elucidating the mechanisms of disease, discovering molecular targets and discovering new chemical or biological entities that can be developed into drugs. Since the implementation of the Bayh-Dole Act of 1980, academic researchers have often created startups to develop and monetize their discoveries.
Universities rarely take these initial discoveries through the hard, crushingly complex and incredibly frustrating work of creating safe and effective drugs. They get to do the fun stuff instead.
Socialized drug development could proceed via a couple of paths. One would be to set up an institute within NIH to do the stuff needed to take initial discoveries all the way through approval: medicinal chemistry, pharmacokinetics, animal testing, clinical testing, regulatory filing. This would be a huge undertaking.
It would also duplicate the very capable infrastructure and expertise already developed by drug companies and contract research organizations. A better approach would be simply to contract with these entities to develop drugs.
Salk’s polio vaccine research and development was funded by the March of Dimes, the the 1950’s equivalent of Kickstarter/GoFundMe. https://en.wikipedia.org/wiki/March_of_Dimes
Great article. What is the role of universities?
Drew Smith, “well said”,
Who paid Salk’s salary ?
USSR and Red China are both excellent examples to look into for evidence that socialized research and production of antibiotics and pharms is best done in a socialized society or a free society. The record should be available unless the outcome was quite negative…
Fay, the GAIN Act and other measures already attempt to improve the profitability of antibiotic R&D, but they are half measures. Ultimately profitability is a reflection of society’s values. We are much more frightened of cancer than we are of infection, and thus we will pay $100k and more for new cancer treatments that extend life by just a few months, while being unwilling to pay more than a few $1000 for a life saving antibiotic. Pharma companies merely react to this market reality.
Markets are just tools, and when one tool fails, you use another. Socialized drug development is just another tool.
Great piece. Thanks so much.
I have waited a long time to hear someone step up with this information in article form. I have wanted to ask my Congress people and senators why they did not mandate the pharmaceutical ccompanies for greater antibiotic science and production. I knew that antibiotics were a short time profit maker, and that profits were the reason the companies did not respond to the desperate need for production of new antibiotics.
But I did not know the rest of the information. Thank you for filling in the backstory. Now I can present a more logical case to those in power.