Worse Than the Disease: Curing Chronic Fatigue
AAfter living in Oklahoma for 40 years, Nita and Doug Thatcher retired in 2009 to the Rust Belt city of Lorain, Ohio, a Cleveland suburb that hugs Lake Erie. When Nita needed to find a new primary care doctor, a friend recommended someone from the Cleveland Clinic. Nita knew the institution’s reputation for cutting-edge research and superior medical services. But as a longtime patient grappling with chronic fatigue syndrome, a debilitating disorder that scientists still don’t fully understand, she was wary when she learned that the clinic was promoting a common but potentially dangerous treatment for the illness: a steady increase in activity known as graded exercise therapy.
The notion that people with chronic fatigue syndrome should be able to exercise their way back to health has enjoyed longstanding and widespread support, and “graded exercise” has become the de facto standard of clinical care. This approach has obvious intuitive appeal. Exercise helps all kinds of illnesses, and it’s a great tool for boosting energy. How could it possibly hurt?
British psychiatrists and psychologists developed the graded exercise strategy for treating chronic fatigue syndrome during the 1990s. They offered a straightforward rationale: These patients were not medically sick but severely out of shape (“deconditioned”) from prolonged avoidance of activity. And they avoided activity because they wrongly believed they had a biological disease that would get worse if they overexerted themselves. During treatment, patients were encouraged to question this “dysfunctional cognition,” view any resurgent symptoms as transient, and push through the exhaustion and pain to rebuild their strength.
Today, leading research supporting graded exercise therapy, often called GET, is unraveling, and the scientists behind that research, along with the esteemed journals that published their findings, have come under fire for what have been called dubious study methods and a questionable peer review process. Meanwhile, millions of patients like Nita who are afflicted with chronic fatigue syndrome — a disorder I have covered for nearly a decade as a health reporter, and about which I have sometimes been as much a crusader as a journalist — continue to combat the therapy’s implied prejudices: that sufferers are out of shape but not medically sick, and that increasing exercise levels will help.

The Cleveland Clinic was among many institutions that embraced graded exercise therapy.
Visual: kevinmnord/Flickr/CC
Decades after the enigmatic ailment was first identified, the precise causes of chronic fatigue syndrome remain a mystery, but what is clear is that neither of those assumptions is true. It is very likely, in fact, that the advent of graded exercise therapy, ostensibly designed to free chronic fatigue syndrome sufferers from an array of debilitating physical and cognitive symptoms, instead made them worse — sometimes much worse. And while the hard questions now being raised about this treatment approach would seem a welcome outcome for public health, it’s cold comfort for those patients who have been subjected to it without any sound science to back it up — yet one more insult for those with a disorder that seems to court misunderstanding.
Nita is among them. She had already tried graded exercise therapy before her arrival in Ohio, and it had not gone well. In 1997, after she had been ill for many years, her doctors in Oklahoma prescribed an exercise regimen that left her much more disabled than before. For a couple of years afterward, she could barely leave the house, and she never returned to her pre-GET level of function. Other patients have routinely reported a similar experience: an extended relapse after they pushed themselves beyond their limits, a symptom often called “post-exertional malaise.” In surveys, patients who have undergone GET have been more likely to report that they got worse, not better.
Nita finally enrolled at the Cleveland Clinic outpatient center near her home, but only after grilling her prospective physician to make sure the graded exercise approach was off the table. “I heard some horror tales about the Cleveland Clinic pushing this, and the Mayo Clinic,” Nita told me over Memorial Day weekend, during an interview at her home — one in a series of conversations conducted in recent months via email, on Facebook, and in person. Later on, she added: “A doctor prescribing graded exercise therapy for this illness would be as irresponsible as a doctor prescribing gradually larger doses of sugar for a diabetic.”
At 67, Nita has coped for decades with the extensive physical and cognitive impairments that characterize chronic fatigue syndrome, from extreme and unrelenting exhaustion to difficulties with memory and concentration, among other symptoms. These days, she spends most of her time in her ground-floor bedroom, settled into a brown recliner. She can sustain a lively and engaged conversation for 15 or so minutes, then starts fumbling over words and needs to rest. She can email or chat with friends on Facebook for up to half an hour, perhaps three times a day. She likes reading light romance novels “because they have a happy ending, they’re not draining.” She doesn’t watch TV— trying to keep up with the plotlines is “too stimulating,” she says.

She and her husband Doug, a Methodist minister, live two blocks from a sandy Lake Erie beach, in a modest Craftsman house on a street lined with other modest Craftsman houses — the kind ordered from Sears in the early 20th century. Nita loves the lake. Being in nature has always felt like “coming home” to her, she says: The lake was one reason the couple returned to Ohio, where they’d both grown up. But she rarely sees the water.
To relax and “zone out,” she leans back in her recliner, closes her eyes and remembers the hikes she took in the years when she could still hike, or conjures images of the hikes she has never done.
“I’ve always been an outdoor person,” she says. “In my mind, I still go hiking, on the shore, in the woods.” Online tools help. “Sometimes I’ll take a hike on my computer. I see trails on Google Earth.”
Chronic fatigue syndrome has been controversial ever since the U.S. Centers for Disease Control and Prevention published its first major journal report on the illness, in 1988. For decades, patients have confronted enormous skepticism and doubt about whether their illness even exists. Yet a significant body of research has demonstrated that the disorder has a physiological basis and does not result from deconditioning or psychiatric problems. In August, a study in the Proceedings of the National Academy of Sciences reported finding distinctive metabolite patterns in the blood plasma of patients with chronic fatigue syndrome, suggesting that multiple metabolic pathways are out of whack.
But patients like Nita have long suffered mistreatment and abuse from the medical and research establishments. I visited her last spring, not long after we connected through the extensive online network of chronic fatigue syndrome patients. I was looking for patients whose doctors had prescribed exercise therapy. Nita had read my previous reporting about the illness and was eager to share her story, although she knew being interviewed would tax her resources.
In our communications, I felt guilty whenever I pressed for more information. I knew responding to each question — and Nita responded conscientiously and in-depth — took something out of her.
In an investigation published last year, I looked at some of the major flaws in a British clinical trial called PACE — a large study of treatments for chronic fatigue syndrome.
For my part, I never planned to become “the chronic fatigue syndrome reporter.” Telling news editors you cover chronic fatigue syndrome is not a helpful career move. At a dinner party, the topic is a conversation-stopper. But after a friend got diagnosed with the syndrome many years ago, I knew he was sick because he was sick, not because he was lazy, depressed, or delusional. In 2009, when research suggested that a strain of mouse virus could be implicated in the disorder, I wrote a number of articles about the ensuing scientific controversy for The New York Times. After further studies attributed the apparent mouse virus link to lab contamination and led to retraction of the initial research, public and media interest in the issue evaporated. But I couldn’t shake the story. I knew these people needed medical help. Yet no one seemed to take the illness seriously.
As a result, I’ve been in touch with a lot of chronic fatigue syndrome patients over the years. Some have much more moderate cases than Nita, some more severe. One thing I quickly learned is that many prefer a more serious-sounding name, myalgic encephalomyelitis, which means inflammation of the brain and central nervous system, along with muscle pain. The term, often shortened to M.E., was coined in the late 1950s after an outbreak of illness at a London hospital. It has been listed for decades as a neurological disorder in the World Health Organization disease classification system — although whether the term is an accurate description of the physiology of the disorder remains somewhat open to debate. These days, some government agencies and advocacy groups, in a compromise of sorts, call the disorder ME/CFS.
Last October, Virology Blog, a popular science site hosted by the Columbia microbiology professor Vincent Racaniello, published my lengthy investigation of the major flaws in a British clinical trial called PACE — the largest and, supposedly, the definitive study of treatments for chronic fatigue syndrome. The main results were published in The Lancet in 2011 and the journal Psychological Medicine in 2013. The trial was led by some of the same experts who had developed graded exercise therapy in the first place, and not surprisingly, their publicly reported findings represented an endorsement of their theories about deconditioning and “unhelpful” illness beliefs.
The PACE investigators acknowledged that ME/CFS patients might feel worse after exercise, but they attributed this to the expected effects of deconditioning, not to the exacerbation of an underlying pathology. Anyone who suffered a serious crash after a course of graded exercise, they argued, had most likely received treatment from untrained clinicians. (The investigators have always acknowledged that an acute viral infection or other sickness can trigger the syndrome. The problem, they claim, is that patients continue to insist they have a medical disease long after the initial episode of illness is over.)
Given the paucity of treatment options, medical institutions and public health agencies were promoting exercise regimens even before the 2011 publication of the Lancet paper, largely based on some smaller studies conducted by the same researchers, as well as colleagues who shared their perspective. The reported success of the PACE trial reinforced that trend — although other researchers have found that ME/CFS patients can best avoid relapses and minimize their symptoms, as Nita does, through a popular self-help approach known as “pacing.” Under this strategy, patients learn to accept their limited capacities and adjust their activities so as not to exceed their perceived energy levels, often called their “energy envelope.”
As it stands, the direct cause, or causes, of ME/CFS remain largely unknown, and there is no definitive treatment. But as I investigated the PACE trial — with its promotion of exercise and increased activity as the path to “recovery” from the disorder — I came to view it as a powerful case study of scientific wrongdoing. Thanks to the incisive analyses of some very smart patients and advocates, I gradually understood how deeply flawed it was and how much harm it was causing. I knew it needed to be publicly and authoritatively discredited.
I also knew I needed to be part of that effort.
In the U.S., it is estimated that about one million people suffer from chronic fatigue syndrome, and millions more suffer worldwide, although many cases remain undiagnosed. Women are two to four times as likely to have the illness. Some patients, like Nita Thatcher, are so debilitated they remain mostly homebound for months or years at a time. Doctors often regard the symptoms as psychosomatic, imaginary, or a sign of mental distress. Patients routinely confront disbelief and ridicule from employers, friends, even family members.
The CDC first investigated the illness in the 1980s in Incline Village, a Lake Tahoe resort town in Nevada. One hundred and sixty residents had flocked to local doctors’ offices, suffering from what appeared to be a persistent viral infection resembling mononucleosis or a nasty, non-resolving flu. However, the CDC team did not confirm a viral link. In the 30 years since, federal researchers have failed to identify any causes, diagnostic markers, or drug treatments — an impressive trifecta of non-accomplishment.
A report last year from the Institute of Medicine portrayed chronic fatigue syndrome as an organic disease marked by major immunological, neurological and cognitive abnormalities.
Last year, however, the scientific terrain shifted sharply when the U.S. Institute of Medicine and the U.S. National Institutes of Health both released high-profile reports about the illness, based on extensive reviews of the literature. In contrast to the arguments of the British researchers, the reports portrayed ME/CFS as an organic disease marked by major immunological, neurological and cognitive abnormalities.
In fact, the IOM report identified the distinguishing symptom as “exertion intolerance,” another name for post-exertional malaise — a sustained physiological crash that can occur after even minimal amounts of activity. In focusing on this phenomenon, the report confirmed what patients like Nita have long understood — that expending too much energy and ignoring the body’s warning signs only makes them sicker. In other words, continuing to exercise despite an increase in fatigue, pain, and other symptoms could do more harm than good.
“The rigid approach implies that those who get sicker after exercise and can’t continue with GET are somehow to blame, giving up too readily and therefore complicit in the perpetuation of their disability,” Peter Rowe, a Johns Hopkins pediatrics professor and ME/CFS expert who served on the Institute of Medicine panel, wrote in an email.
“The assumption that deconditioning is the cause of all symptoms ignores the potential contribution of other unrecognized biomedical problems (and ignores much of the research produced in the last 20-plus years),” he added.
While the exact causes of ME/CFS have yet to be pinned down, most cases arise after acute infectious illnesses; experts believe that exposures to other physiological insults, such as environmental chemicals or mold, could also play a role. Research has shown that even after the initial event has passed, patients’ immune systems often appear to be in a state of hyperactivation, as if their bodies are still responding to an external threat. In some tests patients also exhibit dramatically reduced levels of energy production when they engage in exercise two days in a row, compared to healthy controls. Genetic susceptibility is also believed to be a factor. Some researchers are exploring whether ongoing infections with known or unknown pathogens play a role. In addition to the recent study on metabolites, scientists from Columbia, Stanford, Cornell, and elsewhere have reported significant findings that could ultimately lead to diagnostic tests and possible drug treatments.
In recent years, the NIH has spent about $5 million annually on researching ME/CFS, far less than for many diseases with far fewer sufferers. Last October, following the release of the two U.S. reports, the agency announced plans to step up its efforts to find answers. “Of the many mysterious human illnesses that science has yet to unravel, ME/CFS has proven to be one of the most challenging,” said NIH Director Francis Collins, in a statement. The agency has since started its own study and says it is looking into other ways to support research.
