In all the arguments that erupted afterward, everyone agreed on this: The chickens gained weight.
It was Christmas Day, 1948. The streets of Pearl River, New York, a small town 20 miles northwest of Manhattan on the New Jersey border, were very quiet, and the halls of Lederle Laboratories even more so. There was a skeleton crew at the 500-acre campus: the minimum necessary number of laboratory staff nipping in and out to monitor equipment and make sure the experimental animals were fed.
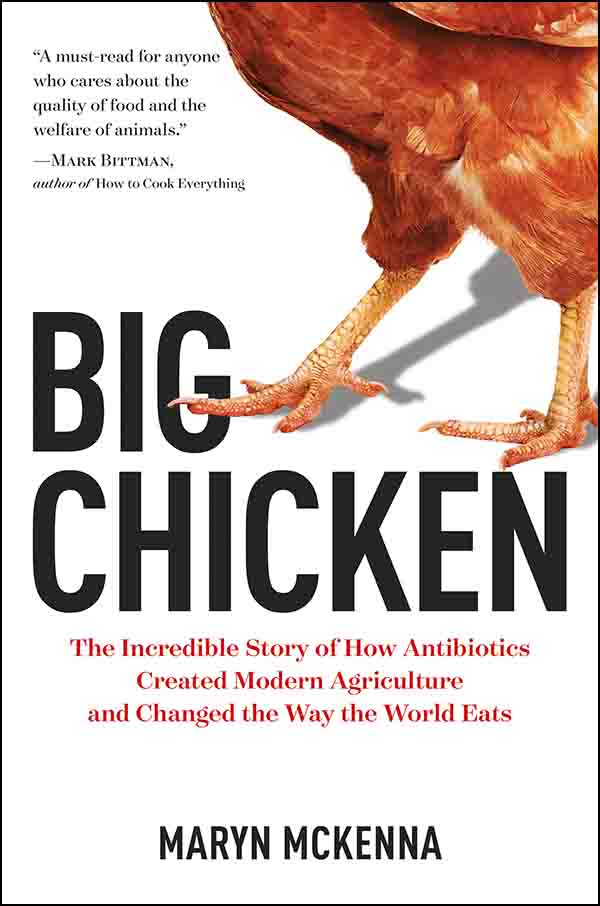
This article is excerpted from Maryn McKenna’s new book, “Big Chicken: The Incredible Story of How Antibiotics Created Modern Agriculture and Changed the Way the World Eats,” published by National Geographic.
Thomas Jukes did not plan to spend much time there himself. He had told his lab assistant to take the holiday off. All he needed was to slip into the animal colony, corner the 133 juvenile chickens that made up his experiment, and weigh them. He expected that it would not take long.
He probably did not expect to change the world.
Jukes was British, slender and dark-haired, with alert eyes behind oversized glasses: an energetic self-made man who had left home at age 17, emigrated to Canada, and worked on a farm and in factories in Detroit to amass enough money for college. He had earned a degree at Ontario Agriculture College — sleeping, at one point, on a cot in the poultry building — and a Ph.D. in biochemistry at the University of Toronto’s medical school, studying the immune systems of chickens and ducks. In 1933, he took a postdoctoral appointment at the University of California, Berkeley, and wound up at its College of Agriculture, where he accomplished notable work, identifying which vitamins had to be added to chicken feed to allow birds to thrive on a manufactured diet.
In the 1930s, that was a crucial question. Until World War I, almost every farmer had kept a few hens to produce eggs and had eaten the hens when they stopped laying. Now, though, chicken meat and eggs were becoming a crop, a farm’s reason for being. Instead of a few at a time, chickens were being raised by the thousands, and instead of wandering around a barnyard, they were sequestered indoors, unable to reach the grains and grubs they would have scratched up from the ground. They needed synthetic nutrition, and the poultry industry needed a parallel industry of experts to supply it.
Jukes became one of those experts, and Lederle, the company that recruited him from California with the promise of a lab and staff, was becoming a leader in poultry science. Lederle was not an agricultural company; it was a pharmaceutical company, one of the first manufacturers of antibiotics.
