Tuberculosis is making a comeback. This month, the World Health Organization released its annual TB report, showing that the global incidence rate for the disease climbed almost 4 percent between 2020 and 2022 — from 128 to 133 cases per 100,000 people — reversing a decades-long gradual decline.
This surge wasn’t inevitable. In 2018, leaders from virtually every United Nations member country committed to essentially double funding for TB to $13 billion a year, with new resources going to expand diagnosis, treatment, and prevention. Instead, funding declined. The new WHO data show that governments only made $5.8 billion of the promised $13 billion available in 2022.
The impacts are not contained to low-income countries, making it harder for wealthier ones to ignore. New York City is grappling with a dramatic 20 percent increase in tuberculosis cases compared to this time last year, according to preliminary data reported by Politico. Meanwhile, the city’s health department describes the disease as a “life-threatening problem.” In Nebraska, health officials investigating an active tuberculosis case had to test more than 500 young children who had been exposed. In fact, preliminary data from the U.S. Centers for Disease Control and Prevention show that 23 states are seeing more people diagnosed with TB so far this year than in all of 2022.
Other countries with historically low TB rates are facing similar challenges. The United Kingdom recently announced a 7 percent increase in people contracting the disease. South Korea just reported its first rise in TB in 12 years. And Australian health authorities are on alert after the country has experienced multiple TB outbreaks in the last year and a half. All are snapshots of a global trend.
When government leaders shirk their responsibility to safeguard communities from this terrible disease, everyday people bear the cost. How else to explain that TB, though preventable and curable, kills more people worldwide than any other infectious illness?
This issue is personal to me. As a nurse serving at a clinic in Kenya in 2010, I developed unexplainable back pain. After a few months I could barely walk, and doctors finally diagnosed me with tuberculosis.
When government leaders shirk their responsibility to safeguard communities from this terrible disease, everyday people bear the cost.
TB is an airborne disease that usually affects the lungs, but the bacteria that infected me worked their way into my spine. Later tests confirmed my case was resistant to multiple drugs, which explained why I had been left bedridden for a year, despite receiving treatment.
The pain was horrific. A living nightmare. I’ve experienced nothing like it, before or since. And yet the worst part was the stigma that came with having TB. No one wanted to come near me. While sick, I had to inject myself 60 times over the course of two months. The isolation, loneliness, and despair cut me deeply.
But I was fortunate. I survived.
Many will not. In September, a report by The Lancet Commission on tuberculosis projected that TB is on track to kill 27 million people and cost the global economy more than $13 trillion by 2050.
This should not be happening. Some life-saving TB interventions such as nutritional support, which was recently shown to reduce TB mortality by up to 60 percent, cost pennies per day. With new diagnostics, simpler treatments, and the first TB vaccines in a century now going into the final stages of testing, statistical modeling conducted by the Stop TB Partnership projects that it’s possible to reduce TB deaths by 90 percent by 2030.
In fact, efforts to that end just got a boost. Recently, manufacturers have reduced prices for key TB diagnostic tests, antibiotic treatments, and preventive therapies — administered after exposure but before symptoms set in. Also welcome is Johnson & Johnson’s decision to not enforce patents on its TB medicine in 134 low- and middle-income countries, enabling cheaper, generic versions of the drug to be produced.
But governments must step up. Most urgently, they should mobilize the resources they have already committed for the TB response. Although it received little media attention, in September the U.N. General Assembly adopted a historic commitment to ratchet up annual funding for TB prevention, diagnosis, and treatment from $5.4 billion to $22 billion by 2027. Member countries also committed to a five-fold increase — to $5 billion annually — for research to develop better diagnostics, treatments, and at least one new vaccine.
The pain was horrific. A living nightmare. I’ve experienced nothing like it, before or since. And yet the worst part was the stigma that came with having TB.
