‘Evidence-Based Medicine’ and the Expulsion of Peter Gøtzsche
For eight months in 1975, Peter Gøtzsche recalls driving around Denmark misleading doctors about a new, more expensive type of penicillin. He was 25 years old, with master’s degrees in biology and chemistry. As a pharmaceutical representative for the Sweden-based Astra Group, he was tasked with promoting Globacillin, which was said to be more effective than regular penicillin. At the time, Gøtzsche says he did not know that the claims he was making on behalf of his employer were not backed by high-quality evidence.
Gøtzsche stayed in the pharmaceutical industry for another eight years, writing brochures, strategizing ad campaigns, and, eventually, presiding over clinical trials. It was here that disillusionment set in. Gøtzsche — in his telling, still a principled naïf — would watch with dismay as his superiors twisted or suppressed any unflattering trial results. Increasingly distraught, Gøtzsche began pursuing a medical degree, leaving the industry for good in 1983.
His medical thesis, titled “Bias in Double-Blind Trials,” examined the claims of 244 reports of clinical trials for non-steroidal anti-inflammatory drugs, a group that includes ibuprofen and aspirin. Gøtzsche’s writing strongly critiqued the marketing practices of his former employer, Astra-Syntex, pointing out that no good evidence existed for their claim that the higher the dose, the better the effect.
That thesis was read by an Oxford researcher and physician named Iain Chalmers. It confirmed his impression, Chalmers wrote to Gøtzsche in 1990, that Gøtzsche was “doing extremely important research.” Chalmers, founding director of Oxford’s National Perinatal Epidemiology Unit, had spent much of the preceding decade hand-searching dozens of journals for studies relevant to care during pregnancy and childbirth. His idea was to collect these papers and compile them into reports so that doctors pressed for time would have authoritative, quickly-scannable syntheses of the best available data. In 1993, Chalmers sent an invitational letter to dozens of people, including Gøtzsche, to help found a not-for-profit organization dedicated to gathering and summarizing the strongest available evidence across virtually every field of medicine, with the aim of allowing clinicians to make informed choices about treatment.
They called it the Cochrane Collaboration, after Archie Cochrane, a Scottish epidemiologist and one of the earliest and most prominent advocates for randomized controlled trials, the gold standard of clinical research. Cochrane today has 11,000 members with supporters in 130 countries, and many of the group’s most high-profile findings — that the placebo effect might be a myth; that mammography likely doesn’t decrease breast cancer mortality, and turns healthy women into cancer patients via false or ambiguous findings — emerged from Gøtzsche’s research.
Gøtzsche became the closest thing the world of statistical analysis had to a full-fledged celebrity. His findings were trumpeted, repeatedly, in The New York Times, with his mammography findings even making the front page in 2001. He became the subject of a documentary and was featured in at least one other. “The Daily Show” once had him play a kind of Big Pharma Deep Throat in a segment on the opioid crisis. Viewed by many as a relentless fighter who has accused entire disciplines of nigh-irredeemable corruption, Gøtzsche’s crusades earned him the respect of powerful peers and a loyal following of layperson-skeptics around the world.
So it came as a surprise, at least to outsiders, when Gøtzsche was summarily expelled in fall of last year from the organization he helped found. He was voted off the board, then stripped of his position as director of the Nordic Cochrane Center, Cochrane’s Danish outpost. The stated reason for his termination was, according to a statement from Cochrane’s governing board, “an ongoing, consistent pattern of disruptive and inappropriate behaviors,” along with a breach of the organization’s spokesperson policy, which requires collaborators to clearly identify whether they’re speaking on behalf of themselves or of Cochrane.
The seeming suddenness of his expulsion, and what critics view as its misguided pretext, has exposed rifts that go back decades: debates about the pharmaceutical industry’s influence on medicine and about the research community’s tolerance of dissent. More fundamentally, Gøtzsche’s expulsion has crystalized a longstanding debate about the proper role of data in the practice of medicine.
Whatever their differences, Cochrane and Gøtzsche are both vocal supporters of evidence-based medicine, a movement that developed nearly 30 years ago to emphasize the use of well-designed research in medical decision-making. The problem is that neither side, nor really anyone, can agree on exactly what evidence-based medicine ought to mean. Some critics have characterized Gøtzsche as a rigid intellectual who views assessing scientific data as a purely technical task that does not require the input of experts in a given field. Gøtzsche calls such characterizations unfair, arguing that he simply advocates — as everyone at Cochrane should — for the use of rigorous methodology and the elimination of bias in assessing the efficacy of treatments. And while the organization has built its reputation on providing trusted evidence, Gøtzsche now criticizes its methods, accusing Cochrane of bending to industry influence and overlooking important documentation of harms.
“Cochrane’s reliance on published [randomized controlled trials],” Gøtzsche wrote in an email to Undark, “makes Cochrane a servant to industry, which passively promotes what industry wants Cochrane to promote: messages that are very often untrue.”
No one from Cochrane’s leadership agreed to speak with Undark about the Gøtzsche dust-up, or to respond to such charges, but in the organization’s statement accompanying his ouster, they made their position clear: “Cochrane is a collaboration,” the board declared, “an organization founded on shared values and an ability to work effectively, considerately, and collaboratively.”