Jukes joined the company in 1942, the year the new drug called penicillin saved the lives of more than 100 victims of the Cocoanut Grove nightclub fire in Boston by preventing infections from taking hold in severe burns. That was enough proof of the power of this mold-based antibiotic for the U.S. government to invest in its production and send millions of doses out onto the battlefields of World War II, saving untold thousands with a speed that seemed miraculous.
An undated portrait of the scientist Thomas Jukes, who fed chickens Aureomycin to see if they’d grow.
Visual: Journal of Nutrition
Penicillin’s success ignited a hunger for additional antibiotics — and for the profit these new drugs could bring. Pharmaceutical companies sent sterile sample tubes around the world, begging missionaries and soldiers to spoon up and send home any mold or dirt that looked promising. Lederle’s chief pathologist, Benjamin Duggar, asked a former colleague at the University of Missouri to send him random scoops of dirt from the campus. One tube, dug from a field where the agricultural school grew varieties of forage grass, contained a bacterium that exuded a golden-yellow chemical. In tests, the compound killed a wide array of disease bacteria — more than penicillin could manage, and different ones from those that streptomycin could kill.
American Cyanamid Company, Lederle’s parent corporation, jubilantly filed for a patent in February 1948. In a nod to the compound’s color— and maybe to the income he hoped would flow from it — Duggar dubbed the fungus Streptomyces aureofaciens, “gold-making.” He called the compound Aureomycin. Later it would be known as chlortetracycline, the first of the entire family of tetracycline drugs.
Jukes was not part of Lederle’s antibiotic effort; he had been hired to work on nutrition. But he was still interested in what chickens needed to eat to thrive in confinement — and by an accident of history, that question was more important than ever. World War II had spurred such demand for protein that chicken production almost tripled. But when the war ended, the poultry market collapsed and producers struggled for ways to cut costs. En masse, they switched their birds’ diet from vitamin-rich fishmeal to much cheaper soybeans. Chickens did not do well on soybeans, though. They grew slowly; their eggs did not hatch. Even when vitamins were added to their feed, as Jukes had learned to do in his first job, the birds did not thrive. People talked about adding a nutritious boost, an “animal protein factor.”
Then Merck & Company, a Lederle rival, discovered that the brewing process for making its own antibiotic, streptomycin, produced a compound that made chickens do better, even when they were fed the small amounts of protein now present in conventional feed. Merck’s scientists identified the byproduct as vitamin B12.
Jukes wondered if Lederle’s Aureomycin, a distant relative of the bacteria species the Merck scientists used, could perform the same trick. That was what brought him to his office on Christmas morning, on a mild, dry day with just a dusting of snow. A few weeks earlier, he had set up an experiment to test whether Lederle possessed an animal protein factor of its own. Today he would find out.
He had chosen a small group of 6-month-old hens and roosters from the birds the company raised to use in research. He fed them a specially mixed diet, low in nutrients so the chicks would be feeble; that way, it would be easier to distinguish the effect of any additives. When the hens laid eggs, he hatched the chicks in an incubator, divided them into groups of 12, and sequestered one dozen to keep as a control group. Those birds got the same deficient diet as their parents. The other groups got different doses of supplements; one of those groups was fed tiny portions of the mash, or growth medium, that Aureomycin had been brewed in.
Christmas was the 25th day since the chicks had hatched. (Most of the control group had died.) One by one, Jukes weighed them all, painstakingly recording the numbers, then looked at his results. And looked again. The birds that had gotten the highest dose of Aureomycin were the heaviest in the room. They weighed almost 10 ounces — a third more than the chicks receiving Merck’s B12.
The chicks had gotten to that weight with the help of 60 grams of the mash containing a trace amount of Aureomycin. Sixty grams is 2 ounces: the weight of a handful of pennies, two slices of bread, an egg. Yet that tiny weight would exert enough force to alter the entire structure of agriculture — and affect land use, labor relations, international trade, animal welfare, and the diet of most of the world.
As further experiments confirmed Aureomycin’s “growth-promoting” effect, Jukes began passing samples to scientists he knew at state agricultural colleges throughout the United States and asked them to conduct experiments of their own. His colleagues were astounded: They reported back that small doses not only cured a bloody diarrhea that would have killed young pigs, but also tripled their rate of growth and boosted the weight of turkey chicks, called poults.