Nita and other patients welcome the new research but say the government has let them down repeatedly. Without sufficient funding to pursue promising leads, Nita said, the recent initiative “won’t count for diddly squat.”
In any event, Nita recognizes, future advances will not bring back the decades scarred by sickness. She doesn’t usually discuss the issue in such depth, she tells me in one of our 15-minute sessions, so being interviewed is surprisingly emotional for her. “It’s a gut-level confrontation with the disease that I don’t put myself through very often,” she says of our conversations. “Sometimes the sense of loss and alienation from the life that I expected has just grabbed me by the throat and told me ‘This is your reality.’”
Despite the uncertainty over causes and the widespread evidence that exertion can be harmful, the exercise therapy pioneered and promoted by British mental health experts has emerged as the dominant treatment model. The Mayo Clinic, WebMD, Kaiser Permanente, and the CDC, among others, promote it on their websites. (The Cleveland Clinic, where Nita Thatcher is still a patient, highlighted graded exercise therapy in an online training module for the illness, which expired in 2014 and has not been replaced.) The American Academy of Family Physicians and the American College of Physicians endorse the treatment. So do UpToDate, a popular commercial site that provides advice on clinical decision-making, and Healthwise, a nonprofit that disseminates information to medical providers. These sites and organizations generally use the name chronic fatigue syndrome, not ME/CFS.
The most prominent evidence for graded exercise therapy comes from the PACE trial, the focus of my extensive reporting last year. (PACE is the shorthand name for the full title of the study as it appeared in The Lancet: “Comparison of adaptive pacing therapy, cognitive behavior therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome: a randomized trial.”) The PACE investigators reported that both graded exercise therapy and a second treatment, cognitive behavior therapy, were moderately effective in improving symptoms.
The trial’s three principal investigators — psychiatrists Peter White and Michael Sharpe, and behavioral psychologist Trudie Chalder — are highly influential in British academic and medical circles. For many years, they have advised government agencies and insurance companies that their behavioral and cognitive approach to treatment could improve the health of ME/CFS disability claimants and get them back to work. Their ideas have heavily influenced medical treatment and public attitudes towards the illness. They designed the trial hoping to demonstrate that the benefits they were claiming for their treatments were real.
British government agencies spent £5 million ($6 million today) on the trial, which recruited 641 participants from specialized clinics, starting in 2005. Participants were randomized into one of four treatment groups and followed for a year. Besides the groups receiving graded exercise therapy and cognitive behavior therapy, a third group received “adaptive pacing therapy,” an intervention based on the pacing approach. However, in transforming this self-help technique into a structured “therapy” — with diaries and advance planning and a “therapist” providing supervision — the PACE researchers changed it enough to make it difficult to compare to the actual symptom-management strategy used by patients.
In a 2011 video produced by The Lancet, Michael Sharpe and Trudie Chalder speak at a press conference outlining the PACE trial and its findings with regard to graded exercise therapy.
Participants in all three intervention arms received up to 15 therapy sessions. They were also offered “specialist medical care” — at least three sessions with a doctor who had expertise in the illness. A comparison group received only the specialist medical care. According to the 2013 paper in Psychological Medicine, 22 percent of those receiving either graded exercise therapy or cognitive behavior therapy “recovered,” about three times the rate in the other two groups.
Unlike large pharmaceutical trials, in which no one knows who is getting the drug and who is getting the placebo, PACE was non-blinded; that is, participants knew which treatment they were receiving and clinicians knew which treatment they were delivering. Non-blinded studies are considered highly vulnerable to bias, especially when the primary outcomes, as in PACE, are subjective.
Cognitive behavior therapy, often called CBT, is designed to help people cope with any number of adversities, including sickness. But PACE presented the therapy differently — as a path toward a full return to health. Like graded exercise therapy, the PACE version of cognitive behavior therapy was geared toward reversing the deconditioning presumed to lie at the heart of the illness. The treatment sought to help participants abandon the belief that they suffered from an organic disease requiring them to rest, at the same time promoting increased activity and a return to regular routines. The various U.S. medical organizations and treatment guidelines, from the CDC and elsewhere, generally recommend cognitive behavior therapy as well as graded exercise.
But the PACE study suffered from such serious flaws that its reported results are uninterpretable and meaningless. Its main claims of success rested on a mind-boggling paradox: In some cases, even if participants got worse during the trial on the two primary outcomes of physical function and fatigue, they could still be deemed “recovered” on these measures. How? Because the investigators’ criteria for “recovery” were so broad that they represented worse health than the entry criteria for serious disability. In fact, 13 percent of the PACE participants qualified simultaneously as being disabled enough to be in the trial, but already “recovered” for physical function or fatigue before any treatment at all — an astonishing fact not disclosed in the published papers. Instead, at the press conference presenting the Lancet paper, co-author Trudie Chalder declared that “twice as many people on graded exercise therapy and cognitive behavior therapy got back to normal.”
In addition to these nonsensical overlapping thresholds for entry and “recovery” on the primary measures of physical function and fatigue, my PACE investigation documented many other flaws, including these:
• After the trial began, the investigators weakened their standards for success by dramatically revising their methods for assessing “improvement” and “recovery,” which bolstered their chances of being able to report positive findings. They did not provide the results they originally promised in their trial protocol nor did they include sensitivity analyses, the standard statistical tests for assessing whether such significant protocol changes produced more favorable results.
• During the study, the investigators published a newsletter for participants that included glowing testimonials from earlier participants about their positive outcomes, potentially biasing the responses of the many remaining subjects.
• While physical functioning and fatigue were subjective outcomes assessed with self-reported questionnaires, the investigators disavowed their own objective measures, like a walking test and employment status, as irrelevant, inaccurate, or otherwise flawed — after all these measures failed to demonstrate “recovery.”
• Even though the investigators promised in their trial protocol to disclose “any possible conflicts of interest” and “institutional affiliations” while obtaining informed consent, they failed to tell prospective participants of their close ties to disability insurers — to whom they had long been promoting the very treatments being studied.
In addition, the PACE investigators identified participants using only a single symptom to diagnose the illness — six months of disabling, medically unexplained fatigue. Other common definitions require multiple symptoms. Last year’s NIH report found that using a broad definition focused on fatigue, as was done in the PACE trial, can generate study populations that include an unknown number of people who do not have ME/CFS but instead suffer from other fatiguing illnesses, including major depressive disorders. (In contrast, ME/CFS patients can suffer from what is often called secondary depression — that is, they are depressed because they have a chronic illness, and especially one that many people deny exists.)
Exercise and psychotherapy are known to benefit people with depression. If participants in an ME/CFS trial are actually suffering from a major depressive disorder but not from ME/CFS, then treatments that benefit them could be misinterpreted as beneficial for ME/CFS patients. Given the difficulty of understanding results from heterogeneous samples, the NIH report concluded that the PACE definition, called the Oxford criteria, could “impair progress and cause harm” and should be “retired” from use. (The PACE trial also included two subgroup analyses of participants defined using more specific definitions, but other researchers have dismissed these subgroup analyses as unreliable.)

In February, as a result of my reporting, 42 scientists, academics and ME/CFS clinicians posted an open letter to The Lancet on Virology Blog, declaring that PACE’s methodological lapses “have no place in published research.” The letter, which I helped to orchestrate, urged the journal to seek a fully independent review of the trial. The investigation also prompted a dozen ME/CFS advocacy groups to warn U.S. health officials that “continuing to use PACE and similar Oxford definition studies to support treatment recommendations for all ME/CFS patients is an issue of grave concern.”
The letter asked them to take steps “to best protect patients.”
In response, the Agency for Healthcare Research and Quality, which had recommended graded exercise therapy and cognitive behavior therapy, recently reversed itself. In a new analysis excluding PACE and other Oxford-criteria studies, the agency found no evidence that graded exercise therapy was effective and minimal evidence for cognitive behavior therapy.
For years, patients have clamored for the PACE investigators to publish the results they promised in their protocol, using their original standards for success. The authors refused. Patients filed requests for anonymized data and other trial documentation under Britain’s freedom-of-information law. Most requests were rejected by Queen Mary University of London, the professional home of lead investigator Peter White.
In September, the university finally released some PACE trial data under a court order involving a freedom-of-information request that a patient had pursued for two years. A small group of patients and academic statisticians analyzed it and published their findings on Virology Blog. And with that, the PACE trial’s 22 percent recovery rates “went up in smoke,” wrote Julie Rehmeyer, a journalist who is also an ME/CFS patient, in a compelling article on how “bad science misled millions” for STAT, a health news site connected to The Boston Globe. In fact, in the new analysis the “recovery” rates fell to single digits, and the results were not statistically significant.
In their own re-analysis of the results, posted online by the university, the authors reported that with the original protocol methods, the graded exercise therapy and cognitive behavior therapy groups were still more likely to produce “improvement” than the other two groups, at a rate of about 20 percent. Patients quickly pointed out that this was a third of the “improvement” rates the PACE team had reported in The Lancet.
Ronald Davis, the renowned Stanford geneticist, told me last year for the Virology Blog investigation that the PACE study “has so many flaws” and that he didn’t “understand how it got through any kind of peer review.” He began investigating ME/CFS himself after his son fell seriously ill a few years ago, and works with the Open Medicine Foundation, a California-based research group focused on the disease. Davis said leading medical organizations and institutions should have scrutinized and assessed the study themselves before adopting its recommendations
“You can’t just say it’s in the literature, so it must be right,” said Davis, who also served on the IOM panel. “You need to read the study and make your own decisions.”
“It shouldn’t have been published,” he added.
Bruce Levin, a Columbia biostatistician who worked with patients on the new “recovery” analysis, reviewed the PACE trial last year at my request and condemned its many methodological lapses. “We all seem to agree that medicine should be based on evidence,” he said in a phone interview for this article. “And if the evidence is faulty, then how can you make guidelines based on faulty evidence?”
To cite the questionable results from PACE as evidence for clinical guidelines, he said, is “ludicrous.”
Levin, Davis, Racaniello, and I are currently seeking additional PACE trial data under the U.K.’s freedom of information law. Queen Mary University of London turned down our request, and we have appealed. Meanwhile, the PACE principal investigators — White, Sharpe and Chalder — did not answer multiple email requests seeking comment for this article. Neither did Richard Horton, editor of The Lancet.
Last fall, Virology Blog posted the PACE team’s response to my investigation, along with my rebuttal of that response.
Nita and Doug Thatcher have been together for half a century. For most of that time, she has been ill — sometimes functioning reasonably well, sometimes barely able to get up. Doug is 69, two years older than Nita. Easygoing and self-deprecating with calm gray eyes, he smiles and chuckles when he talks about his wife.
He tells me he is Nita’s “lover, friend, helper.” She calls him “my rock” and “that solid core of warm gold at the center.” She considers herself luckier than many: She’s heard too many stories of people with ME/CFS deserted by spouses, children, friends and colleagues.

Nita and Doug have been together for over half a century. Above, the couple are seen with their grandson, Michael. Below, at a family reunion in 2010. (All family photos courtesy of Nita Thatcher.)
Nita was always blessed with “plenty of spizzerinctum,” says Doug. He heard an old preacher use that word once and thought it captured his wife’s sparkle and vitality, the qualities that drew him to her. Doug says he sees the same person when he looks at Nita now. He laughs. “More weight, bless her heart!” Then he adds: “I see the same person, in jail. Confined, sometimes — in solitary confinement.”
Doug and Nita have maintained separate bedrooms for many years. Her illness already made it hard for her to get a good night’s rest, and then his snoring compounded the problem. That did not end their sex life, but Nita’s health once again declined after the move to Ohio. Several years ago, she found that experiencing an orgasm could push her body into a bad relapse, so they stopped having sex. “That’s been hard,” she says wistfully. Luckily, hugging and kissing are still possible. “You just find ways to be intimate,” adds Doug.
She stays as active as she can without exceeding what she knows is her limit. Several times a day, she braves the journey from her recliner to the front door and back. The path snakes through the kitchen, den, and living room. At her best, she can make the trip without a rest. During weaker periods, she leans on countertops, walls and furniture, as needed. The round trip takes about 100 steps. Her current daily maximum is 800 to 1,000.
Like others with the illness who practice pacing, Nita is attuned to her body’s shifting sensations; that’s how she knows when to rest. “I’m a Type A-minus personality,” she says, very much the type to push through difficult situations. (The “minus” helps “to take off the obnoxiousness of being a Type A personality.”) But if your body tells you to stop, she explains, the worst thing someone with ME/CFS can do is try to push through.