Gøtzsche, they suggested, didn’t seem to understand that.
In 1992, the Journal of the American Medical Association published a paper titled “Evidence-Based Medicine: A New Approach to Teaching the Practice of Medicine.” With more than 30 co-authors, it advocated “a new paradigm for medical practice,” deemphasizing intuitional and clinical experience in favor of the latest research data. “We believed that the way we were practicing medicine was different from how it had been practiced before,” the paper’s lead author, Gordon Guyatt recalled, — “fundamentally different.”
The paper had its origins at McMaster University in Ontario, Canada, where David Sackett, an American-Canadian epidemiologist, had been arguing that doctors should be able to make sense of the literature and apply it to their practice. Among other things, this meant studying randomized controlled trials to determine whether an intervention really works.
In a randomized controlled trial, the participants are divided into two or more groups. One group gets the intervention — a drug, for example — and the others get a placebo, a varied dose of the drug, or some other form of treatment. By the 1970s, these trials were a standard component of drug approval. Still, even in the early 1990s, the results had a more modest influence on clinical practice than they do today. According to Guyatt, doctors did not typically keep up with the literature, and drugs were dispensed according to the guidance of local opinion leaders or influence from pharmaceutical representatives. The idea behind evidence-based medicine, then, was for clinicians to consult the literature before making a decision.
Chalmers had been a visiting professor at McMaster in the late 1980s. As the McMaster crew refined and exported their theories, Chalmers began building his own movement, distinct from but parallel to evidence-based medicine, and with significant overlap in ideology and personnel. Its roots lay in the Gaza Strip, where Chalmers had worked as a United Nations doctor in 1969 and 1970. “I believe I would have done a better job, and that fewer of my patients would have suffered, if I’d had access to a good source of reliable evidence for research,” Chalmers said.
The Cochrane Collaboration was meant to rectify this problem by way of something called a systematic review: all the best randomized controlled trial data on a given treatment, sifted and synthesized into one readable report. “Basically, it was a bunch of troublemaking anarchists who wanted to do something which the establishment was not doing,” Chalmers said. A skilled evangelizer (“In those days, to meet Iain Chalmers was to get hooked to his cause,” said Jos Kleijnen, founding director of the Dutch Cochrane Center), Chalmers had no trouble assembling a global network of like-minded colleagues for his first symposium — Gøtzsche among them.
“The Cochrane Collaboration was an extraordinarily powerful threat against authority,” Sackett told the researcher and author Alan Cassels in his 2015 book on Cochrane. “Individuals who had reputations based upon ‘this is the way this disorder must be treated’ obviously were terribly threatened by what was going to happen with these young upstarts, and kids, and punks, and even laypeople challenging them about what they said must occur in terms of health care.”
In an interview, Peter Gøtzsche expresses his views on the “criminality” of pharmaceutical companies.
The backlash, then, was not surprising. And yet, by the end of the 1990s, the Cochrane Collaboration had attained more or less its present-day esteem, and evidence-based medicine was installed as the dominant paradigm of Western medical practice, a position from which it is has not budged in 20 years. The Collaboration’s efforts were embraced by nurses and younger doctors, who for the first time had a means of challenging the decisions of their elders — what proponents sneeringly called “eminence-based medicine.”
Cochrane, which began as an almost whimsical experiment among a group of like-minded colleagues — an effort, according to Hilda Bastian, one of its founding members, to work out something like the total sum of human knowledge — has morphed, in the course of a quarter-century, into one of the world’s most prestigious medical research bodies, with outposts in dozens of countries and yearly outlays exceeding $1 million apiece from the U.S., U.K., and Australian governments, plus large donations from groups like the Bill and Melinda Gates Foundation, which gave Cochrane $1.15 million in 2016.
Cochrane’s total income last year was roughly $13 million, most of it from royalties on its enormous library of systematic reviews, generated by Cochrane’s global network of research centers and licensed to universities and hospitals around the world. Historically, these research centers have been more or less autonomous, free to pursue their own projects under the Cochrane banner while Cochrane’s main office in London lobbied for and distributed funding.
In recent years, though, Cochrane’s leadership has adopted a more hands-on approach, attempting to centralize the efforts of its far-flung franchises. In November of 2018, 16 disillusioned Cochranites formed Cochrane Members for Change, to protest what one member, Robert Wolff, described in a blog post as a mismatch between these two approaches, “a grassroots science-focused collaboration” on the one hand, and a “top-down more business-oriented” organization on the other. Among this group, Gøtzsche’s termination was interpreted as a troubling symbol of the new business-oriented direction.
Gøtzsche said that Cochrane was “founded on the best of human motives — honesty, generosity, fairness, transparency, openness.” He believes his expulsion will dog the organization for years to come. “It was a fundamental error they made,” he said.