Word got around. So many researchers asked for Aureomycin residue that Jukes ran through the Pearl River plant’s fermentation byproducts faster than they were being made. He resorted to plundering the company dump for any discarded fermentation vessels, including reused glass Coke bottles, that might contain a few precious grams of drug.
Farmers began clamoring for it too. Demand was so intense that a senator from Nebraska sent an official complaint that the farmers in neighboring Iowa were getting more of the product than his own constituents. Vice President Alben Barkley requested and received a load to feed to livestock on his family’s Kentucky farm.
As a pharmaceutical manufacturer, Lederle had to report any new drug and any new use of a drug to the Food and Drug Administration. It had done that when Aureomycin was first achieved, registering it appropriately as a human medication. But when it came to animal feed, the company was cagey, calling it a vitamin supplement. (A 1949 patent application for Aureomycin in animal feed, describing it as a drug and not a “source of vitamin B12,” proves it knew better.) Jukes and his colleague E.L. Robert Stokstad did not publicly acknowledge how their discovery worked until April 1950, at the annual meeting of the American Chemical Society. A New York Times reporter happened to be covering the conference. The following morning, his story trumpeted the news on the front page: “‘Wonder Drug’ Aureomycin Found to Spur Growth 50%.”
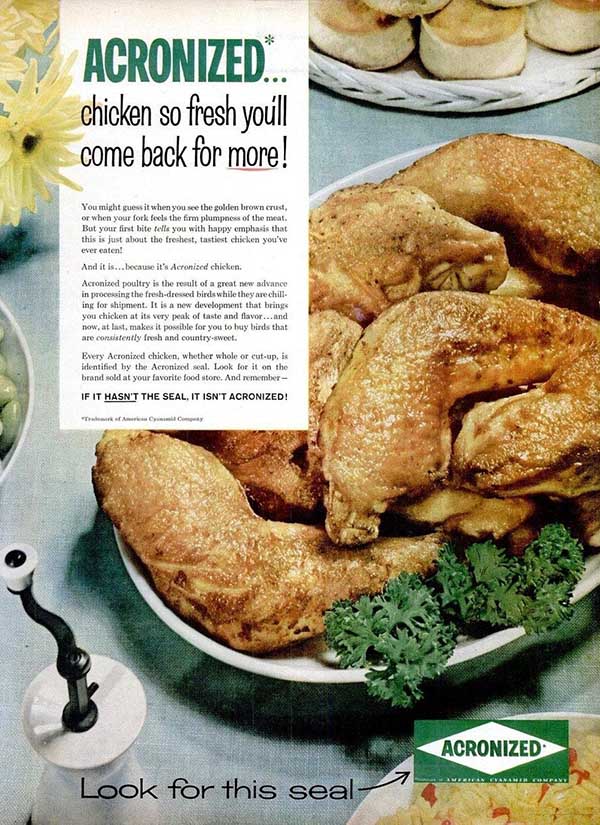
In a 1956 ad, Lederle boasted that its Acronizing process — dunking raw meat into an antibiotic solution — “brings you chicken at its very peak of taste and flavor.”
The story contained a clue as to why Aureomycin had become so popular: It was cheap. “Five pounds of an unpurified product, selling at 30 to 40 cents a pound, when added to a whole ton of animal feed . . . ‘has increased the rate of growth of hogs by as much as 50 per cent,’” it said. And it ended by declaring, with a boldness that would turn out to be overconfident: “No undesirable side effects have been observed.”
In retrospect, such statements sound startling. But they make sense in the context of the time. Antibiotics were new, and the world was in love with them.
There was a reason they were called miracle drugs. Before penicillin, minor cuts and scrapes often burgeoned into infections so serious they required amputations. Three out of every 10 pneumonia patients died; so did nine women out of every 1,000 who gave birth. (That was in the cleanest hospitals; often the death toll was higher.) Untreated ear infections ravaged children’s hearing. One out of every six soldiers wounded on the battlefield died there, and huge numbers contracted syphilis and gonorrhea that left them disabled, arthritic, or blind.
