In Australia, ‘Thunderstorm Asthma’ Fuels the Quest for a Cure
On a sweltering afternoon in November 2016, the Bureau of Meteorology in the Australian state of Victoria issued a severe thunderstorm warning for several regional areas around metropolitan Melbourne.
It was a relatively routine announcement for the time of the year. Thunderstorms are a common springtime occurrence in and around Australia’s second-largest city, whose famously changeable weather is said by locals to produce four seasons in a single day.
But as it turned out, the hours following the November 21 alert were anything but routine.
During that Monday evening and the following Tuesday, authorities were inundated with ambulance calls every few seconds, resulting in more than 8,500 people flooding into hospitals with respiratory difficulties. Health care workers were overwhelmed as emergency departments ran out of asthma inhalers and space to put new admissions. Victorian Health Minister Jill Hennessy would later liken the situation to “150 bombs going off at once.”
The issues — which would ultimately claim ten lives — turned out to be the result of a rare phenomenon known as “thunderstorm asthma.” Though still not fully understood, the weather event is thought to occur due to the spread of pollen and mold that gets swept into the high humidity of the clouds, broken into smaller particles, and rained back down. For a person with asthma — whose airways are chronically inflamed — the spread of these particles can set off an attack.
This unusual weather event is not unique to Melbourne. Along with a number of other Australian towns and cities, thunderstorm asthma cases have been recorded in the United States, the United Kingdom, Kuwait, and Iran. Still, the city is thought to be particularly susceptible due to its prevailing winds, heavy rainfall, and high pollen count. And while Melbourne has documented at least six thunderstorm asthma outbreaks in the last four decades, the 2016 episode was by far the most extreme ever seen, serving as a major wakeup call to authorities who had previously paid little attention to the issue.
Since then, the city has emerged at the vanguard of efforts to tackle the hazardous weather phenomenon and, more fundamentally, to develop a cure for asthma outright.
At the Walter and Eliza Hall Institute, an imposing multi-storied structure at the edge of Melbourne’s central business district, researchers are banking on the belief that the key to curing asthma lies in our DNA. Although DNA itself is stable, the epigenome, or genetic “punctuation,” which regulates which genes are activated at a particular moment, is affected by the environment.
Armed with this knowledge, a team led by Rhys Allan, an expert in molecular immunology, is carrying out research aimed at rewiring the circuitry of the immune cells that are triggered during an asthma attack. By erasing chemical tags on the cells through targeted drug therapy, Allan and his colleagues say they hope to be able to turn off the immune response that causes the symptoms in the first place.
“That is the idea, that you could actually switch those cells and stop them from being able to continually cause the disease,” Allan says, likening the immune system to memory. “The reprogramming works so effectively that you’ve now destabilized those cells and they are not able to remember.”
Allan says his team’s work on tackling asthma’s root cause is unique in its approach.
“What we are trying to do is understand the fundamental action of the immune system, how it works at the molecular level,” he says, noting that they are seeking to bypass the immune response, rather than boost it like many burgeoning cancer treatments.
Though deaths due to asthma are rare, Australia experiences about 400 each year — putting it at a higher rate than many other developed nations, including Sweden, Canada, and South Korea. The U.S. experiences a similar rate of deaths, the majority of which experts say could be prevented with proper medical care.
While there have been a limited number of studies on the relationship between asthma and thunderstorms outside of Australia, researchers at Emory University in Atlanta, Georgia, have documented a general link between the two, even outside of rare epidemic-level events. Stefanie Ebelt Sarnat, the associate professor of environmental health who led the work, says she believes the area requires far more research and sees promise in the work of her counterparts in Melbourne.
“For those people that don’t have a good asthma management plan or don’t have their medication figured out, they’re going to be more prone to being impacted by any environmental triggers or allergic triggers to their asthma,” she says. “So figuring out medications that help people, I think, that’s going to be a needed area.”
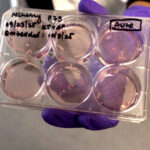
So far, Allan’s team has been successful at “short circuiting” asthma-causing cells in in vitro tests and experiments using mice. The hope is that human trials will be possible within a number of years.
“We know where the targets are, we know which ones to switch off,” Allan says. “We need to develop it so it’s more effective at this point.”
Most likely, treatment, possibly in the form of a pill, would be administered at the onset of symptoms, when the immune system has kicked into gear. As they replicate, cells would “unlearn” their asthmatic reaction, the theory goes, ultimately delivering a cure.
“Cells are more susceptible to being rewired when they are activated,” Allan points out.