Nita has a full, round face and a welcoming gaze. During one of our conversations, she wears a large turquoise robe that billows over the recliner, with a magenta shawl around her shoulders. She sits with her legs stretched forward, crossed at the ankles. In her younger years, with a 36-22-36 figure, she would have been described as buxom. But prolonged inactivity, among other factors, has altered her proportions. These days she weighs 270 pounds — twice what she considers optimum.
“I was not obese till my mid-50s,” she says. She knows the extra weight exacerbates her medical problems. She’s 30 pounds down from what she was at her highest.
Nita can find much of what she needs in the cabinets and drawers on either side of her recliner — sewing items, toiletries, a blood pressure monitor, medication, hair rollers, stationary, pens and pencils, a stapler. Books she might want — about arts and crafts, for example — are within easy reach. The bed and bathroom are each a few steps away, the kitchen only a bit farther. “This is my life now basically,” she says in a voice layered with acceptance, surprise, sadness. “This room.”
The Thatchers have six grandchildren, so some of her shelves are stacked with pop-up books — “20,000 Leagues Under the Sea,” “Star Wars,” books about ancient Egypt, and Pompeii. The grandkids have adapted to her illness, but it pains her that “they know me as a sick grandma — that hurts more than a lot of other things,” she says. “You like to think you pass certain things on to children and grandchildren. I wanted to pass on how to have fun, how to enjoy life. I don’t know if I’ve been successful in that.”
To help her grandkids understand her situation, Nita used a teaching tool she came across online. She spread out a batch of spoons on the floor, explaining that each one represented a certain amount of activity. Healthy people have a lot of spoons they can use every day. Currently, Nita figures she has, at most, 13: fixing a frozen meal uses up a spoon, for example, as does every 15-minute conversation. “You want me to push you around the playground, I need to take three of my spoons,” she told her grandkids. Even the youngest, Hayden — 4 at the time — grasped the concept.
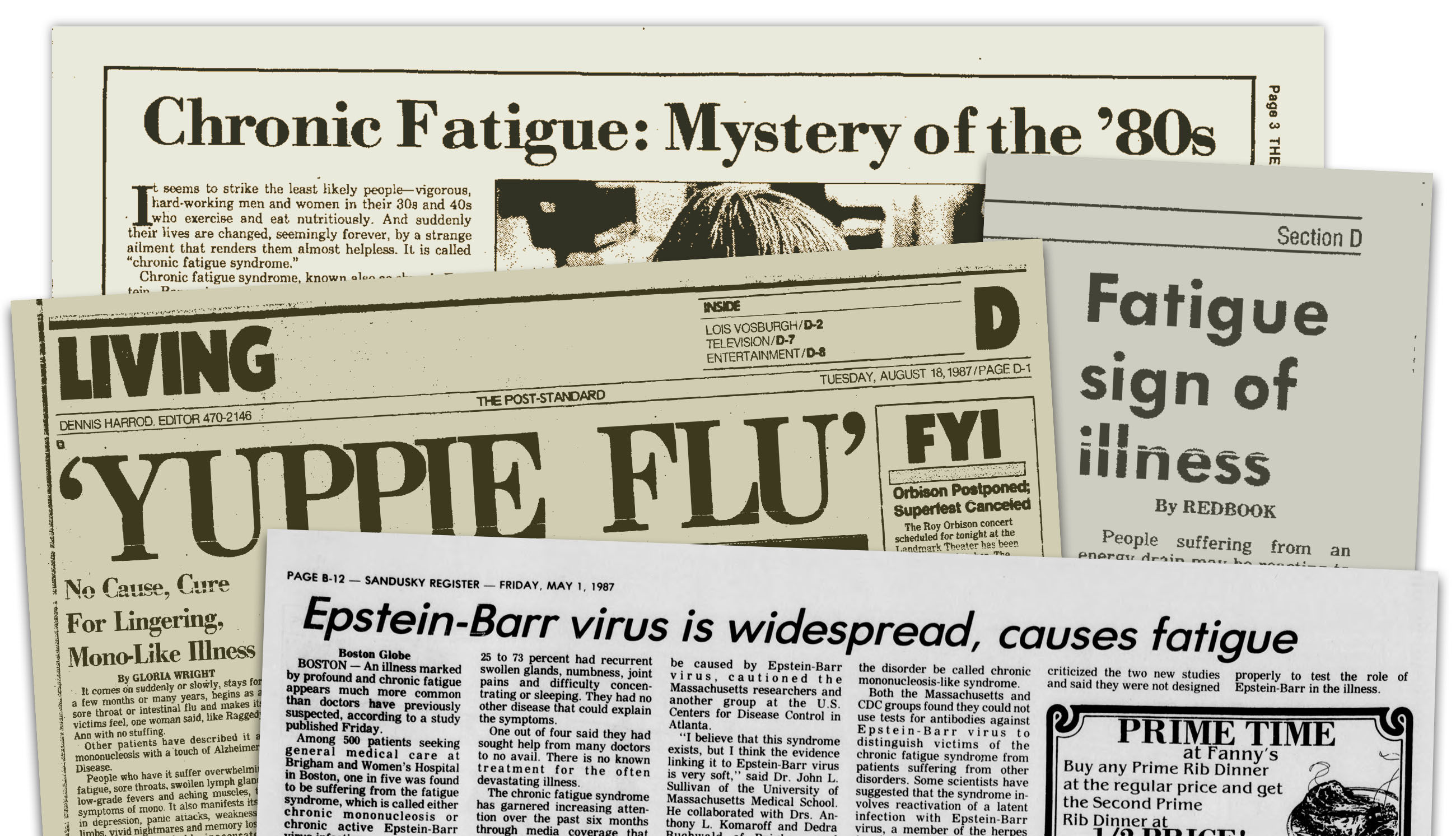
It is hard to overstate how much patients hate the name chronic fatigue syndrome. The reported outbreak in Incline Village in the mid-1980s appeared to be linked in many cases to the Epstein-Barr virus, which causes mononucleosis. But the CDC investigators disputed the role of the pathogen in the cases they reviewed and declined to officially name the illness chronic Epstein-Barr virus syndrome. Instead, in its 1988 paper, the CDC-led team settled on chronic fatigue syndrome.
For patients, the name designated by the CDC has been a disaster. For one thing, it conflates “chronic fatigue,” which is a symptom of many conditions, with the specific illness known as “chronic fatigue syndrome,” creating the false impression that the latter is essentially an extended case of the former. Moreover, the common meaning of the word “fatigue” does not come close to conveying the paralyzing exhaustion that patients routinely describe. Because of these misunderstandings, patients say the name has distorted public perceptions and affected how their doctors treat them, how much money is spent on research, and how their families and friends respond.
Laura Hillenbrand, author of the best-sellers “Seabiscuit” and “Unbroken,” and probably the best-known person with the disease, has called the name “condescending” and “misleading.” “The average person who has this disease, before they got it, we were not lazy people,” she told The New York Times in 2011. “This disease leaves people bedridden. I’ve gone through phases where I couldn’t roll over in bed. I couldn’t speak. To have it called ‘fatigue’ is a gross misnomer.”
Beyond the name, the issue of how to define the illness has bedeviled the field and hampered research. In 1994, a CDC-led team published the most widely used definition. To receive a diagnosis, patients must have experienced six months of unexplained, disabling fatigue, as in the Oxford criteria used in the PACE trial. However, they must also display any four of eight other symptoms: post-exertional malaise, unrefreshing sleep, problems with memory or concentration, muscle pain, joint pain, headaches, tender lymph nodes, and sore throat.
Although the CDC definition, unlike the Oxford criteria, requires multiple symptoms, many experts have still criticized it as imprecise. They argue that several of those eight symptoms — such as post-exertional malaise, unrefreshing sleep, and problems with memory or concentration (or other cognitive functions) — are central to the disease and should be required, not optional. Many patients and clinicians prefer two more detailed and precise definitions published in 2003 and 2011.
Ever since the CDC coined the unpopular name, patients and advocates have faulted the U.S. government’s incompetent response. In “Osler’s Web,” a prodigious feat of investigative reporting published in 1996, the journalist Hillary Johnson documented how top health officials dismissed the significance of the illness and neglected promising leads. In the late 1990s, the CDC was found to have diverted tens of millions of dollars that Congress had designated for chronic fatigue syndrome into other programs. In the 2000s, the agency focused on stress-related and psychological aspects of the disorder, to the dismay of patients. A much-ridiculed paper in the journal Psychotherapy and Psychosomatics asserted that patients suffered from “maladaptive personality features,” and in particular from higher rates of “paranoid, schizoid, avoidant, obsessive-compulsive, and depressive personality disorders.”
Since 2012, the CDC has been conducting a study designed to gather standardized medical information on as many as 450 patients, drawn from the practices of several clinicians experienced at treating ME/CFS. The agency hopes the results will more clearly define the disorder, identify possible subgroups, and illuminate the underlying physiology, but to date no actionable information has been published.
Nita and Doug both grew up in strict religious homes, and both learned to question the unforgiving doctrines and literalist biblical beliefs their families tried to instill. She met him when she was 11, at a church summer camp. (“Oh, my Lord, what was Nita like when I met her? A stringbean, a wiry, vivacious young lady,” recalls Doug.) They began dating six years later, in 1966. As a high school senior, she chafed under her mother’s strict control. He was already off in college. The week after graduation, she left home to be near him and escape her mother’s dictates.
Although the couple shared a strong emotional and physical bond, and got engaged quickly, Nita insisted on delaying the wedding for more than a year, to make sure Doug would respect her as an equal partner. “I grew up with a strong reliance on my own intellect and a great deal of determination not to be dominated or manipulated,” she says now.
They married in the summer of 1968. Instead of continuing with college, Nita worked to support her husband’s studies, first in Michigan and then in Oklahoma, where he attended divinity school. Within a few years, they had two young children — Julie, born in 1971, and John, born two years later.
Many ME/CFS patients can identify a particular point when their illness began. They got sick from an acute viral infection or something else — and then when they should have gotten better, they didn’t. But some people, like Nita, report a more gradual decline. A few years after she married Doug, she experienced a terrible bout of flu, followed by her difficult second pregnancy. She recovered from both. But afterwards, in her late 20s, she started to drag. She never seemed to have as much energy as she should.




She noticed it especially while playing volleyball and tennis — two favorite pursuits. She felt sluggish, always slow to reach the ball. Then the muscle aches started. And she began having trouble getting a refreshing night’s rest. The doctors couldn’t figure it out. The tests all came back negative. For several years, she took medication to help her sleep. Then the medication stopped working.
Nita managed, more or less, for the next 15 years. She learned to rest when she needed to. Sometimes her energy levels improved for months at a time, and she was able to hike and camp out, within limits. She wrote and directed some church musicals and community theater productions, always struggling but managing somehow.
As her illness fluctuated, Nita adapted to its rhythms. For a while she took college classes again, then realized she was overdoing it — she still had two little kids around — and stopped. In the early 1980s, she recovered enough to work full time in the auto-financing industry, reviewing contracts. Then she got worse again and quit. Later still, she started her own costume-making business; she loved the work, and being her own boss allowed her to control the hours. And always, Doug was willing to pick up the slack. “I knew she had a lot more limitations and was dealing with something serious and mysterious,” he says.
Nita kept seeking out information and answers. She recalls that at one point in 1989, she was listening to a talk show and heard about a new illness called chronic fatigue syndrome. The description sounded similar to what she had been experiencing for more than a decade. But she thought the name was insulting, trivializing — “like a slap in the face.”
In 1989, the year after the CDC-led team selected the term chronic fatigue syndrome, four British researchers — Simon Wessely, a psychiatrist; Trudie Chalder, the psychologist and future PACE investigator; and two colleagues — proposed an explanation for the ongoing disability of patients with the condition.
“A model is outlined of an acute illness giving way to a chronic fatigue state in which symptoms are perpetuated by a cycle of inactivity, deterioration in exercise tolerance and further symptoms,” they wrote in the Journal of the Royal College of General Practitioners. “This is compounded by the depressive illness that is often part of the syndrome. The result is a self-perpetuating cycle of exercise avoidance.”
Because patients were presumed to wrongly believe that they suffered from a medical disease, the authors proposed treatments that focused on both psychological and behavioral approaches. “Cognitive therapy helps the patient understand how genuine symptoms arise from the frequent combination of physical inactivity and depression, rather than continuing infection, while a behavioral approach enables the treatment of avoidance behavior and a gradual return to normal physical activity,” they wrote.