The relief of being freed from that burden sparked a joyous overreaction. Penicillin was not only dispensed to patients in hospitals; manufacturers tossed it into ointments, throat lozenges, gum, toothpaste, inhalable powders, even lipstick. Anyone could buy penicillin over the counter in a pharmacy; prescriptions were not required until 1951 (and even then only because overuse was provoking allergies). There was no understanding yet that antibiotics work only against bacterial diseases, not viruses. It seemed only smart to take the new drugs for any ailment — foolish, in fact, not to.
Yet from the early days of the antibiotic era, there had been rumblings of concern about how long their effectiveness would last. In 1945, a few months before receiving the Nobel Prize in Medicine for discovering penicillin, the Scottish scientist Alexander Fleming warned against its use in too small doses, “so that, instead of clearing up the infection, the microbes are educated to resist penicillin.”
“In such a case,” he went on, “the thoughtless person playing with penicillin treatment is morally responsible for the death of the man who finally succumbs to infection with the penicillin-resistant organism. I hope this evil can be averted.”
Fleming was prescient, and unheeded. By 1947, a hospital in London was experiencing an outbreak of staph infections that did not respond to penicillin. By 1953, the same resistant bug sparked an epidemic in Australia, and in 1955 it crossed to the United States, infecting more than 5,000 mothers who had given birth in hospitals near Seattle and their newborns too. Those illnesses marked the start of the lethal game of leapfrog that organisms and antibiotics have engaged in ever since. Researchers direct a drug against them; they evolve a defense against it; other researchers produce a new drug; bacteria evolve a defense again.
The antibiotic doses being given to animals for growth promotion could not strictly be considered “too small,” but only because the animals were healthy and did not require a dose of any size. But the amounts being given were minuscule. Lederle veterinarians warned that the company’s new product would encourage antibiotic resistance, but they were overruled by its corporate parent, American Cyanamid. “Competition was right on our heels,” Jukes said three decades later.
The FDA took a similar attitude, accepting drug companies’ assertions that growth promoters were safe. In 1951, with no advance public notice and without holding a hearing, it approved Aureomycin and five other antibiotics for use in animal feed. The administrator of the Federal Security Administration, which oversaw the FDA at the time, said it “would be against public interest to delay.”
Even as antibiotics were catching on as growth promoters in animals, researchers began to wonder whether they would do the same for humans. Between 1950 and 1955, experimenters fed routine doses of antibiotics to small groups of premature babies. Other researchers concocted other human trials that are unnerving by modern ethical standards. Antibiotics were given to people who had no capacity to consent, including developmentally disabled children held in a eugenics institution in Florida and undernourished poor children in Guatemala and Kenya. Fortunately for the subjects, none of the trials reported adverse effects, and in all of them the growth promoters worked. All of the recipients, adults and children, put on muscle, and the children grew taller as well.
Those results made researchers even more confident that antibiotics in animals had no negative effects, and that led in turn to the drugs’ most out-there use: keeping food from going bad. In several countries, led by the United States, experimenters added antibiotics to the cold-water tanks in which fish were held on fishing boats and to the ice on which fish were stored in processing plants. They washed spinach in a streptomycin solution after harvesting. They painted the drugs on the outside of cuts of meat and mixed them into ground beef. (Such practices did not last long, but a Lederle process called Acronizing —dunking raw chicken and fish into an antibiotic solution — persisted for a decade.)
The experiments led to a kind of category creep for Aureomycin. The drug that had first been used only to make animals grow faster began to be used to protect them from diseases as well. This required a larger dose. Lederle salesmen began to tell farmers that they should give chickens not 10 grams of Aureomycin per ton of feed but up to 200 grams, a 20-fold increase. The FDA blessed the practice in April 1953, extending approval of Aureomycin from just growth promotion to prevention as well—once more without any advance notice and without a public hearing.