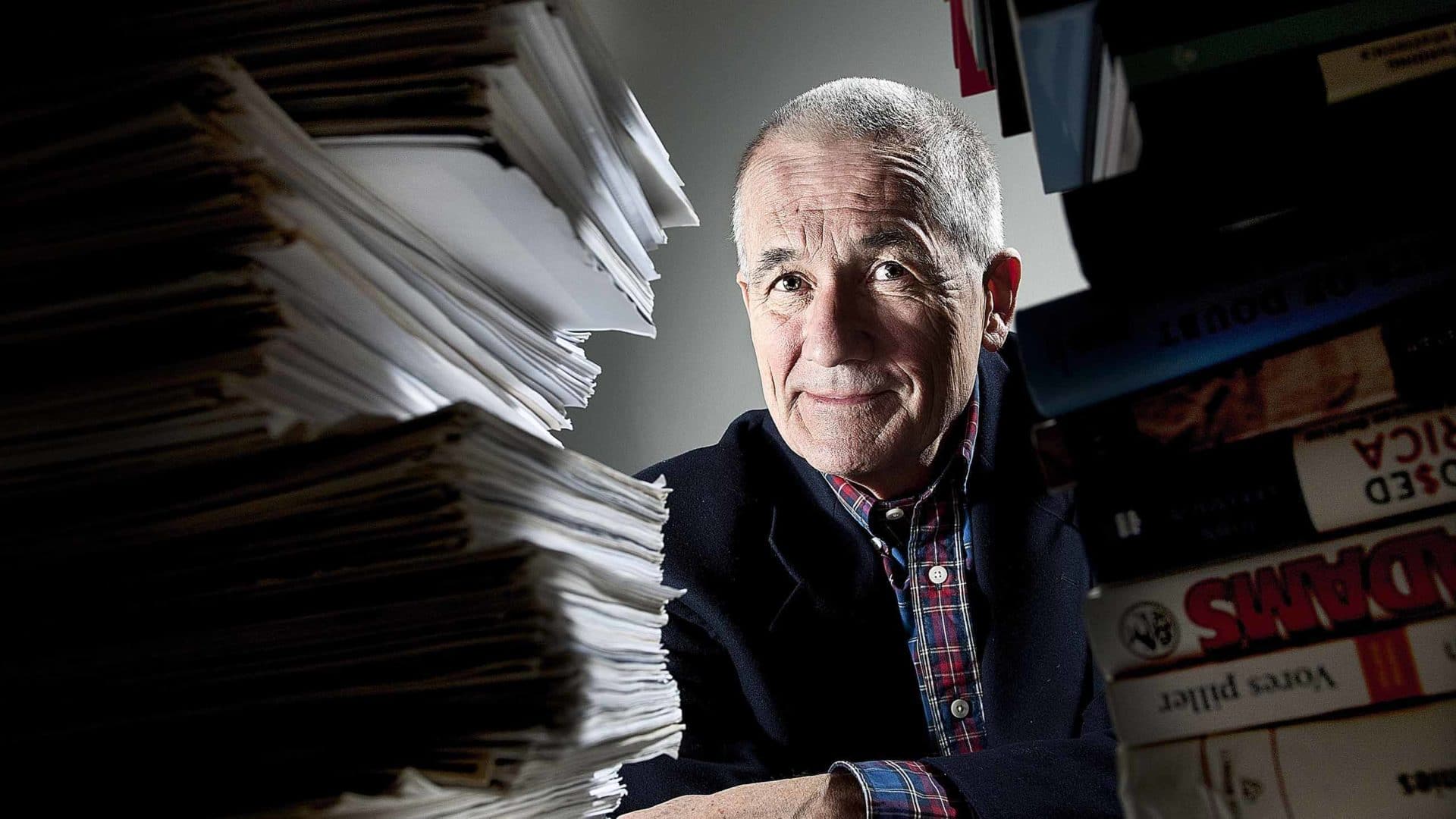
In person, Gøtzsche can be a warm, appealing, gently ironic presence. At 70, he is tall and thin, with a faint dusting of gray hair. Both his eyebrows arch skeptically in the same direction. He delights in bad jokes — “irretrievably bad jokes,” Chalmers said. “Not rude or anything like that; they’re just not funny.” He can be famously good company, and it is not hard to see why so many of the people he has mentored and worked with remain loyal to him. “I just remember [Peter] as one of the most sincere scientists that I have ever met,” said Kleijnen, the Dutch Cochrane Center founding director.
But when it comes to his books and public persona, he also has a famously take-no-prisoners approach. “I dig so deeply in my research,” Gøtzsche said, “that I find the skeletons people have buried down there. And when I put them up on the ground people yell and scream, and call me all sorts of names, because they didn’t think anybody would ever find the skeletons.”