Wessely, Chalder, and their colleagues — including White and Sharpe, Chalder’s PACE co-investigators — have since collectively written hundreds of articles, studies, and reports, a great many of them promoting what they call the “biopsychosocial” theory of the illness, focused on false cognitions, avoidance of exercise, and deconditioning. They have attained leading positions at well-known academic and medical institutions. They have also cultivated close consulting and financial relationships with British health agencies as well as disability insurance companies. (Wessely was deeply involved with PACE but is not a co-author. He is considered a founder of the cognitive-behavioral approach to treating ME/CFS and is currently president of the Royal College of Psychiatrists, the U.K.’s national professional association.)
These mental health professionals have long blamed what they call the “M.E. lobby” — that is, patient activists and advocacy groups — for enabling, supporting, and reinforcing claimants’ delusions of having an ongoing, unresolved disease. The provision of state and private disability benefits, and other financial, social and psychological factors, Sharpe wrote in a 2002 UNUMProvident report on disability insurance trends, could also impede both the patient’s own recovery and the effort to resolve insurance claims.
“A strong belief and preoccupation that one has a ‘medical disease’ and a helpless and passive attitude to coping is associated with persistent disability,” Sharpe warned in the report.
Mary Dimmock, a former scientist and business analyst at Pfizer, has become a patient advocate after her son fell ill with chronic fatigue syndrome. Here, she discusses the lack of funding for basic research into the disorder.
“The current system of state benefits, insurance payments and litigation remain potentially major obstacles to effective rehabilitation,” he wrote.
Some early studies from these and other investigators showed that treating patients with cognitive and behavioral therapies could improve subjective responses on questionnaires about fatigue, physical function, and other health indicators. However, results for objective measures of improved function proved disappointing. In 2003, the Medical Research Council, a U.K. government body that supports health research, announced that it would fund a clinical trial to determine once and for all which treatments were effective. Three other government agencies agreed to contribute funding, among them the Department for Work and Pensions, charged with handling state disability issues.
The work and ideas of these British clinicians have had a major impact on treatment, and not just in Britain. Over the years, they have collaborated closely with experts at the NIH and CDC. The flood of studies and papers they produced throughout the 1990s touting their theory and approach found a receptive audience among U.S. health officials and medical professionals.
Mary Dimmock, a former scientist and business analyst at Pfizer who became a patient advocate after her son fell ill, has researched the development of U.S. health care policy toward ME/CFS. “At least by the early 1990s, key players in research in the U.S. had embraced the idea of [false] illness beliefs and deconditioning,” she said in a phone interview. By the mid-1990s, she added, clinical guidelines for doctors began placing a “heavy emphasis” on graded exercise therapy and cognitive behavior therapy.
Dimmock and her son, Matthew Lazell-Fairman, have documented the government’s decades of neglect of the illness in a self-published report, “Thirty Years of Disdain: How HHS and a Group of Psychiatrists Buried Myalgic Encephalomyelitis.”
In the mid-1990s, after years of suffering from the extended and unexplained lapses in energy, Nita, then in her 40s, finally received an official diagnosis. Her doctor had already told her he believed, as did she, that she had the illness she’d heard about — chronic fatigue syndrome. By then, the term had become widely known, although the condition was commonly derided as “yuppie flu.”
The doctor referred her to a local psychiatrist, who ruled out depression as a cause and formally identified her condition. Then he told Nita the good news: British experts had found that patients improved significantly after a regimen of gradually increasing exercise. He sent her to a physical therapist familiar with the technique. “It was all the rage in the U.K., according to the therapist, and showing great results,” she says. “He was gung-ho on it.”
Nita was skeptical. At this point, she felt she was operating at about half her pre-illness energy level — not great, but good enough. She made sure to take two eight-minute walks a day. That was as much exercise as she felt her body could handle, and she feared testing the limits. But her primary care doctor also urged her to give the treatment a chance, and the psychiatrist insisted it would help her, so she agreed.
The physical therapist directed her to increase the twice-daily walks to as long as 15 minutes over the course of six weeks, and to add resistance and stretching exercises. She followed his instructions but felt she was sliding downhill. “After three weeks, I said, ‘I don’t know if I can handle it — the pain is worse, the fatigue is worse,’” she recalls. “He said, ‘We just need to tweak it.’ He said, ‘This is working really well in the U.K. and it will work for you.’”
But after more weeks of dragging herself through a shortened exercise regimen, she suffered a complete crash. Her body refused to do more, and she quit the program. The physical therapist would not sign documents supporting Nita’s request to seek disability. He insisted she keep going, that she needed to stick with the routine. “I just about told him where he could shove that,” she says.
The psychiatrist also refused to sign any disability forms. “He told me he wouldn’t be helping me with disability because I wasn’t trying to get well with a proven course of action,” she explained in an email. Her primary care doctor knew she’d given the exercise program a serious chance, so he was willing to sign the required documents.
The post-exercise crash knocked Nita way below her previous middling level — to about 15 percent of her pre-illness state, she estimates. She stopped her various activities and mostly rested, sparing time only for family visits. Gradually, over two or three years, she regained some of the energy she’d had before the crash. But she never regained it all.
She could no longer play softball or tennis, but she was once again able to participate in local theater groups. She didn’t have the strength to sew all the costumes, but she still loved to design them. And best of all, she found herself able to hike and camp again, as long as she made sure to take long rests.
While Nita and others have found that pacing helps control their symptom flare-ups, the PACE results convinced many medical authorities that the strategy doesn’t work — even though the trial did not test pacing as a self-help technique but instead assessed the investigators’ highly structured version of it. Meanwhile, graded exercise and cognitive behavior therapy continue to be widely recommended.
In the summer of 2015, experts at the Mayo Clinic in Rochester, Minnesota, told Rachel Riggs, a San Diego entrepreneur and business consultant who had suffered from exhaustion and other symptoms for years, that she had chronic fatigue syndrome. The Mayo website recommends graded exercise and cognitive behavior therapy. But instead of entering the clinic’s own rehabilitation program, which included activities designed to counter deconditioning, Riggs asked for advice on pursuing a home-based regimen modeled on the Mayo approach instead. She followed the instructions carefully, she says, alternating between aerobic exercise and yoga — and relapsed badly after a month.
“Total zombie,” she recalled in a recent Facebook exchange. “I was having trouble thinking and processing complex ideas, and severe sensitivity to any stimulus. … If someone sneezed unexpectedly, it was as though I was on the firing squad in Afghanistan.”
In desperation, she decided to enroll in Mayo’s rehabilitation program after all — and then, just before leaving home, conducted some online research. For the first time, she read about post-exertional malaise and the controversies surrounding the PACE trial. So she canceled the Mayo program and sought treatment with well-regarded ME/CFS specialists instead. Although somewhat improved after months of rest and treatment with an immune modulator, she has still not recovered her pre-crash level of function.
She used to walk 20 minutes every morning, but that remains beyond her current capabilities. With the crash, she also suffered some loss in cognitive function. “My brain has been toast since then,” she wrote. “I feel as though I have lost about 20 I.Q. points.”
Obtaining satisfactory responses (or any responses at all) from medical institutions about the PACE trial is surprisingly challenging. Despite its prominence, no one appears willing to defend it directly.
Eileen Sheil, a spokeswoman for the Cleveland Clinic, confirmed that the medical center no longer offers the online training module promoting GET and CBT. But she failed to respond to repeated requests for information about the clinic’s current treatment protocol. Kaiser Permanente, UpToDate and Healthwise did not respond to multiple requests for information about their continued support for the PACE interventions. A spokeswoman for the Mayo Clinic emailed that “we are not interested in participating in your story.”
In response to questions about the study’s documented flaws, the CDC’s Division of High Consequence Pathogens and Pathology, which oversees ME/CFS, emailed a statement explaining that the agency “was not involved in the PACE trial and is therefore unable to offer its opinion on its efficacy or integrity.” The statement did not explain why the agency’s non-involvement in PACE automatically neutered its ability to assess the integrity of a study in which some participants were already “recovered” on the primary measures at the start.

Nita says she knows many things are not within her control, including her chronic fatigue syndrome. But she is determined to stay upbeat.
Visual: Michael McElroy for Undark
The CDC statement also noted that the agency “is committed to providing guidance based on the most up-to-date, evidence-based science available.” Yet it did not explain why the website still recommends treatments — specifically graded exercise and cognitive behavior therapy — for which the main evidence comes from PACE and other studies using the Oxford criteria. Among the most “up-to-date, evidence-based science available” about Oxford criteria studies comes from last year’s NIH report, which found that they could “impair progress and cause harm” because the samples included people without ME/CFS.
Mary Dimmock, the patient advocate and former pharmaceutical scientist, has repeatedly complained to federal health authorities that the treatment recommendations are based on lumping together incompatible studies.
“Evidence-based guidelines should be based on studies in patients who actually have the disease for which the guidelines are being developed,” she said in a phone interview. “But if you mix and match the results from studies that don’t include the same set of patients, then the treatment recommendations that you develop are not necessarily valid for the group of patients they’re intended for. It would be like developing cancer recommendations based on heart patients.”
One afternoon, while Nita rests, Doug is sitting on the white wicker chair on the front porch, smoking a Pall Mall. Doug has diabetes. He knows smoking isn’t good for him, and it bothers him that he can’t quit.
After 40 years serving multiple congregations in Oklahoma, Doug is glad to be back in Ohio. He hopes to see more of their family. Their daughter, a property manager, lives with her family in Columbus, an easy drive to Lorain. Their son, his wife, and their kids had also moved to Ohio in 2009, but they are now living back in Oklahoma.
Doug tells me he has always made sure to maintain his own interests, and he continues to do so in retirement. He plays tennis. He hangs out with friends. He tends his collection of hundreds of vinyl records, browsing in record shops and attending flea markets and record conventions. Like his wife and both kids, he is a big Queen fan.
I ask Doug how Nita’s illness has affected him, and how he has reconciled their situation with his faith. He’s never been prone to depression, says Doug, and it’s not his nature to worry much about the future. But dealing with Nita’s situation has forced him to become much more patient over the years. It’s also forced him to be a better cook, he says with a chuckle.
And despite Nita’s disability, he marvels at her spirit and ability to cope. “She’s able to maintain an equilibrium and balance in the midst of all this that I think is highly unusual for being so limited,” he says, his voice tinged with awe. “She accepts what she’s got, but she’s not caving in to it.”
As for his faith, it has always been “a questioning faith,” he says. “God in our view is big enough that we can shake our fists once in a while,” he says. “It’s OK to cuss and say, ‘What the hell are you doing to me?’ If God’s not big enough to be questioned or screamed at, then God’s not big enough.”
Mostly, he and Nita have managed to adjust their lives to the changing circumstances. Usually he’s reconciled to it. But not always. Human beings are good at feeling sorry for themselves and holding “a pity party,” he says, and he’s no exception. “There are a few times when I feel I really don’t like all this being on my shoulders,” he says. “I experience that thought from time to time: ‘That sucks!’ So I say it out loud, and it’s over.”
For her part, Nita knows that her health could continue to decline. She knows something could happen to Doug. She’s a pragmatist. From her recliner, she has mapped out and priced possible future living arrangements. She knows many things are not within her control, but she remains determined, she says, to seek “as much joy as I can,” despite her circumstances. “I have enough faith in myself” — she pats her chest — “that I’ll find a way. I’m not sure how. But I’ve done it so far, and I’ll keep doing it.”
David Tuller is a lecturer in public health and journalism at the University of California, Berkeley. He has been a staff reporter and editor at both The San Francisco Chronicle and Salon.com, and he has been a frequent contributor to The New York Times and other publications. At Berkeley, he receives support from a Kaiser Permanente grant to the Graduate School of Journalism.










Comments are automatically closed one year after article publication. Archived comments are below.
Another significant help could be Dr. Lisa Sanders’s column for The New York Times Magazine: “Diagnosis.” Here she describes different people’s symptoms, still without a diagnosis by doctors. She invites people and doctors around the world to contribute their experiences and findings to try and solve the medical problems. This would be a good forum for ME/CFS sufferers to describe their symptoms and ask for help. Many unknown medical conditions have been resolved with this column.
Introducing ‘Diagnosis,’ a New Show From The Times and Netflixhttps://www.nytimes.com › 2019/07/22 › magazine › diag…
Jul 22, 2019 — The documentary series based on Dr. Lisa Sanders’s column for The New York Times Magazine is now live.
Dr. Saint Amand, in California, USA, retired now, has pinpointed a solution to reverse the symptoms of Fibromyalgia. He says Chronic Fatigue Syndrome is Fibromyalgia. In his book, “What Your Doctor May NOT Tell You About Fibromyalgia: The Revolutionary Treatment That Can Reverse the Disease,” (by R. Paul St. Amand and Claudia Craig Merek) he goes over everything he’s learned about Fibromyalgia, from 20-30 symptoms, to the Guaifenesin Protocol. Having used the Guaifenesin Protocol myself, I can tell you it absolutely works.