Visual courtesy of New City Library postcard collection
This was huge — and not just for Lederle, which could instantly count on bigger sales. It gave farmers permission to use antibiotics far more freely, insulating unscrupulous or inexperienced or careless producers from the consequences of bad farming practices. They could squeeze animals in more tightly, clean their barns less frequently, scrimp on nutrition, turn a blind eye to pests — and know they were protected against the diseases that would otherwise have resulted, because the antibiotic doses protected their livestock from the start. The decision opened the door to industrial-scale production and the animal welfare abuses it would one day be accused of. And though it would take years before anyone put the pieces together, it would increase antibiotic resistance as well. (Using antibiotics to promote growth in animals did not end in this country until 2017. Preventive use is still allowed.)
To the end of his life — he died in 1999, at 93 — Jukes championed his invention and refused to acknowledge any downside. That may have been possessiveness, or arrogance, or just cussedness: He seems to have taken pleasure in defying received wisdom. He derided regulation of dangerous food additives and called organic food a “myth.” He opposed federal action that prevented beef cattle from getting the estrogen compound DES, even though it was known to cause cancer in the daughters of women who were given it in pregnancy. He directed special rage at the ban on the pesticide DDT and the hugely influential 1962 book “Silent Spring,” which provoked it. He railed that the federal government had caved to “that segment of society represented by the antivivisectionists, anti-fluoridationists, and organic farmers.” In a parody published in the journal Chemical Week, he mocked its author, Rachel Carson, as a writer of “science fiction horror stories.”
Writing for both scientific journals and newspapers — his zestful polemics appeared, among other places, in Science, Nature, the Journal of the American Medical Association, and The New York Times — Jukes dismissed any concerns about livestock antibiotics and the concentrated confinement farms they would create. “The use of antibiotics for farm animals does not present a hazard to public health,” he declared in the New England Journal of Medicine in 1970. Appearing at the New York Academy of Sciences in 1971, he asked: “Do we have so many cattle, pigs, and chickens that we ignore the need for feeding them by the most economical means? I do not think so.”
And later: “The urban public has been encouraged by the animal-rights movement to believe that animals ‘feel better’ when they have more space for roaming. But how do we know this is true? Humans voluntarily jam themselves together to watch sports or in social gatherings. The larger and denser the crowd, the more successful the event.” He wrote that in 1992, at age 86. It may have been his last public word on the subject.
Maryn McKenna is a freelancer focused on public health, global health, and food policy, and a senior fellow of the Schuster Institute for Investigative Journalism at Brandeis University. A former Knight Science Journalism fellow at MIT, she delivered a TED Talk, “What do we do when antibiotics don’t work anymore?,” that has been viewed more than 1.5 million times.










Comments are automatically closed one year after article publication. Archived comments are below.
I followed your directions for my chickens and am hoping for positive results. At the time I noticed the mites, I had my first hen go broody.
Jukes was right about Rachel Carson.
Carson comes up with illogical conclusions based upon studies that never were able to tie the thinning eggshells to predatory birds. In fact Carson’s book has caused more death than Hitler with the resurgence of Malaria due to the banning of DDT.
Go pick up your cheques boys, thanks….. The chemical and drug industry.
They speak (an obvious) truth and you respond with silly ad hominim attacks. Do you leftists ever actually think before you spew nonsense?
The people on the left spout semi informed ad hominim crap just as do people on the right… but typically with less malicious intent. The problem is that most people are too lazy or too stupid to read, understand, and interpret the raw data themselves, and when the people (left or right) that they trust push a position that is either biased or incompletely considered they latch onto the most dramatic interpretations promoted by the popular media.
For example: People on the left and the right each want to promote censorship which favors their respective belief structures in fear that someone who might be on their side today might have a change of heart. Fear of injustice to ones heart felt cause similarly creates blind intolerance of alternative perspectives. Certain drugs (like alcohol and marijuana) and sex workers are another example which, interestingly, generate hyperbole which crosses different boundaries. Liberals significantly overlap Libertarians until Liberals reach into socialism or Libertarians reach into unfettered social Darwinism.
In the case of chemicals and medications there is a lack of understanding which has resulted in fear of the unknown on the left and habitual trust from the right. Both positions are founded in ignorance because the reality is far more complex and nuanced, and it is (in fact) very difficult to figure out who to trust without first understanding the data… a challenging and time consuming task when so many people have an agenda which provide foundational bias.