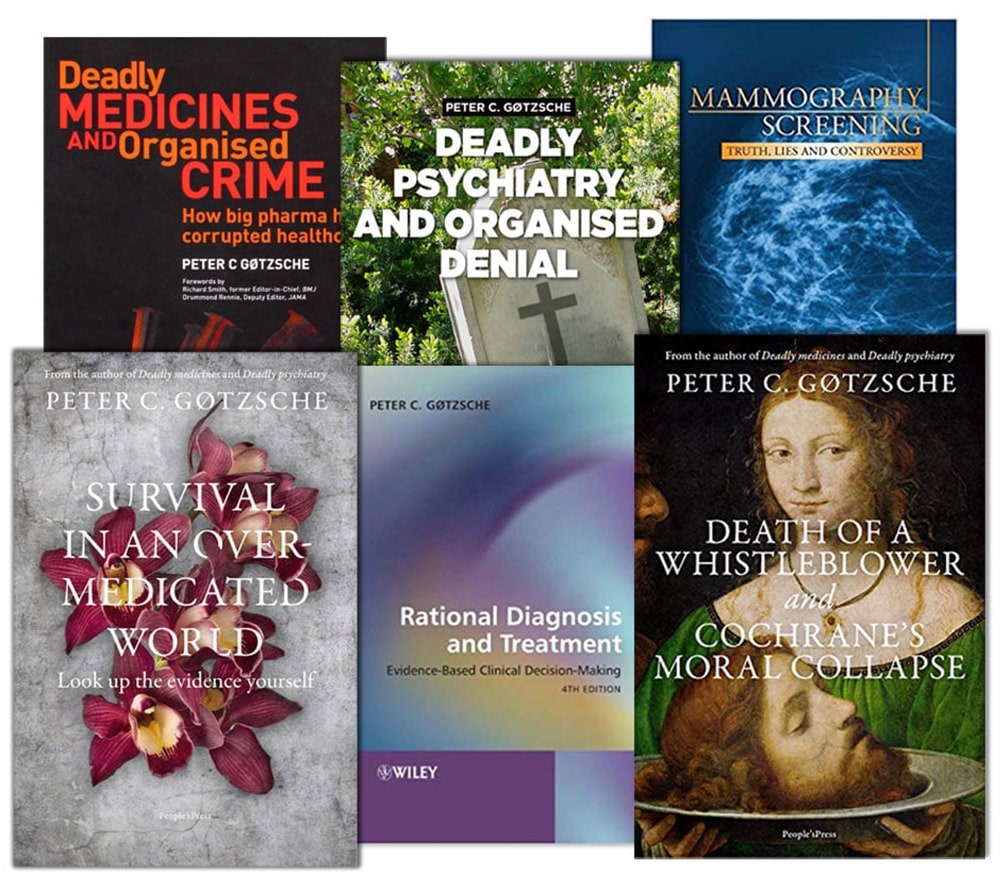
It started with Gøtzsche’s 2012 book on mammography, a recap of the research and controversies attendant to his decade-plus campaign against breast cancer screening. Gøtzsche’s view was, and still is, controversial. His public profile rose a year later with his next book, “Deadly Medicines and Organized Crime.” It excoriated the pharmaceutical industry, likening its tactics (bribes, kickbacks, serial fraud) to those of the mob.
Gøtzsche’s next crusade had markedly less currency, and planted him, in the eyes of some, on the outer edges of the fringe. Released in 2015, the book was called “Deadly Psychiatry and Organized Denial.” Its argument, more or less, is that much about the way psychiatry is practiced is wrong; that the specialty is built on “myths, lies and highly flawed research”; that the majority of practicing psychiatrists are, actively or through ignorance, deceiving and harming their patients, given Gøtzsche’s finding that prescription pills are the third leading cause of death in the U.S. and Europe; and that these same psychiatrists might have noticed some of this were they not helplessly compromised by industry money.
The main reason for the “drug disaster” he writes, is that “leading psychiatrists have allowed the drug industry to corrupt their academic discipline and themselves.” Gøtzsche then goes on to compare the leaders in the field to “primate silverbacks in the jungle” and claims that “psychiatric research is predominantly pseudoscience.”
The psychiatric community had some quibbles with this. Cochrane did, too. When Gøtzsche published a summary of his findings in the Daily Mail, Cochrane’s leadership took the unusual step of publicly distancing themselves through a statement on Cochrane’s website. In addition to stating “unequivocally” that the organization did not share Gøtzsche’s views, it publicly chastised the Danish professor: “He has an obligation . . . to distinguish sufficiently in public between his own research and that of Cochrane — the organization to which he belongs.”
This infuriated Gøtzsche, and the encounter seems to mark the point of no return in his relations with Cochrane management. In the years since, Gøtzsche, who has no special training in psychiatry, has become a fixture on the antipsychiatry circuit, criticizing the discipline in editorials, in presentations, and at various symposia about withdrawing from psychiatric medications. (He has since claimed that almost all Cochrane reviews on psychiatric drugs should not be trusted.) Up until his expulsion, Gøtzsche listed his title in these outreach activities as director of the Nordic Cochrane Center, leading multiple parties to complain to Cochrane itself.
One of these complainants, Fuller Torrey, a researcher at the Stanley Medical Research Institute, a nonprofit that funds work on schizophrenia and bipolar disorder, shared his correspondence with Cochrane’s chief executive. Torrey wrote to call attention to Gøtzsche’s association with an organization called the Hearing Voices Network, which, Torrey claims, “promotes the belief that … auditory hallucinations are merely on end of a normal behavior spectrum.” Echoing other complaints, he added in a follow-up letter: “It is very difficult to imagine how anyone with these views could possibly be objective regarding a Cochrane study of antipsychotics, thus impugning your credibility which is your most important asset.”
In other words, Torrey seemed to be asking: Is this what Cochrane represents?
Gøtzsche and his defenders argue that Cochrane is not meant to “represent” anything — that Cochrane, as initially conceived, is simply a loose network of independent researchers, who will inevitably hold a range of opinions. But the organization Gøtzsche was forced out of in September of last year was different in crucial respects from the one he’d joined a quarter-century earlier. For one thing, it was no longer called the Cochrane Collaboration. It dropped the latter word in 2015, as part of a broader rebranding effort, and is now known simply as Cochrane.