This web site is mostly a walk-by means of for the entire data you needed about this and didn’t know who to ask. Glimpse here, and you’ll undoubtedly uncover it.
I agree with Elizabeth Edwards about the need for large scale research on survivors – there must be many like me who recovered and proper analysis of the circumstances would be helpful. I can only go on my own experience but I had to rely on self-help because it was 30 years ago and the only ideas anyone could come up with at that stage were vitamin supplements and allergy testing!
What has always struck me about the condition is how it confuses everyone, including the sufferer, about whether it is physical or psychological, and in this it challenges that binary opposition. I think I instinctively knew that it was both psychological and physical, and so did everything I could to improve both my mental and physical health, like stopping alcohol, eating super healthy and, to return to the original article topic, I also tried to gradually build up exercise, although this at first was desperately difficult, but I am sure this helped a great deal. In the end I think the most significant thing I did was to give up my job for a year to study full-time for my Master’s degree, which boosted my self-esteem as well as giving me the chance to rest more and increase fitness. I did remain in fear that it would return for many years but happily it has not and I doubt now that it ever will.
The final thing I would add (and why I have not used my real name here) is that thirty years ago I was not aware that in my twenties I was suffering from complex PTSD as a result of childhood sexual abuse, the memory of which I had repressed. The onset on my illness was a classic post-viral scenario but I assume that my underlying mental health problems combined with the chicken pox gave rise to the CFS. I think there was some research on the link between the illness and psycho-sexual problems many years back, and I recall that some people didn’t want to hear about that sort of thing, but I think avoiding such issues is not going to help anyone.
You can share your recovery story, if you’d like to, and read a variety of others’ recovery stories on Cort Johnson’s ‘Health Rising’ blog. There are other sources too, eg a couple of people offering for-profit brain/autonomic nervous system retraining programmes have ‘success stories’ sections (but bear in mind they may be only a handful out of all the people who’ve tried the methods prescribed, without recovering).
IMO, all such stories need to be approached with interest, but caution. There are clearly as many paths that have led to recovery as there are triggers and illness trajectories. We know that what works for one person does little or nothing for another. Some things are moderately helpful for most people, eg dietary adjustments and pacing (not the PACE type, but the normal kind!). Meditation and/or anything that promotes relaxation and/or better sleep (may be different for each individual) can be good. But it’s all very individual.
It can be helpful to hear how others have recovered, just in case something resonates, or they did something we hadn’t thought of yet, but it can equally be depressing for the majority of us who’ve tried most if not all of it, and more, without success. Those more recently diagnosed, who read one person’s success story and think that must be the way to do it, and copy that system assiduously, only to end in disappointment, can become disillusioned quite fast.. so, I’m just saying, not everyone is going to be as thrilled to hear another recovery story as you might suppose.
Sorry if this sounds all too negative. I do agree absolutely that some serious, large scale research/analysis into recovery stories could yield very useful insights.
ive been isolated with chronic fatigue since the 70s. i have ptsd from verbal and emotional abuse. now im alone at home all day and want to break free from it. depression and anxiety and paranoia and being obese don’t help.
Finally! I can’t believe it. With thanks for all those advocates; an active online presence. This explains it it all! A lifetime of embracing life; but wondering why I could never “catch my breath” , if you will. Surrendering to the circumstance in a darkened room; but now, knowing. There is hope! Thank you! Thank you!
Thank you for the article and all the work you’ve done!
To nasty people out there including some who commented here, who insist on blaming patients wholly or partially:
I AM thin. I DON’T have depression. I can prove it.
Check out my Facebook page Robin Brown. And patients, carers and advocates, join my group Dr Hng’s ME/CFS Friends.
That’s right – I’m a doctor. I am the last thing you would call lazy or depressed. Buy my book and see for yourself. You clearly need educating, unless you have already decided, “My mind is made up, don’t confuse me with the truth”.
And the comment about not having sex was nonsense. She stopped because an orgasm caused a relapse? Seriously?
I sympathize with all those who have learned the truth about academia, funded research, and even motivations for medical advancement. But what about personal responsibility? And being accountable for contributing factors like what they are obviously eating? I won’t presume to judge anyone, but the fact is that eating too much, and not exercising will ultimately fatigue anyone. And even though they deny ‘depression’, it seems clear that it is present to a degree. Show me a thin, meditating ‘victim’ of this syndrome.
I am a thin meditating “victim of this disease” with a MS in psychology! Don’t judge what you don’t know anything about!
I have had CFS/ME for over 10 years, it took 4 years + for a diagnosis, complicated by my age and expectations that you naturally slow down as you age, the menopause and a prior history of depression. I had a pretty gung ho attitude to life, have always been physically active and loved the great outdoors and had the expectation that this, along with healthy eating habits would maintain a level of health and fitness as I approached retirement. As I had no secondary source of income and thought relying on the benefit system would probably break me I struggled on reducing my hours to part time, crashed on my days off and had chunks of time off sick. I did attend a specialist CFS/ME clinic, was not the most popular patient because I thought feedback, after I followed their advice, would be welcomed, it wasn’t. Pacing was the most helpful guidance I received from the medical profession, I spent thousands trying alternative routes to health but finally decided that I would do better to work it out for myself. I decided I would stop taking any medication to manage the symptoms so I could rely on my body’s feedback to monitor my activity/rest/diet. This approach has worked moderately successfully, I have a much greater functioning range but have also now given up work and, out of necessity, live the quiet life my continuing symptoms demand. Strangely, the more I improve the less people believe the diagnosis, so I have mostly stopped talking about the limitations it places on me. I do get quite lonely and despondent but feel hugely comforted and supported by people sharing their experiences and the energetic drive to debunk the damaging but medically validated ‘support’ within the health system. Excellent work, thank you.
I am sure that there are many causes of cfs. I myself was admitted to hospital suffering from sepsis 15 years ago. I took early retirement soon afterwards as I could no longer manage to drive to work let alone do a days work when I got there. My doctor was unsympathetic and would not sign me off work. Over the years I have seen various doctors and offered many “treatments”. I too became isolated , luckily my husband and family eventually understood. Over time I became worse to the point where I was almost bedridden. My daughter persuaded me to try one more visit to hospital. I am so glad that I did. He had the answer. I am non celiac gluten intolerant. Somehow my body mechanism must have changed 15 years ago. It could have been the sepsis or all the drugs I was given. Apparently the gluten protein attacks my brain which results in fatigue and eventually ataxia. I do not think that the normal tests for gluten intolerance shows up this problem.
The point in all this is that I am sure there are others like me who have not been diagnosed and also that others possibly have some other autoimmune problem that at the moment has not been recognized.
I agree that one thing that is hard to deal with is that very few people recognize how debilitating it is or even acknowledge it as an illness and it is not just laziness.
Good luck to all those who are still suffering.
Thank you David, this is a great article for all concerned. I was diagnosed with ME/CFS in 1985, I was lucky that my family Dr. had just attended a conference about CFS. It took 3 years to begin to recover, since then I have had numerous relapses of varying degrees. I have been in a severe relapse for 3 years, as bad as the initial onset. I have tried to watch for news & information on ME/CFS every few months, much easier with a pc, than it was at the beginning. But the stigma is still the same, very few freinds or family really understand, including my (new ) Dr.(my original Dr. has retired with ME/CFS) When I brought up the subject of some treatment ideas for ME/CFS, he immediately suggested PACE, I laughed & suggested he look into the study in more detail… If we felt better we would do more, or more often overdo & relapse again.
There are a few things I would like to contribute about my understanding of ME/CFS. It is important to note that some symptoms of ME/CFS can change with each relapse, so it helps to realize this when navigating this dreadful illness. Another issue that complicates this even more, is trying to distinguish When you really Need to see a Dr., is it just more ME/CFS? or can this really be treated with medicine? A very frightening aspect is the possible contagion of ME/CFS. No one who has this would want to pass it on to anyone.
I would like to suggest that David consider another article about all the new discoveries that have been made in the past few years, from seeing it in the brain to the gut bacteria and so on.. I would love to see a well written article that can give hope to sufferers, as well as some validation for the many strange symptoms we all endure. Thank you for being openminded enough to see what ME/CFS can do to those who have it as well as those around them.
As an ex Advance Personal Trainer & Sports Therapist. Enjoying all sports and participating in Triathlons all over the whole of the UK. After bouts of meningitis I went on to being diagnosed with mild ME. I was given GET and pacing by the NHS. I was doing the amount of an unhealthy 80 year old. Still, this wouldn’t put me off as I wanted my health back and was told this is the best treatment. After 6 weeks of keeping it up no matter how Ill I felt, I crashed badly and ended up with severe ME and have not recovered despite 5 years passing. I am stuck in this state, sadly I am not alone, I have heard hundreds of stories telling the simular stories from other adults who had mild ME and now have it severe too because of pacing and GET
When the psychologists took over in the 90’s, I stopped telling people what I had (mecfs since 1984), since most of the time I’m fortunate enough to be able to “pass.” No longer. Your original report on the PACE trial gave me hope. Someone is paying attention! Please keep looking into this.
Been ill for 28 years and had some desperate times despite a loving family. Always amazed at how the press distorts these issues. Look after yourself and please keep going- you offer a glimmer of light . Many thanks
Great article -thank you. As a ME/CFS sufferer who can just work part time, doing a few hours a day. I’m fortunate,but can’t push to do more. As a health professional in Rheumatology I’ve been asked to treat patients with ME/CFS, but taken from this as wouldn’t use recommended treatments of PACE and GET. In the UK we need more journalists to tell the truth and interview patients who are suffering. Please keep writing the real story.
I am late to the comments party but this is important stuff. We suffer tremendously and have almost no allies who understand that medical science has gone this one wrong. Anybody that disagrees with this and tries to help us is fairly easily ignored. Doctors, researchers, the media, and friends and family, not to mention society at large, have long ago made their minds up about this and if we have anyone in our lives willing to see this for what it is, we are fortunate.
So we should understand that David, in joining our fight, has taken a potential risk. We’ve seen this week how the media promotes the other side of the narrative in the UK, often without opportunity to respond, and that the NIH has carefully considered our concerns, and, in hewing to some sort of scientific open-mindedness, has decided that Edward Shorter is an appropriate choice to speak on the history of CFS, at NIH. This is what they think of us, that they would present Esther Crawley as an expert on a disease in which she declares a 2% prevalence based on self-report, without requiring a diagnosis (and the journal she published in wouldn’t even deign to publish a dissenting letter), and Shorter, regardless of what any of us would think about that–heck, even Simon Wessely had protested at Shorter’s first Psychology Today blog about the IOM report.
David deserves more than thanks in taking this on as a project, even if he’s obviously correct that we’re handled in a way that enables shockingly corrupt and harmful ‘science,’ but unfortunately thanks will have to do for now. Hopefully some day he & those others who fight the good fight will see more tangible progress in this fight than we’ve been handed so far.
For me as a professional ballet dancer I knew from the start there was no way to push through this illness.
As a dancer you just develop a certain physical intelligence or intuition about your body and how it should feel.
This was different from the fatigue or the pain I’ve been dealing with on stage. Or even a cold or the flu with fever. Your body just tells you that it’s ok.
But this was different, even when I did it know anything about ME yet.
But I followed doctors orders. Twice. Started CBT and GET. I got very ill for several months.
If I had to do it all over again I would avoid these treatments like the plague.
I might not have gotten as ill as I am now.
Almost ten years ill. With the last years, house and bed bound. In the dark. Living like an involuntary recluse.
There is no cure. No funding in the Netherlands for biomedical research since 2005. Why would you? CBT and GET just work? Right??
Thank you David for this monumental article. Let’s keep banging on that door so the next generations won’t have to deal with this big old lie. And get actual treatment or ideally a cure.
You are a hero. Can’t thank you enough.
Groetjes Anil van der Zee from Amsterdam.
It’s so refreshing to see investigative journalism accurately reflecting the facts. After seeing the UK psychobabble the Science Media Centre organizes for their media to spread, and seeing that their media just regurgitate fallacies, your integrity is a breath of fresh air.
Great article! It’s refreshing to read something written by someone who is on our side, for a change. I want my life back – the life I had before I became ill and turned 24 years old. I’m 53 years old now. ME/CFS has helped me lose just about everything – a brother I adored, a husband I adored, pets I adored, the ability to work and earn a living, etc. But the honest truth is that the less I do, the better I can function.