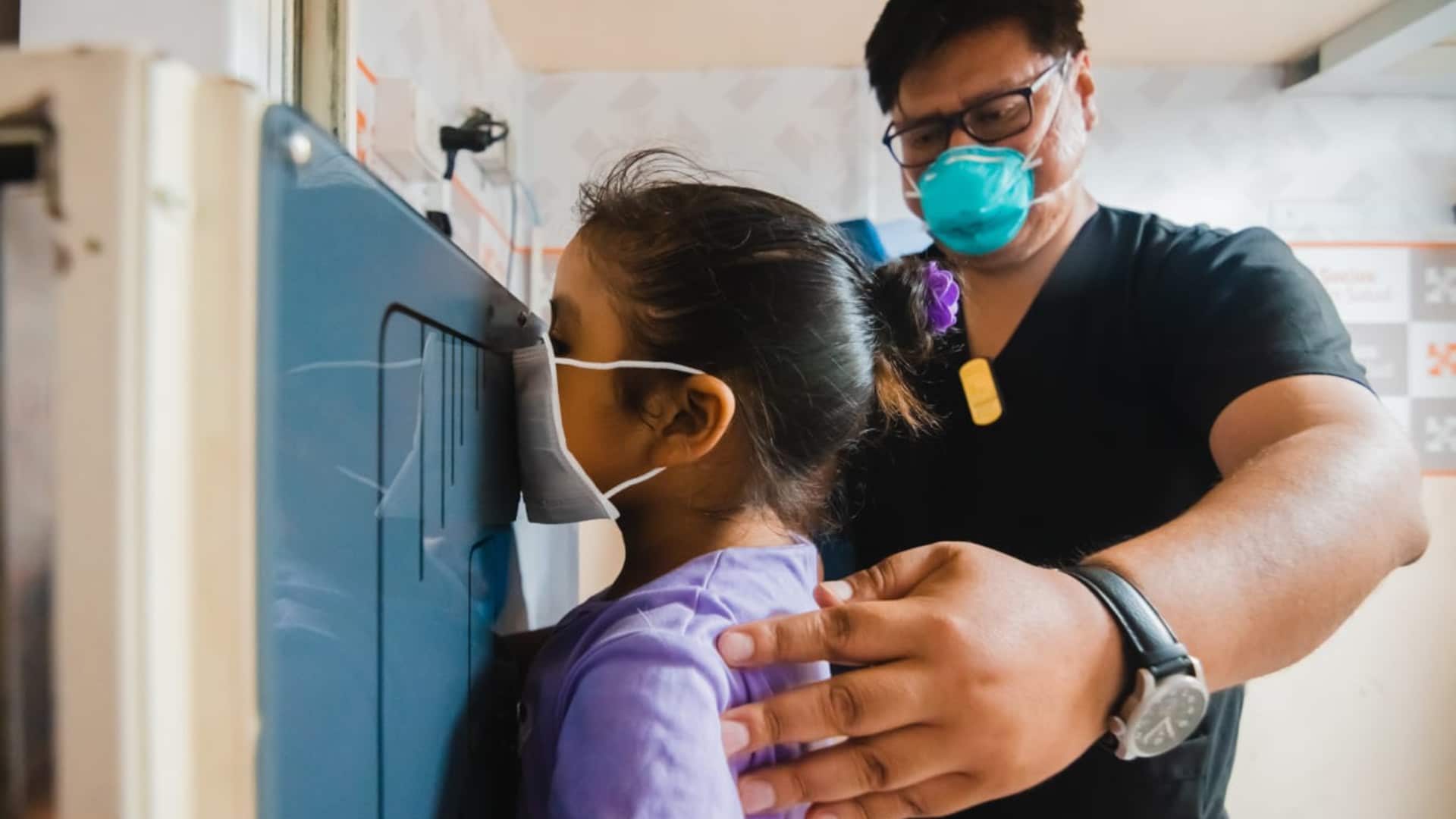
It’s critical that governments meet these commitments, because health workers today cannot possibly deliver TB care at the scale that’s required. Worldwide, roughly one in three people with TB — more than 3 million — go undiagnosed each year, which means they remain contagious. Clinics like mine need these additional resources to help us shift from passively receiving people with TB once they’re very sick, to actively finding and delivering care to people with TB in our communities. Experts agree that this proactive approach is key to halting TB’s spread.
That said, funding isn’t everything. People with TB need their political officials to be champions for them. TB stigma may keep people from seeking diagnosis and treatment. Leaders can use their platforms to raise constructive awareness and encourage people to seek the care they need. Otherwise, communities will continue living in fear of this preventable, curable illness.
When I was sick, I fought for my life. Surviving TB has allowed me to fight for the lives of my patients. Those who hold the power to end this disease must fight for us, too.
Naomi Muthua Wanjiru is a TB nurse, health advocate, and survivor of multidrug-resistant tuberculosis who lives in Nyandarua County, Kenya. She has worked with Stop TB Partnership, Global Fund Advocates Network, and other TB initiatives.
Paul Jensen, science communications consultant and TB advocate, assisted Wanjiru with editing and sourcing for this piece.