In 2012, the organization hired Mark Wilson to serve as its CEO. Wilson, who does not have a science background, had spent more than a decade working in operations and development for the International Federation of Red Cross and Red Crescent Societies. In the view of Cochrane’s latter-day detractors, Wilson is the driving force behind the organization’s abandonment of its early, idealistic principles. According to them, he has corrupted the legitimacy of Cochrane’s systematic reviews by kowtowing to pharmaceutical companies and taking a relaxed stance towards conflict-of-interest issues. Former colleagues also describe Wilson as someone who uses business-speak as a weapon, rapidly jargon-ing subordinates into submission. “You can’t get a word in edge-wise,” said Kay Dickersin, another founding Cochrane member and, until it closed last year, the director of the U.S. Cochrane Center.
For his part, Wilson did not respond to multiple interview requests sent by email. Similarly, other members of Cochrane declined to be interviewed. “Having spoken with my colleagues,” Cochrane spokeswoman Jo Anthony wrote in an email, “I understand, at this time, none of them wish to follow up on your polite request and are happy for me to send you this note on their behalf.”
Wilson has been praised for plotting a stable financial future for Cochrane, and for effectively consolidating an unruly, globe-spanning collective of scientists. Even Hilda Bastian — one of Cochrane’s founding members, who parted ways with the organization over the board’s refusal to remove the paywall from the Cochrane Library — noted that Wilson is politically astute. Cochrane “is lucky Mark Wilson hasn’t abandoned them, turned on them,” she added.
“Cochrane started out as a movement,” said Nick Royle, Wilson’s predecessor as CEO. “Over time, it became more business-like, and some of those early adopters perhaps didn’t fit so well into the later framework. That’s just the normal evolution of an organization. That’s just how these things are.”
Gøtzsche has little patience for the new status quo. During a visit this past March, he was highly energized, particularly when discussing what he sees as Wilson’s venality, power-lust, and imaginative bankruptcy. When he isn’t denigrating Wilson, Gøtzsche seems to impute to him an omnipotence somewhat disproportionate to his role as chief executive. In “Death of a Whistleblower and Cochrane’s Moral Collapse,” Gøtzsche’s book-length account of his Cochrane ordeal, Wilson’s regime is compared to those of Voldemort, Big Brother, and Stalin. “He is so powerful that he controls the whole governing board,” Gøtzsche told me. “He controls everything.”
Disagreements over the direction of the organization came to a head last September. Ahead of its 25th annual colloquium, held at Edinburgh’s International Conference Center, governing board members voted to expel Gøtzsche from the organization he had helped turn into a global force. The reason for the expulsion, as related later that month to STAT and Retraction Watch: Gøtzsche had, among other things, used Cochrane letterhead on non-Cochrane-related business, in such a way as to potentially violate the organization’s spokesperson policy.
(An independent legal team hired to review the dispute had not concluded prior to the expulsion that Cochrane’s policy warranted sanction.)
On September 16, the BMJ published a blog post by a researcher who worked with Gøtzsche titled “Cochrane — a sinking ship?” That evening, in Science: “Evidence-based Medicine Group in Turmoil After Expulsion of Co-founder.” And a news article in Nature the next day: “Mass Resignation Guts Board of Prestigious Cochrane Collaboration.” Similar articles were popping up in Italy, Colombia, and Sweden.
Near the end of the conference’s second day, attendees took their seats for the Annual General Meeting in the conference hall’s 1,200-capacity Pentland Suite. About 30 minutes in, the governing board’s co-chair, Martin Burton, took the stage. (The meeting was recorded and posted on YouTube.) Gøtzsche recounts in “Death of a Whistleblower” that before the meeting, he and David Hammerstein — a fellow board member who’d resigned upon Gøtzsche’s expulsion — had gathered signatures for a vote of no confidence in the present board, and the establishment of a new one right there in the conference hall. At Gøtzsche’s signal, two of his colleagues were to stand and set the process in motion.
Gøtzsche lifted himself from his seat and signaled to his colleagues across the room. But the colleagues stayed seated. (Neither would comment for this article, but in his book on the expulsion, Gøtzsche suggests that at least one, Karsten Juhl Jørgensen, was worried about Wilson taking retributive action.)
No coup materialized. About a week later, Gøtzsche was formally booted from the board. About a month after that, he was summarily fired from his job as the director of the Nordic Cochrane Center.
The Cochrane/Gøtzsche split has by now been made to bear the weight of a number of disparate narratives by the journals and the medical press. One popular narrative posits Gøtzsche as a truth-seeking maverick — the spirit of evidence-based medicine incarnate — going up against the creeping commercialism and bias-tolerance of mainstream science. Peter “is willing to take positions that are sometimes very unpopular and probably create a lot of anxiety and even enmity in some circles,” said John Ioannidis, a Stanford professor and prominent supporter of evidence-based medicine. “We need people who are willing to take unpopular positions and provide the data.”
Another narrative describes Gøtzsche as a practitioner of an older, perhaps outmoded model of evidence-based medicine in which reviewing study data is viewed as a narrow task — as, essentially, math — which has since been superseded by the more open, pluralistic version supposedly taken up by Cochrane since Wilson’s hiring.