If realized, Allan and others say, the breakthrough would mark an evolution in the treatment available to asthma sufferers, even if it remains a matter of debate which avenues hold the most potential for ending the condition as we know it.
According to Gary Stadtmauer, a New York-based allergist and immunologist, the best approach is primary prevention — “stopping the disease from ever developing.” The cost of drugs which would target immune responses, he argues, remains prohibitive.
Currently, sufferers rely on inhalers to treat symptoms as they occur or preventative steroids that require continual use to be effective. Up to 40 percent of those affected during the 2016 thunderstorm asthma epidemic were unaware they had asthma and many apparently had never suffered from the condition at all. Others took their preventative medication inconsistently due to a lack of regular symptoms.
“It’s intuitively unreasonable in my view to keep taking something that abolishes your symptoms, so people stop taking it all the time,” says Jo Douglass, an allergy specialist at the Royal Melbourne Hospital, noting that as many as one-third of preventative medication prescriptions go unfilled.
For clinicians such as her, a key challenge is trying to predict who might be most at risk from thunderstorm asthma, which as yet cannot be done with any certainty. Common among those sickened in last year’s event was high sensitivity to grass pollen, casting a light on a rarely examined link between allergies and asthma.
“It’s a natural experiment in a way because of the high prevalence of allergies and the catastrophic asthma that emerged,” Douglass, who is a member of a multi-disciplinary task force established to examine ways to better predict and treat thunderstorm asthma, says of the city. “The role of true allergic asthma in the overall picture of asthma is not completely clear.”
In the last year, state authorities have rolled out an early warning alert system and a GP-focused education campaign for thunderstorm asthma. During high-risk periods, asthma and allergy sufferers are advised to stay indoors and have their usual medications at the ready.
Despite Australia’s high mortality rate for the disease, Allan says, research into a cure hasn’t always gotten the attention it deserves.
“Allergic asthma has not been seen as that serious,” Allan says. “But it is serious.”
John Power is a journalist whose work has appeared in some three dozen media outlets including The Guardian, The Christian Science Monitor, Quartz, The Age, The South China Morning Post, The Irish Times, The Nikkei Asian Review, and Al Jazeera. Previously based in Seoul, South Korea, he currently reports from Melbourne, Australia.










Comments are automatically closed one year after article publication. Archived comments are below.
Australia does not have as much magnesium in water, soil etc as other parts of the world.
Magnesium deficiency is a factor in asthma, smooth muscle function etc (something that was well known and researched in 80s-90s).
Melbourne is magnesium deficient. For example, magnesium has been getting stripped out of Melb water over last decade, while chloroform has nearly doubled in the water in some areas.
Also the increasing chemical/industrial pollutants in the air from petro-chemical, military/RAAF, industry etc. Melbourne is a low lying/sea level area and the dense pressure system that accompanies thunderstorms, plus still air (insufficient ventilation) forces all those chemicals down. They’re not dispersed. Not dissimilar to chlorine poisoning (and herbicides that damage vegetation) that’s gone on in various wars.
The pollen theory – more specifically the breakdown of pollens – has not been substantiated/proven.
Instead of manipulating and modifying people to fit toxic environments so as to generate new revenue streams, bolster health with basic building blocks such as magnesium, potassium etc, and address the poisons in the atmosphere at real, practical level.
Btw, magnesium is also one of those basic elements that’s protective against various cancers. Is essential for lots of bodily functions.
Lightning produces ozone, which is a lung irritant. See: https://www.ncbi.nlm.nih.gov/pubmed/11493720
Despite any possible benefits, marijuana also has enormous risks for asthmatics, especially if you smoke it. Since, it can increase inflammation, making your asthma symptoms worse.
When you smoke marijuana, there are components called bullae that can build up in your lungs. These are large air sacs that can eventually disrupt your breathing. Manage your asthma proactively with RoundGlass Breathe
There is much misinformation about cannabis, which has been found to be helpful for asthma. See: https://www.ncbi.nlm.nih.gov/pubmed/1099949
I’d go to Australia to help with trials. May this team find a cure/switch to immune response. I’m feeling hopeful.
Cannabis may help its an anti-inflammatory. In my own personal experience if I have a cough sometimes I’ll smoke weed and it clears my chest and opens my airwaves. I know a lot of people will dismiss this but do your research before you do it has helped me so no reason why I will not help others
I agree. Since moving from London to Amsterdam where cannabis is regulated, my repeat prescriptions of Symbicort has gone down and now I take it once per day instead of 3 (due to attacks). Only thing that has changed is more and better Cannabis. 13 years proof out of 25 Years of Smoking.