Thank you, David Tuller, for this extremely well-written article! I’ve been ill with CFS/ME and MCS ever since having a cold in mid-August, 1987. One totally expects to get completely well after a cold, right? I gave at least 20 antidepressants a try; and when none of them made me feel better, it was obvious that something else was causing all of my misery. It took over 12 years and over 12 doctors to finally get correct diagnoses. Even still, the less I do the better I feel. Getting angry about it just makes me more exhausted. I want my life back. I had a very fun, energetic life back in early 1987 before I turned 24 years old. I’m 53 years old now. I’ve lost all my family because of these illnesses, including an extremely intelligent brother who should understand them, but simply doesn’t want to. I lost my husband of 28+ years because of these illnesses. I lost my pets in the divorce, one of the most painful things ever. The established medical community is crazy to say that I just need to keep trying antidepressants. How sane is it to keep trying something over and over again when it doesn’t work?! I’m not crazy! The less I exert myself, the better I feel, and that’s the truth.
First I’d like to thank David Tuller for his continued commitment to shine a light on the disservices committed against this very sick community of 1-2.5 million Americans and 14 million worldwide. I also greatly appreciate Nita sharing her personal story.
Next may I please reply to the comment above posted by “Jane”. I’m not sure if you just slipped up in your comment by using the term chronic fatigue, or by suggesting that any treatment focused on fatigue is an answer to this disease, ME/CFS. Chronic fatigue is a symptom of many illnesses, while ME/CFS is much, much more. If I misunderstand your meaning then please forgive me, but it is so important a clarification and warrants a response so that others who read your comment who are not familiar with this disease will not use the term chronic fatigue
interchangeably with ME/CFS.
Finally I would like to just reiterate that ME/CFS has an annual economic burden of $17-$24 billion american dollars per year. Patients are at a much higher risk of dying from heart disease , cancer and suicide than the healthy population and at a much younger age (37.8% to Cancer; 19% to Heart Disease; 19% to Suicide). Those who commit suicide t do the most severe house/bed bound and do so out of desperation and loss of hope for any improvement.
The $6 million dollars in annual research money granted by the NIH is a pittance especially compared to other diseases with similar levels of debility and which affect far fewer patients.
Thank you for a great article in general and especially for bringing up mold in it. There now are large numbers of well-vetted, classic ME/CFS patients who are reporting substantial improvements in their conditions from careful avoidance of environmental mold toxins, and so I am hoping that more systematic studies will be done looking at this factor in the near future.
Approximately 17 Million PWME global wide held prisoner and sentenced to ME purgatory by a bunch of Psychiatrists for close to 50 yrs. Highest causes of death: 37.8% to Cancer; 19% to Heart Disease; 19% to Suicide.
Those who committed suicide did not do so because of depression. They did so out of desperation.
http://www.name-us.org/ResearchPages/ResearchArticlesAbstracts/JasonArticles/Jason2005Mortalityfull.pdf
An excellent piece that took hold of me straight away …so I read it without pause which was using up a spoon too many but one has to break out occasionally even with this monster of a disease. I was thinking that instead of MR Shorter summarising his psychiatric version of the history of ME to NIH staff…may be someone could read this to them instead…..far more worthwhile and certainly this has truth, realism and indicates exactly why biomedical research study funding is needed now.
Thank you so much, David!
It is TIME (!!) for The Mayo Clinic to stop prescribing GET to their patients and openly acknowledge they have moved on from such antiquated treatment modalities. Just last year, I came very close to putting 18k on a credit card at their insistence it would benefit me. It would have cost us another 8k for travel and hotel for the month. I am particularly offended by their ignorance and cavalier attitude about this because most of us are unemployed. Thanks to the piece you wrote last year on this subject, David, I am beyond grateful to have been saved the expense, and more than likely, symptom progression, by not falling for this as a legitimate treatment. GET with the program, MAYO!!!
David, Is there a way that you could put me in touch with Nina? I live in her area and have a doctor who has done wonders for my fatigue, and I would love to share the information with her. Contact me via my email address and put “Nina – Chronic fatigue in the subject line. Thank you, Jane
Where are the objective physiological markers? The ICC and the CCC document easily measurable abnormal physiological responses to exercise/exertion. So why aren’t we all measuring them? Heart rate monitors help with pacing and stayimg under our anaerobic threshold is recommended so why aren’t we gathering evidence on this, it seems to be helping peole?
Workwell found we have a low anaerobic threshold so this disese is not invisible !!
How can we get patient power showing that something is wrong?
It’s not normal to have a heart rate of 140 just getting out of bed….it doesn’t matter what you think the cause is show us how o get better???
We know that our HR is elevated at rest after exertion this isn’t normal so why isn’t it being investigated??
Seems to me the the CCC and ICC are full of gems of ideas that could be used to good effect.
Measuring your heart rate doesn’t need to men’s doing any exercise as the abnormalities show up for many in day to day life!!!
PACE trial participants found that as they worsened their true morning resting heart rate deteriorated.
On person said that the PACE response that’s not normal, that shouldn’t be happening, you better stop recording your heart rate.
Telling someone to stop recording their deterioration doesn’t make the deterioristio stop.
David does a tremendous job here exposing a treatment that has harmed many thousands of patients. If graded exercise were a drug, and the PACE study funded by drug companies, the scandal would be enormous. But, this involves a long-stigmatized, misunderstood, understudied illness, so the rest of the world is slow to take notice. There are more threads here waiting to be pulled by enterprising reporters. Look at David’s line about how the proponents of the PACE trial consulted for insurance companies and the British welfare department. Follow the money and it points to bad science being foisted on patients to save insurers from having to pay claims. Disability insurance companies, to this day, pretend they don’t know what ME/CFS really is or how damaging it can be.
Strange how so many others have turned away (family, friends) or, sadists all, have willfully abused us with their science. But David Tuller stepped in to help. You, David Tuller, are a wonder. If I was well enough to cry, I would at this moment cry in gratitude.
Outstanding article David, as always.
Thank you David for your tenacity in reporting on all that is wrong with GET for ME and the PACE trial.
Should anybody read this far in the comments, please take a look at the stopget.org website. This site provides background to the use of GET as a ‘treatment’ for ME sufferers, a current trial of GET on children (the MAGENTA trial) and links to two petitions for those who wish to register their support for the call to stop all trials of graded exercise therapy for ME. Thank you to anybody who does sign these.
Thanks for your great work and interest, David Tuller. It is much appreciated and hopefully read by many. A great easy read on this mess, summing up the grim history of this disease and illustrating the immense strength of patients. It is absolutely insane thinking of the worldwide harm done by the “Weasley-school” and PACE, without medicine itself asking the relevant contradicting questions they often do in the name of good science. The effect has been devastating on patients and society.
The conference in Florida past days really give hope for further progress. Time is urgent. People have lost years and years. It is totally absurd to experience the enourmous gap between the oversold nonsense-models from U.K. that have hurt so many for decades, and the things we actually do know. Thank god for the curious and rigorous physicians that keep up the important work without substantial funding. That is really impressive.
Thank you David Tuller! Must be really difficult to look at ME-sufferers and say: Sorry, I was wrong. I made you suffer more than I helped you, even when I saw my mistakes made you cry. So much easier to say: It’s all in your head/mind, please continue. ME made me understand what I never expected to learn about doctors I met when I asked for help and trusted them. ME also teached me why I never should treat someone like they did. Always remember the truth is more powerful. Sometimes too powerful I guess.
Thank you for everything! Best wishes from Norway
Thank you David Tuller for writing about how it really is,
Thank you so very much, Dr. Tuller for all your work on this vital topic! And, thank you for continuing to point out that institutions are slow to change gears now that the Oxford diagnostic criteria, GET and CBT as cures/valid treatments for ME have been discredited. More patients and the medical profession must be made aware of this. Your writing will certainly assist with this!
The Canadian government needs to listen to what you, and biomedical scientists are saying about ME. The Canadian Institutes of Health Research stands by a recent grant application review and denial, that said there is no evidence CFS is a disease, and that it is pointless to hunt for biomarkers. It appears our Health Ministry believes this as fact.
Belief systems are harder to move than mountains. Thank you Dr. Tuller for your concerted efforts and success in moving erroneous ME belief systems.
Dr. Tuller, thank you so much for another fantastic article. You are one of the few healthy people who seems to truly understand how this disease feels to sufferers, especially the core symptom of post-exertional loss of function.
I’ve been sick with ME since 1994 and largely bedbound since 2005. I can walk fewer than 40 steps per day and can no longer walk to the bathroom; I have to be pushed in my wheelchair or use a bedside commode. I’m so weak that I have to bathe and brush my teeth here in my bed.
For me, a forced program of graded exercise would be a disaster, causing me to lose even more of my abilities. This letter to the IOM committee, signed by nine severely ill ME patients, explains the adverse effects of forced activity:
http://paradigmchange.me/wp/severe/
I deeply appreciate your work that shines a bright light on the harmful “therapy” GET.
Investigative journalists play an important role in uncovering unethical practices. An example: Cardinal Law of Boston didn’t resign until the Boston Globe’s Spotlight team published hundreds of articles exposing Catholic priests’ sexual abuse of children and the Catholic Church’s subsequent coverup of these crimes.
Sadly, practitioners of GET, the PACE authors and their defenders are now digging in, refusing to admit any wrongdoing, much like the Catholic Church.
If you keep publishing these articles, the public will eventually recognize GET and those who defend it as frauds.
I agree with Rebecca that it would be helpful to have this indepth level of reporting applied to those people who have recovered from ME or who, like me, achieve a better standard of health than many by continuing to do gentle exercise. People like Rebecca and I are excluded from the debate about ME. I can assure you I have all the symptoms of an ME sufferer but have finally managed to stop my slide down the hill and start the long climb back up. Our stories could hold part of the answer to how to cure ME.
Thank you for this, and for the excellent interview on your podcast. I have been living with this disease for five years, and it is hell. I am currently functioning at 2-3 (1 being bedridden, 10 perfect health), the worst I’ve ever been due to my very Type A insistence on pushing myself. The doctors and psychiatrists who were treating me always applauded my commitment to staying active while disregarding my steady deterioration. Needless to say, I don’t see any of them anymore.
That said, I’ve become a big believer in gentle conditioning within my energy envelope. VERY gentle. I am benefiting from breath work, careful stretching, and subtle, mindful movement to retain some core strength and maintain healthy posture. I do this under the supervision of a Pilates instructor who comes to the house and never, ever pushes me. We stop when I say so.
GET was a disaster, rightfully discredited. But I wonder if we pitched the baby with the bath water? Deconditioning really is a problem. Some—maybe most—of us could benefit from PT. It just has to be the right kind.
Many thanks. Hard to read as it resonates so much.
” She doesn’t watch TV— trying to keep up with the plotlines is “too stimulating,” she says”.
Watching things I’d like to watch (breaking bad, …) often is far too draining to the point that it can cause fatigue in the next days.
E. Reinhold, please take a look at the emerging theories and research that was presented last week at a conference for ME/CFS:
http://iacfsme.org/ME-CFS-Primer-Education/News/IACFSME-2016-Program.aspx
You can perform a search for the words “mitochondria” or “POTS” or “mast cell” and find relevant information.
Also to add that in the UK its a very scary place to be a sufferer. I avoid Drs at almost all costs. One fears that refusing CBT GET may result in being sectioned (ie taken to a psychiatric institution against one’s will & declared mentally incompetent to make one’s own decisions) in order to be forced into doing CBT/GET.
That fear, although it *sounds* paranoid, is unfortunately well founded (eg poor Sophia Mirza who died from ME as a result of such an event, & Ean Proctor – a child removed from his parents & taken to a psychiatric unit where he was taken out of his wheelchair & put in the deep end of the swimming pool in order to ‘prove’ to him that he wasnt paralyzed by severe ME – whereupon he sank like a stone & almost drowned – if you’re incredulous google it. And so many others…. Karina Hanson, ugh the list is long & horrific. )
Thank you so so much for writing this article David & huge thanks to Nita & Doug also.
it’s medical arrogance gone mad, coupled with people in power who accept whatever they are told as long as it confirms their own prejudices.
The agony of being told that the reason you have lost your independence, the ability to leave your house, your career, friends, pretty much everything, & are suffering immeasurably every moment, is because you are not trying hard enough to do the very thing that YOU know from long experience is what makes you ill in the first place, cannot be underestimated. It is an unspeakable cruelty to be told, having been made ill by a ‘treatment’ recommended by your doctor, that you are iller because you must want to be. It’s Kafkaesque.
How spectacularly condescending it is to be told (at 35) that you cannot tell the difference between the physical sensations of having done more exercise than one is used to, and the sensations of being ill.