Both views were recently unpacked in a 2019 paper published in the Journal of Evaluation in Clinical Practice. The paper’s corresponding author, University of Oxford professor Trish Greenhalgh, has in recent years emerged as one of the most prominent internal critics of the direction the evidence-based medicine movement has taken since its inception. In the 2019 paper, she takes particular issue with how the movement prioritizes clinical trial data over and above a physician’s intuition or knowledge.

(Greenhalgh said she could not comment for this article, citing the possibility of a legal challenge to her piece from Gøtzsche. Gøtzsche, in a private, 11-page rebuttal he sent to Greenhalgh, which he shared with Undark, claims that the article is “libelous” and “riddled with biases, errors and inexcusable oversights.”)
Evidence-based medicine’s detractors further point out that its very name makes it difficult to criticize. “How do you argue against evidence-based medicine?” asked Mark Tonelli, a professor of medicine at the University of Washington. One way would be to destabilize the very concept of “evidence.”
Randomized controlled trials, which are typically conducted by scientists who don’t practice medicine, and often funded by people who want to sell drugs, are not designed with the patient in mind. For one thing, as Tonelli pointed out, these trials tend to weed out patients with more than one illness, meaning these drugs are being tested on people who bear little resemblance to huge swaths of the patient population. (“What elderly diabetic patient doesn’t have comorbidities?” asked Tonelli.) And as Greenhalgh pointed out in a 2014 paper titled “Evidence-Based Medicine: A Movement in Crisis?” — which set off a fervent round of soul searching in the evidence-based medicine community — the results of randomized controlled trials may be “statistically but not clinically significant.”
More importantly, according to these same critics, in elevating randomized controlled trials, the evidence-based medicine movement has consciously demoted all other forms of knowledge: observational studies, clinical experience, and the unique, un-averageable needs of the patient on the other side of the doctor’s desk. Greenhalgh suggests, in her Journal of Evaluation in Clinical Practice paper, that this has lately begun to change, citing an “epistemic crisis” in the movement. Gøtzsche, she argues, is trying to resist the “epistemic forces” that are redefining his world.
The implication is that in sacrificing Gøtzsche, Cochrane is taking a step towards a reformed, less aggressively doctrinal evidence-based medicine. The problem, from what Gøtzsche has argued, is that he agrees with much of what Tonelli and Greenhalgh have to say. Rather than relying solely on randomized controlled trials, he says, “observational studies and case reports can be very important for finding harms.”
In any case, exactly how dismissing Gøtzsche would lead to any real change in Cochrane is unclear, as is any specific way in which this “epistemic crisis” has led to tangible changes for the better. According to Tonelli, these concerns have not trickled down to clinical practice. For people like Greenhalgh in particular, there’s a feeling that this “can be solved,” he said. “For me, it’s more of a true epistemic limitation and the only way to get past it is to acknowledge the severe limitations of clinical research for practice and then re-broaden our approach to how we view medical knowledge.” Despite being primarily targeted at patients, the conclusions of “Deadly Psychiatry” might provide one example of an evidence-based medicine troublingly abstracted from real people’s needs.
David Healy, a psychiatrist, prominent psychiatry critic, and sympathetic ally of Gøtzsche’s, pointed out that “if you’re not constrained by the need to actually treat people” and don’t see that medications can be helpful, “then it’s easy to drift into thinking it would be best if we didn’t have them. And I think Peter has toppled a little bit too much over that way.”
This past March, Gøtzsche launched an organization called the Institute for Scientific Freedom, which aims to “preserve honesty and integrity in science.” It was part of Gøtzsche’s campaign to avenge himself for the perceived wrongs visited upon him by Cochrane, and to further the work he once did at the Nordic Cochrane Center. (The article he wrote to announce the institute, published on the psychiatry-skeptic website Mad in America, contained 12 paragraphs on his expulsion from Cochrane and on Cochrane’s perceived moral rot, and roughly one sentence on what the institute would actually consist of.)
Gøtzsche’s home, 20 to 30 minutes by car from the center of Copenhagen, hummed with activity on the afternoon before the institute’s opening symposium, which was to be held the following day. Among those milling about the kitchen were Peter Wilmshurst, the British cardiologist who in 1986 had blown the whistle on Sterling-Winthrop, a drug company which had tried to suppress his negative findings about the cardiac drug amrinone. (He was able to blow the whistle a second time, two decades later, when a medical device company that had recruited him for help tried passing off misleading data.)
Also in attendance was the U.S. psychiatrist Peter Breggin, who at 83 years old, is still capable of generating controversy — as when, last year, he served as an expert witness for Michelle Carter, the woman who, as a teenager, pressured her boyfriend into killing himself. (Breggin has made his name in part as an expert witness for people who commit crimes while on prescription drugs, which Carter was at the time.)
Pamela Popper, another of the next day’s lecturers and a prominent advocate for healthy eating as a substitute for medication — and a business partner of Breggin’s — was also visiting. A naturopath, Popper runs a popular YouTube channel, and it had driven some of sign-ups for the next day’s conference. She wasn’t surprised, she said, by what happened to Gøtzsche. “We’ve all been come after,” she said. “It’s a badge of honor really, to be pursued by them. It must mean you’re doing something right.”
