If you look in the crisper drawer of my fridge, you won’t find much in the way of salad. Instead, the drawer is jam packed with something even more important to my health: insulin.
I am one of more than a million people in the U.S. with insulin-dependent diabetes. But like many others, I can’t afford the retail costs or copays for the medication that keeps me alive. During months when I teach as an adjunct professor and am covered by my university’s insurance plan, I stock up as much insulin as I can. During the remainder of the year, I do what thousands of others do: I cross the border to Mexico where, just 12 miles from my house in San Diego, I can buy the same medicine at one-tenth of the price.
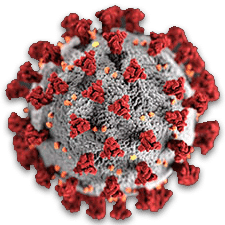
The U.S. International Trade Commission estimates that more than 952,000 Californians travel to Mexico each year for health care, including for prescription drugs. But now that the U.S.’s northern and southern borders have closed to nonessential travel as a result of the Covid-19 pandemic, lifelines to affordable medicine in Mexico in Canada have effectively been cut off. Just as American households are beginning to feel the pinch of a historic economic slowdown, many diabetes patients will be left with few if any options for obtaining affordable insulin.
Of course, Covid-19 didn’t cause this problem; it is merely revealing cracks in a broken drug development system that allows pharmaceutical companies to prioritize profit over patients. But the pandemic underscores the urgency of the problem — one that could easily be fixed if only politicians were willing to stand up to the drug manufacturing giants.
 |
Thoughts or questions on Covid-19? |
To understand why a short drive can be the difference between life and death for people with diabetes, you need to understand why insulin costs so much in the U.S. More than 90 percent of the global insulin supply is controlled by just three companies — Eli Lilly, Sanofi, and Novo Nordisk. These suppliers’ commonly exploit loopholes in U.S. patent law to prevent generic competition, and their insulin prices tend to increase in lockstep with one another. That, and the federal government’s unwillingness to regulate prices, may explain why the price of insulin in the U.S. has more than tripled over the last decade. In the U.S., a roughly weeklong supply of rapid-acting insulin, sold as a multidose pen, costs $133. In Canada, where drug prices are federally regulated, that same $133 can get you 13 pens. In Mexico, it can get you 10. In every case, the manufacturers reap handsome profits: A BMJ study estimates that a vial of insulin — about three pens’ worth — cost manufacturers between just $3.69 and $6.16 to produce.
Even for Americans who are covered by health insurance, high insulin prices can impose significant financial strain. Copays under Medicare Part D can range from $25 to $484 for a box of five pens of fast-acting insulin. (Currently, my copay is $110.) And in many cases, that insulin must be taken in conjunction with long-acting insulin, which can retail at around $170 for a supply that, for me, lasts only about two weeks. On top of that, there are out-of-pocket costs for needles, test strips, and sometimes oral medications, pumps, and glucose monitors. The American Diabetes Association estimates that, on average, a person with diabetes spends $9,601 out-of-pocket each year on treatments for the disease. People with insulin-dependent diabetes likely spend even more.
These high prices can cause more than financial ruin. In a survey of diabetes patients at the Yale Diabetes Center, 25 percent of the 199 respondents said they ration their medication to save on costs, a risky practice that can lead to dangerous health complications. During the last three years, at least 12 people in the U.S. have died because they could not afford insulin.
Faced with the prospects of rationing or bankruptcy, many Americans are opting instead to take a trip to the border. Caravans have been organized to shuttle people with diabetes to Canada to stock up on supplies. A nonprofit is recruiting volunteers to travel to Mexico to buy insulin to give away to strangers. Now that the U.S. borders have been effectively closed, these options have been taken off the table.
Without access to affordable insulin, many people with diabetes will panic. A lucky few will have stockpiled a supply before the pandemic hit, as I did. Others will resort to the sadly familiar technique of begging friends for spare insulin. I have, in the past, exaggerated my own insulin needs to my doctor in order to obtain surplus medication to give to friends. I’m already seeing insulin being shared among my friends locally. But “bumming some off a friend” is a way cheap kids score weed, not a sustainable or sensible way to ensure access to essential medicines.
Still other diabetes patients will change their eating habits, adopting a lower carbohydrate diet in order to stretch their supply of insulin. But these dietary changes, a form of rationing, can have devastating results as the person’s carbohydrate stores dwindle and their diabetes becomes more difficult to manage. A routine drop in blood sugar that might normally have been solved with a handful of jelly beans could become fatal.
So far, attempts to address insulin prices in the face of the Covid-19 pandemic have been piecemeal. Eli Lilly just announced that it will cap insulin copays at $35 per month using a complicated coupon system, to give relief to patients suffering from the financial fallout. But for people with diabetes who have been using other brands, it will likely be medically and logistically challenging to switch to Eli Lilly’s formula, which works differently and has different dose durations than competing manufacturer’s formulas. It’s also sad that Eli Lilly waited this long to act on the problem — and that they seem to be doing so primarily to get a short-term public relations bump.
Hopefully, Americans will look back at this pandemic, and the response to it, as a turning point in our approach to regulating the pharmaceutical industry. But it shouldn’t take such a catastrophe for lawmakers to realize that the way this country develops and sells insulin is fundamentally broken.
The longer the border remains shut, the more likely I am to see my friends rationing insulin and the more likely I am to get emails asking if I have any to spare. If it remains shut for more than a few more weeks, as government leaders now indicate it will, I am likely to be sending those emails myself. I just hope the border reopens before my crisper drawer gets empty.
James Stout, Ph.D., lives and teaches in San Diego, helps run diabetes and exercise nonprofit programs in Indigenous communities, and volunteers with Universities Allied for Essential Medicines.