It is a classic example of gaslighting…. – when patients are given psychological therapy to systematically remove their faith in their own reality, & get them to disbelieve their own experiences. Convincing them to DO more & more of the one thing that their experiences tell them will harm them (more exercise). And then when that gaslighting is successful & they DO get worse, going from housebound to bedbound (or worse) as a result, they are told it’s because they must have some unconscious desire/need to stay disabled, or they simpy didnt try hard enough (to do the thing that makes them worse). And that experience damages more than one’s physical health, it damages one’s mental health as well. It abuse, pure and simple. That may not be the intent, but it is the result. Iatrogenic harm at it’s most insidious.
And all because a group of psychiatrists have a theory and are unable to acknowledge to themselves the possibility that they might be mistaken. The reason patients get worse after GET couldnt possibly be because those psychs are wrong could it?! i mean what a suggestion!… such a notion is unthinkable! It cant POSSIBLY be that because they are infallible….. therefore it MUST be some flaw or fault in the patients. I’m sure thats why they feel no shame in having ‘doctored’ the figures in PACE, I dont doubt that they believe their slight of hand was for patient’s benefit.
It is hubris on an epic scale. And millions of lives, including the abject & intolerable suffering of children, are all being sacrificed at the altar of their egos. It makes me sick. Literally.
I thank God regularly for people like you David, it is only quality investigative journalism that will reveal this scandal to the world.
Thank you so much for this. My M.E. Started with mononucleosis when I was 17. Graded Exercise Therapy was the worst thing I could have done – I ended up in a wheelchair and went from ‘mildly affected’ to ‘moderate’.
I became pregnant and was concerned about the exertion involved in labour. I fought for a managed labour, and was also (eventually) given the option of an elective c-section. I still don’t know if I made the right choice. I suspect not. Labour pushed me over from ‘moderate’ to ‘severe’.
I’m in the UK, and it’s a terrifying place to have ME. I’ve been in the emergency room a couple of times, and I never know if saying ‘I have severe ME’ is going to signal to that person that my health is very fragile, or if they’re going to assume ‘deluded malingerer’. You just don’t want to be in that position when you’ve just been in an emergency ambulance and you’re unsure whether you will live or die.
Very many thanks for your excellent article and for all you have done bringing this scandal out into the public domain after so many years. I have been mainly bedbound 20 years with ME and at long last there is hope of change and recognition.
If only the blinkered UK medical establishment who feed the British media, and NICE guidelines who haven’t seen the need to look at ‘foreign’ research so do not plan to review them till next year, would take note!
Thanks for the excellent summary. If you are affiliated with Kaiser HMO, can you lobby with them to develop a comprehensive program for ME/CFS since they have millions of patients in California etc, and seeing 5 doctors to get diagnosed in <6 months instead of 30 over years, and helping people cope with M.E., instead of having ER visits, would save them money, improve patient care, and show they are a leader for others to follow, instead of waiting for CDC then Mayo to put out correct information. California has been a leader incl for AIDS, why not M.E.! We have proclamations for ME awareness from San Francisco CA, Los Angeles, Sacramento, other cities, & are striving to get State proclamation for CA and other states, and perhaps next US president, then I think having public officials aware, school boards aware etc will lead to much more funding for M.E. in 2017.
See for example MEPedia where we are trying to display any proclamations, and hope you can add any you might have in your city, state, province, country for the world to see who cares about M.E.
http://me-pedia.org/wiki/United_States_proclamations
I like the Los Angeles proclamation if you want a template, but must customize for your city and give letter for your story.
This is such an important topic! So much stigma and unnecessary suffering has been caused by the PACE school in the UK. Here in the US, the 30+ years of neglect and disdain from CDC and NIH for PwME has done the same. Thank you for shedding light on the long and sordid history of this disease. Keep up the good work.
this is the financial run-around, not(run down).
Here is the financial run around.
I’m so grateful to David Tuller for giving voice to so many of us who are weak to speak for ourselves.
Another accurate and comprehensive article. Thanks again David Tuller.
Good read, lots of info, thank you! Mr. Tuller
Sincere thanks for your amazing work. I truly hope the medieval mindset that is PACE, and all those implicated with it, will finally be seen and accepted by all for the enormous crime that I believe it is. Your unfailing efforts will help tremendously in that I feel, and help stop it fading from public view, as the establishment so desperately want it to. Please to keep up the very good work.
Thanks so much for this riveting article. Intertwining the reality of the personal lives of Doug and Nita with the far reaching and damaging facts of the Pace trial is nothing short of brilliant.
Excellent article by David Tuller, gets straight to the heart of the abuses faced by people with ME from the medical establishment. Surely it is now plain to see that significant funding of bio research is the only way forward.
Thank you David teller for standing up against bad/fraudulent science. The truth will be uncovered sooner thanks to you. How has pace not been retracted yet?????
Thank you David, for such a well-researched and argued article. As a ME/CFS sufferer whose health was severely damaged by graded exercise, it is time that the pseudoscientists responsible for this junk science are held accountable.
Beautifully written, David – we are so grateful for you unrelenting advocacy!
Where to begin? Thank you for interviewing my cousin, Niita. I also have been treated with physical therapy and became worse over the last 30 years. Thankfully my husband can cook, clean, and do lsundry. However he doesn’t completely get it. My kids do not get it.
Thank you for all your work.
I was one also to be recommended agressive rehab by a physio who was paid by the disability insurance company. Thankfully I knew better than to fall for that. See, I had just started getting chest pain and shortness of breath, on top of orthostatic intolerance. So I held my grounds. Instead, the insurance company sent an occupational therapist to help me ‘setting goals and get motivated’. She wanted me to go walk every day at the same time. I was provided with a booklet that looked like CBT. And when I told the occupational therapist I was getting short of breath and my muscles stopped working halfway around the block (I was walking very slowly) she gave up and wrote in her report I was too focused on my symptoms (therefore my fault).
i have been sick for 8 full years this next week, and terribly traumatized by the lack of appropriate health care received. In my country (Canada).
Thank you to David Tuller for speaking up. There are millions around the world missing from their life, without competent care.
I am laying here in my bed with tears streaming down my cheeks because I know these patients, and David, you could not have picked a better person than Nita to highlight as a long term ME/CFS patient, who in my experience is a shining example that we are NOT depressed, unmotivated or have given up! WE ARE SEVERELY ILL AND WE HAVE BEEN AND CONTINUE TO BE ABUSED.
Personally, I have been ill for 24 years and the last ten ended up in the severe category like Nita because I “drank the Kool-Aid” and believed I could, through sheer will and determination, push myself and show this disease who the boss was. Ha! I learned that my body is the boss and with ME/CFS it can be a brutal task master if I do not listen to it.
It is comforting, in a way, each time a new study rolls out showing proof that ME/CFS is a physiological disease that reaches to the very core of every cell in our bodies. Further solid research and a public outcry over the cheating, lies and damage the PACE trial has wrought upon our patient community are sometimes the only light we see at the end of our tiny tunneled lives . The truth train feels like it’s finally going in the right direction and it’s speed is increasing
I so look forward to the day when that PACE trial will come tumbling down publicly. Thank you for continuing to use your talent of investigative journalism to act as part of the wrecking ball that will fully expose and demolish the already fractured study and liberate those of us who have been imprisoned behind the walls it’s misrepresentations built.
Thank you so very much for your invaluable commitment, insight, and courage, as well as your skill and dedication to writing so well about all of this. And thank you for your persistence in spite of the risks and other downside that come with being so outspoken and insistent about getting the truth out, loud and clear! We all deeply appreciate everything you have done and continue to do. Thank you so much for this extraordinary article.
Thank you so much for covering this story! I am one of those patients who have been rendered permanently bedridden by doctors forcing “exercise” on me. It’s the worst recommendation you could give someone with ME.
I’ve had ME since early childhood and tried exercise until a couple of years ago. It has always made me worse, as has being active in general. All this time, doctors and people who knew me thought I was “deconditioned” or lacked motivation. This has been very hard, because keeping up activity has made me worse permanently. My experiences in society: health care, school, work, relationships, have given me PTSD because of the demands to “act like normal”.
It’s an absolute delight to see David Tuller write about my experiences and validating them. Currently, the IACFSME conference gives me much hope as well, as they are talking about my symptoms. Not my beliefs or background or motivation, but post exertional malaise, brainfog, orthostatic intolerance, muscle and joint pain. I don’t want to think about the biopsychosocial view anymore, but unfortunately, I am confronted with it every day. Thank you very much for your efforts to change this.
Neglect fueled by intellectual sloth and complacency has caused enormous suffering to people with ME. Many thanks to David Tuller for all his work documenting this.
Fantastic article, David! The PACE study made me believe I should get up and exercise and now I am almost completely housebound and have to spend the majority of my time in bed. What mystifies me is how Peter White’s own research prior to PACE found that inflammatory cytokines were present in ME sufferers blood for a prolonged period after exercise *(ref: JCFS 2004:12 (2):51-66). This would account for Post Exertional Malaise that is a prerequisite for an diagnosis of ME. Why did the PACE team not tell the trial participants about these findings and the potential harms of exercise? Why did the PACE team fail to record cytokine level data during the PACE trial? And why would they think Graded Exercise Therapy (GET) is any sort of treatment considering this objective biomedical evidence?
Simon Wessely, Peter White, Michael Sharpe, Trudie Chalder, Esther Crawley….These are the names that should never be involved in ME research ever again. These people ignore science in favour of their own entrenched and disproved beliefs, which are heavily biased because of their associations with disability insurance agencies and the UK’s Department of Work and Pensions.
*Margaret Williams’ ‘Proof Postive-Revisited’ 26th September 2016. Highly recommended reading, available by a simple web search.
Thank you. I am very grateful to you for your selfless work in such a thankless, neglected and little-did-I-know intentionally deceptive medical area. I went from a healthy happy fully functional 34 year old woman to a severely ill person in just a few months back in 1994-5 and have struggled with ME/CFS for the past 22 years. I wish you all the very best in your work and hope that you will be recognized for your dedication and determination in executing such thorough reporting and writing. Your work is a beacon for those of us who have this illness. God bless you.
Thank you David for fighting for us. I hope some kind of Humanitarian award is given to you now or in future.
Thank you again Dr. Tuller!
“In the 30 years since, federal researchers have failed to identify any causes, diagnostic markers, or drug treatments — an impressive trifecta of non-accomplishment.” How true!
Dr. Rowe put it well
““The assumption that deconditioning is the cause of all symptoms ignores the potential contribution of other unrecognized biomedical problems (and ignores much of the research produced in the last 20-plus years),” he added.”
Healthcare professionals (and laypeople) need to have (more) open minds about things they can’t easily explain.
An earlier commenter aptly noted – if healthcare professionals would listen to patients/caregivers we would be much further along in diagnosing people accurately, and treating them appropriately.
I’d like to add my heartfelt thanks to you, David, for your unwavering, persistent commitment to exposing this nightmare situation. Given these awful circumstances for pwME over the decades, US ME/CFS clinician Dr Nancy Klimas’s findings sadly come as no surprise:
Dr. Nancy Klimas also said in an interview in the Miamy Herald 2009:
“I’ve had patients who met posttraumatic stress disorder criteria, where their trauma was their interaction with their physician around this illness. They came to a doctor with Chronic Fatigue Syndrome; they left the doctor with PTSD.”
http://livetsbilder.blogspot.co.uk/2016/10/the-most-extreme-consequence-trauma-and.html?m=1
David, thank you for this historical and personal article and, of course, your advocacy in helping M.E. patients. I never use any other term. It was what I was diagnosed with in 1987 by a specialist and again in 2011 by another M.E. expert, one of the 26 M.E. experts who compiled the 2011 ICC for M.E.
In that ICC for M.E. (http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2796.2011.02428.x/full), these M.E. experts state:
“The label ‘chronic fatigue syndrome’ (CFS) has persisted for many years because of the lack of knowledge of the aetiological agents and the disease process. In view of more recent research and clinical experience that strongly point to widespread inflammation and multisystemic neuropathology, it is more appropriate and correct to use the term ‘myalgic encephalomyelitis’ (ME) because it indicates an underlying pathophysiology. It is also consistent with the neurological classification of ME in the World Health Organization’s International Classification of Diseases (ICD G93.3).”
I would like to add that inflammation was found in autopsies of Sophia Mirza and Casey Fero so the experts are correct in stating that M.E. is the more correct name.
So many people thought I was a conspiracy theorist when I used to tell them what has been happening in the field of M.E. and CFS. Your work has shown that the world that fact can indeed be stranger than fiction. Besides the very serious harm those psychs have caused, they have also prevented decades of proper biomedical research.
Although the ’cause’ of M.E. may not yet been discovered, I always wonder why this is mentioned in most articles. I don’t think the causes of lots of illnesses and diseases are known. Yet it’s not mentioned with regard to them. Maybe it’s because they have a biomarker?