With Gøtzsche, of course, the pursuit is reciprocal. He is infamous for coming after people, even his own colleagues. Two months before Edinburgh, Gøtzsche co-authored a critique of Cochrane’s recent HPV vaccine review, which had concluded that “there is high-certainty evidence that HPV vaccines protect against cervical precancer in adolescent girls and women.” Gøtzsche’s paper accused Cochrane’s researchers of excluding nearly half the relevant trials and incompletely assessing certain adverse events and safety signals.
From all the available evidence, this paper was not the cause of Gøtzsche’s expulsion. His two co-authors, also members of Cochrane, were not removed from the organization. The news coverage, though, tended to link the two events, and Gøtzsche was subsequently taken up as a hero by anti-vaccination groups, who assumed he shared their worldview. The Danish researcher appeared to outside observers not to be at pains to disabuse his new followers of this notion. If anything, he appeared to be courting it.
A few weeks before the symposium, Gøtzsche’s face had cropped up in the promotional materials for a workshop run by Physicians for Informed Consent, a prominent anti-vaccination group, to be held just a few days after the opening of his institute. Gøtzsche was to deliver its keynote, alongside such anti-vaccine luminaries as Toni Bark and Robert F. Kennedy Jr. When the news was picked up on Twitter, Gøtzsche quickly pulled out. When asked about it, he claimed he hadn’t realized who the other speakers would be.
The Institute for Scientific Freedom’s symposium was held at Bethesda, a historic church in central Copenhagen. The one-day event was to be made up mostly of short talks (sample titles: “Medical journals are an extension of the marketing arm of pharmaceutical companies”; “The many forms of scientific censorship in psychiatry”) with two audience Q&As, one before the lunch break and one at the end. There were about 80 or 90 people in attendance, some who appeared to be in their 20s, but most who looked to be at or beyond middle-age. Gøtzsche, appropriately, looked nearly priestlike, standing on the stage in all-black.
The fact that Gøtzsche had inadvertently organized a kind of impromptu anti-vaccination convention became clear during the first Q&A, after the fourth or fifth successive question about vaccines. One questioner asked Peter Aaby — who conducts vaccine research in Africa — why, given the apparent abundance of studies showing that measles is actually good for you, we don’t try and study what happens when you give certain African children large doses of Vitamin C instead of “injecting them full of toxins” (i.e., giving them the measles vaccine).
“Could I perhaps ask also for questions about … not vaccines?” Gøtzsche asked eventually.
The next questioner promptly took the mic and said they had a question about vaccines.
“Please, please, please talk about something else now!” said Gøtzsche.
“I just want to say that the BCG part of tuberculosis, which is in the BCG vaccine, was never on the schedule in the U.S., and tuberculosis was the number two killer in — ”
“But please, excuse me, this is still — ”
The woman talked over him, so Gøtzsche raised his voice to match: “I ask you very kindly to not ask a question about vaccines at this point in time.”

Iain Chalmers had flown in from London to attend the event. He’d had to duck out early, but said later by phone that he had been troubled by much of what he’d managed to see.
The older psychiatrist, he said, referencing Peter Breggin, “basically, he seemed to feel that undying love was a good treatment for psychosis.” And referencing Pam Popper’s talk: She seemed to think “you could stay healthy all your life if you eat the right foods.” Not to mention the audience, and their worryingly sustained applause at certain lines from the stage, notably those seeming to be against vaccination.
It had become clear to Chalmers, at least, that in taking on the establishment, Gøtzsche had attracted the wrong crowd. He didn’t mention any of this at the conference. But before leaving for the airport, Chalmers relayed one bit of tough-love advice: namely, that Gøtzsche should reconsider making himself the public face of his new organization. Nothing against him — it’s just, he isn’t much of a showman. Sort of an anti-showman, really.
There had been plans to publish a transcript of the Q&A, but these were quickly scuttled — “too embarrassing,” Gøtzsche admitted later. The whole thing seemed to alarm him. “We were quite disturbed by these people,” he said.
Gøtzsche had some trouble getting his recent book, “Survival in an Overmedicated World,” published in English. He said he never needed an agent before, but had to hire one this time. After a round of rejections, Gøtzsche says, the agent informed him that American publishers thought it somewhat irresponsible to publish a manual about how to bypass doctors and seek out the best medical information via the internet. “You should not trust your doctor. You should look up the evidence yourself,” he told me, explaining the book’s thesis.
This project might represent, depending on your perspective, either the vilest perversion or the perfect apotheosis of the evidence-based medicine ethos. If we reduce the practicing doctor to an algorithm, mechanically relaying the relevant treatment as prescribed by the latest data, then dispensing with that doctor — with her biases, her blind spots, her susceptibility to the latest marketing or lobbying efforts — seems a sensible next step.
The book has appeared in several languages, with the English version published at the end of April. Its opening paragraph is instructive:
“‘You do not ask a barber if you need a haircut.’ Most people have heard this expression or something similar. Yet we willingly allow our doctors to subject us to various diagnostic investigations and treatments which may be financially beneficial for themselves. Health care is riddled with financial conflicts of interest, and even when your doctor does not directly benefit, there are many other reasons you should be on the alert.”
Having started his career critiquing the drug companies, Gøtzsche’s circle of scorn has since widened to take in mammographers, psychiatrists, scores of his own colleagues, and, now, seemingly every single doctor in the world. According to him, he has another book — “Vaccines: Truth, Lies, and Controversy,” coming out in February.
As for whether he’s through with Cochrane, Gøtzsche said: “It’s not over yet.”
Daniel Kolitz is a writer living in Brooklyn.
UPDATE: A previous version of this piece incorrectly stated the number of Cochrane members who formed Cochrane Members for Change as 620. There were 16 founding members. The group subsequently collected 620 signatures of support.










Comments are automatically closed one year after article publication. Archived comments are below.
The bigger picture Gotzsche’s versatile work points to is that the mainstream medical establishment is run by a bunch of psychopaths:
https://www.rolf-hefti.com/covid-19-coronavirus.html
That is the ultimate “forbidden” insight.
Gotzsche’s next crusade had markedly less currency, and planted him, in the eyes of some, on the outer edges of the fringe. Released in 2015, the book was called “Deadly Psychiatry and Organized Denial.” Its argument, more or less, is that much about the way psychiatry is practiced is wrong; that the specialty is built on “myths, lies and highly flawed research”; that the majority of practicing psychiatrists are, actively or through ignorance, deceiving and harming their patients, given Gotzsche’s finding that prescription pills are the third leading cause of death in the U.S. and Europe; and that these same psychiatrists might have noticed some of this were they not helplessly compromised by industry money.
Great article! I’d argue with a couple of points: firstly Gøtzsche didn’t “quickly” pull out of the PIC event:
https://twitter.com/Rosewind2007/status/1230417119260676096?s=20
Secondly “The fact that Gøtzsche had inadvertently organized a kind of impromptu anti-vaccination convention became clear during the first Q&A…”
Nope, it was clear from much much earlier.
I tweeted about this.
But great article and superb photos.
Cheers,
Rosewind
I’ve asked the author of this article if he ever spoke with Lars Jorgensen, the corresponding author of Gotzsche’s HPV vaccine critique and his last PhD student. I haven’t gotten an answer, but Gotzsche was conveniently removed from Nordic Cochrane the week before Jorgensen submitted his dissertation on HPV vaccines naming Gotzsche as his “Principal Supervisor.” The reason Jorgensen wasn’t “removed” was because he graduated when Gotzsche was removed.
https://drive.google.com/file/d/1B823OIQ3-5pBlEqRvTpD5HAcu80o9vVP/view
Not interviewing a key person for a vaccine story and leaving readers in the dark is par for the course at “Undark.”
https://www.autisminvestigated.com/author-ethan-lindenberger-hoax/
And how strange that after 25 years of presumably using letterheads the same way and being the same person, Cochrane suddenly decides it can’t stand Peter Gotzsche after he criticizes its view on vaccines. Of course, it really isn’t strange because it should be obvious to anyone familiar with this issue: Cochrane can no longer stand Peter Gotzsche because it can’t stand his view on vaccines.
Good piece of journalism that I think Cochrane’s leadership ought to respond to. My own two cents, speaking as a journalist, is that dropping “Collaboration” was as crazy as an aborted UK idea, years back, to rename “Royal Mail” as “Consignia”. But then I think it was crazy to rename the British Medical Journal, The BMJ. So what would I know?
Sackett’s concept of Evidence-Based Medicine (EBM), in the British Medical Journal in 1996, is that EBM relies on the combination of relevant research (which means going beyond randomized controlled trials), clinician judgment and experience, and family culture and values, to offer families a range of options for truly informed consent. relying on research alone may lead to recommending options that have no hope of acceptance to families, and relying on clinical judgment alone leads to the use of ineffective treatments by believers with no good research to back up the approach. The balance between these things is crucial. My understanding is that the US National Academies of Science Institutes of Medicine (now called the National Academies of Medicine) adopted this version of EBM in 2001. Still, we see people continue to use a definition of EBM that is restricted to RCTs and, in a way, can just as easily create misrepresentations in the field if negative studies aren’t published.. The advent of ALl Trials helps, requiring reporting on all clinical trials, but the fines are small and the process is still new. So far I have seen two studies reporting no effect of desvenlafaxine in children with depression, which in my view is rare, courageous and clinically helpful. But I’d like to see this discussion fleshed out to cover the range of definitions of EBM and the intent of Sackett and others in ‘allowing’ additional considerations beyond RCTs.
While the tone of the article is that Gotzchke is now questionable because his questions have extended toward the field of medicine in general, one would ask why should this be surprising or indeed, unethical? He has spent his time trawling through the negative depths of the medical industry and perhaps has uncovered even more than he expected.
The man should be judged on the data he produces and not through any bias toward those who question vaccines or medications. Indeed, everyone should question everything which is done to their body. That is common sense.
Doctors are not gods and they often make mistakes as we see from the death rate, in third place, from conventional medicine, most of it from prescribed drugs. More so because the chemists control the medical industry and influence research outcomes as has become increasingly clear.
It is not just Gotzche who has raised questions about the reliability of research. Editors of both The Lancet and The New England Journal of Medicine have done so and the work of Dr John Ioannadis concluded, most published research is false.
Methinks the writer of this article betrays his own prejudices rather than revealing Peter Gotzche’s.
Peter Gøtzsche – a true modern hero.