If I may mention the Irish perspective please? The Republic of Ireland is a small country but that doesn’t affect the proportion of patients with M.E. here. As a rule, not much research is done here in Ireland and none at all has been done on M.E. So, our Health Service Executive (HSE) takes its information from elsewhere. In the case of M.E., it took its information from the NHS in the U.K. So our HSE website has the PACE guidelines on it.
Back in January of this year, a neurologist said to me: “The only thing I know about M.E. is Graded Exercise Therapy”.
When I contacted the HSE regarding this, I was told that they “assumed the information from the NHS was correct”. Although I have sent them the correct information and proof of the discredited PACE trial, including your excellent Trial By Error trilogy etc., they are in the process now of ‘verifying’ this. So, the proof has been literally handed to them and they are trying to verify it but they did not try to verify the nonsense that they copied from the NHS website. They ‘assumed’ it to be correct.
My point is: what is done in other countries affects M.E. patients here (and elsewhere). Yet we seem to be largely ignored and rarely supported. Back when I was first diagnosed, and actually up until quite recently, my illness was referred to as M.E. It is only in the latter few years that it has been called CFS.
I totally agree that the likes of the Oxford criteria is a sham. In fact, most talk of fatigue is enough to drive me mad. In my opinion, it is the least of our worries. We are thoroughly exhausted but rarely mention it.
Suffering from transient paralysis, temporary total paralysis, constant and never-ending weakness, Orthostatic Intolerance/POTS, horrific nausea, severe pain, cognitive impairment, etc. etc. etc. all make ‘fatigue’ pale into almost nothingness. If a patient is bedridden 95% and housebound 99% of the time, I don’t think fatigue is the problem (or main problem). So, to me, it’s time that that word took a backstage and certainly should not be a defining symptom in research into M.E.
Sorry for the long comment and my sincerest thanks for all you have done.
Thank you David for telling it as it is!!!!
I went from mild ME to severe because of Graded Exercise and PACE. As an ex Advance Personal Trainer who competed in triathlons over the UK, I was naive when ME struck after bouts of viral meningitis. So was pleased I could start getting fit again. An ill 80 year old could have done more, but I had to keep it up daily no matter how ill I felt. This caused a massive relapse that led me to be bedbound for several years. Now mainly housebound years later. I’ve got to know thousands who had the same reaction and now have their life totally ruined by this damned disabling illness.
Thank you for bringing the truth to light.
Your writing will form into a book on the definitive history of ME. All we need now is one more chapter with a happy ending – a curing treatment and discredit to medics who have prescribed the wrong treatment on no evidence base for decades. It won’t be enough to say that it was the best evidence at the time. There never was any evidence at all. I fear your book may have more than one chapter until we reach the happy ending. Thank you for your insight and clarity.
Thank you David Tuller for a brilliant article.
As an ME sufferer for 27 years in the UK I have had no specialist input, and have primary care doctors who are completely ignorant about ME and use the NICE guidelines to suggest I should try to exercise more. They have showed no interest in learning more about ME, in fact I have in writing from one of them that it is not their job to learn about ‘rare’ conditions, so I’ve given up asking. In a way I don’t blame them – if they are told ME is an MUS (medically unexplained symptoms) and that this means it’s psychosomatic, why would they see the point of looking further.
I am deeply depressed by the stranglehold the psychiatric biopsychosocial model has over the whole British medical and political establishment. It horrifies me how the perpetrators of such non-science can get away with it – with the collusion of politicians because it suits them to dismiss us as unworthy of medical or financial support.
I feel helpless in the face of such medical negligence and malpractice that should have resulted in the perpetrators being struck off, but instead has showered them with professorships, prizes and honours including a knighthood. This is corruption on a grand scale.
I am so grateful for David Tuller’s efforts that will, I hope, one day, help to expose this gross injustice to severely suffering people around the world.
Probably the best article I have ever seen on the illness. One point that may seem too obvious to mention to patients, but unclear to observers is what the medical insurance industry (and in Europe the state healthcare providers) have to gain from the Wessely/Oxford school model. The answer is to check your policies. Many insurance policies have a specific exclusion clause for ‘mental’ illnesses. So the underwriters have a vested interest in lumping as many conditions as possible into the ‘mental illness’ category – and in fact in the whole concept of ‘mental illness’ as an illness with no physical cause. The same applies to a lesser extent to various national welfare systems, which can use the idea that illnesses designated as ‘mental’ are treatable by talking and willpower to minimise payouts to patients who appear uncoopeative. The global insurance industry stands to take a huge hit if it were ever forced to pay out on these and other currently inexplicable conditions. Expect them to fight hard and long.
All, sadly, very true.
“A new report from the Centre for Welfare Reform explains how a current scientific controversy relates to the debate surrounding welfare reform and cuts to disability benefits.”
http://www.centreforwelfarereform.org/news/misleading-mability-cuts/00270.html
David, thank you for your persistence in bringing this important story to light. I was a regular swimmer and scuba diver when I fell ill in my late twenties. I tried to remain active even after getting sick because that was my nature, I was always active and slim, but not know. Although activity worked for me during some of my remission periods, more often it initiated downward spiral both cognitive and physical. Gentle walks in the pool might follow with difficulties finding my way home. Pushing at low levels day after day is sometimes doable for me after 31 years of trying to redefine my life with this illness but it is very easy to trigger problems with connective tissues that now do show up on MRI’s or visible to the naked eye. For 31 years I have had to find PT practitioners willing to try and help with almost no help from the medical community that readily reports, there is no cure, there is no treatment. I find myself as one of the lucky ones, so many of the other patients are not able to go for a slow walk in the pool, or have funds to beg alternative practitioners to try something different. One of the cruelest aspects of this illness, is the irony. When a day comes when a patient feels a little better and tries to push, chances are they in their delight of having a sense of a little energy they will over do, crash, and then be criticized for not trying enough. The best thing a family or friend can do is to know a person with ME/CFS is more likely to do more that they should, than not. I am grateful for my friends and family, who allow me to reach for some semblance of living a life and then understand when I go quiet and disappear to rest and heal. I am only able to function when I am able to recognize my inner body signals that it is time to stop or shift, and respect my bodies self imposed limits.
Thank you David!
I fortunately have much more health than I did in the early years but still think the trend is downhill because it’s largely due to avoiding gluten and mold, and being careful about other aspects of my diet and sleep. That I have the level of health I have. I hate the term “extreme avoidance” because that intimates some type of diligence on my part. I am lucky enough to have the resources to be able to move out into the desert have a large metal building erected and than put another building inside of that where I can control issues with mold growth. I don’t waste any time or resources on “decon” or “extreme avoidance”. Compared to where I was 20 years ago living in a moldy house in florida I would consider myself cured. But I am but a shell of what I used to be before I got sick at 37. I get up, try not to nap during the day or I end up with sleep issues at night. My goal is to do as much light work around my place as possible. My cognitive ability is very limited especially in situations where there is stress. I can spend a large amount of time in front of my computer reading science articles are cfs related subjects. I have in the past crashed so bad from pushing myself with physical activity that I couldn’t sit up in bed without extreme dizziness. lately I have been able to get away with much more activity. I consider myself very lucky for this but when I see what normal people have I still get angry. I want a real diagnosis, not a bogus one that imply’s I’m somehow doing this to myself. I believe if authorities researched the issue of water damaged buildings and cfs they would find more than a correlation, they would find a connection that can be reproduced or demonstrated in a way that can not be denied. Which should eliminate any doubt at least some percentage of cfs suffer’s the condition is real. And we deserve the same respect that would be shown to anyone with any other kind of illness that limits their abilities.
Can’t thank you enough for your outstanding work on this issue, Mr Tuller, and anybody who has helped you. It has been critical in getting the rest of the world to pay more attention to what is really happening here.
This is what real journalism looks like.
“Despite its prominence, no one appears willing to defend it directly.”
This is getting truly absurd. Some are still willing to weakly defend PACE, but only by side-stepping the specific issues raised by the trial’s critics. No-one seems willing to support the trial in any real debate with the many informed critics who have taken the time to detail its flaws.
So many of those in medical research who should be speaking out on this issue instead seem committed to looking the other way and hoping that this embarrassing scandal will pass without affecting them or their colleagues. PACE raises important issues with problems in medical research that go well beyond ME/CFS, and do pose a threat to the careers of many researchers who have been getting away with worryingly low standards for their work. Particularly in the UK, it seems that PACE is seen as too big to fail, and that too many have already committed to the prejudiced dismissal of patient’s concerns. To now acknowledge that they had got this wrong would be a humiliating climb-down. After Richard Horton’s angry disparaging of those patients who dared criticise the Lancet’s PACE trial papers, he has placed himself in a situation where he cannot afford to recognise the problems with these publications.
Much of the UK medical Establishment seems to have adopted a bunker mentality on this issue. It is possible that they will still get away with it, regardless of the harm it does to patients.
“bunker mentality” really sums it up. The recent reply from NICE to an FOI request beggars belief, it is truly horrifying:
In internal correspondence released this month under the Freedom of Information Act (FoI), the agency admitted that it has not yet considered the results of important US studies when deciding what is best for British M.E. patients……
……Professor Mark Baker wrote: “We would take seriously the views of the relevant esteemed medical associations in the UK, principally the RCP (Royal College of Physicians) and the RCPsych,(Royal College of Psychiatrists) when looking at reviewing this guidance.
“I am not aware of any reason to do anything before then unless some major new evidence on treatment emerges, and we know that no major studies are in progress”.
http://www.meassociation.org.uk/2016/10/nice-takes-a-dim-view-of-foreign-work-on-mecfs-robin-ellis-freedom-of-information-request-24-october-2016/#comment-6455
NICE have, shamefully, put their fingers in their ears and their heads in the sand, despite the last recent years seeing the groundbreaking IOM report, wonderful Invest in ME international conferences, Prof. Ron Davies and Bob Naviaux’s work, and numerous other fantastic biomedical research yielding undeniable evidence.
I have had ME/CFS three times. I have recovered each time. The last time, the radiologist read my SPECT scan as early Alzheimer’s Disease and had severe memory issues at the same time. Having abnormal SPECT scan occurs in 70+% of ME patients — Dr. Daniel Amen has scanned many CFS patients with similar results in all of them.
I’m recovered. Working as a Senior Software Engineer in Seattle. Memory is recovered.
The model that is consistent with all of the research is that ME is a persistent severe shift of the microbiome (i.e. gut bacteria) which can result in Lactic acidosis, mal-absorption, virus reactivation, etc. Fetal transplants will often result in immediate remission (that will persist for months) of ME, which implies that it is the microbiome causing almost all of the symptoms. Unfortunately, such transplants are hit and miss for persisting.
There have been recent studies that found that some symptoms matches specific bacteria shifts.
As a biostatistician, let me just say that I’m shocked at how badly Lancet dropped the ball on this one. I normally have great respect for their peer review process, and hope they address this exception to it soon.
Great article, masterfully telling so many aspects of CFS! David, you continue to rock it!
This article illustrates perfectly the challenge of patient-centered healthcare. If our doctors would listen to us when we report what happens after activity, and if policy makers and medical educators listened to us, then we would advance much faster. Our experiences are important data points, and these can inform research, healthcare and education to the benefit of all. But the “medical establishment” has to be willing to listen and learn from us.
Magisterial work to weave in these stories with the broad story of the disease Myalgic Encephalomyelitis since the CDC and NIH’s wrong turn in the eighties. It was a wrong turn “accidentally on purpose” because as Stephen Straus, a chief scientist, at NIH told Tom Hennessy, now deceased, studying this group chronically ill people was unexiting, “I want to study AIDs–a real disease” (this is from memory so not word for word)
However bad the disbelief from many in medicine, and many friends, and even family, is I want to make a point the disease IS worse. Much worse. If I could choose to be well tomorrow but have them still, all, disbelieve me, I’d do it in a second! And I think many others too.
What we need desperately is treatments, and a cure for our disease. But a cure, most likely, won’t happen without a large research effort (using a homogenous definition like the ICC). And that, most likely, won’t come without a complete change in attitude from NIH, CDC, and indeed Congress.
So in the meantime we have to demand respect for the disease, for the facts. We need social support for the many many patients who, like Nita, also can’t care for themselves and have No One to help. I would note this lack of social support is in part a moral consequence of the flashy, incessant marketing (and uncritical acceptance) of PACE and the biopyschosocial approach.
Respect for a disease is a means to get what is even more necessary: effectual treatment, a cure, and, until then, greater social supports. Additionally I believe respect means listening to patients who have entered a remission: was it by a random chance? was it the result of avoiding a toxin? these scientific questions Can be asked, and certainly they can be answered!
However it should go without saying that scientists and doctors should have respect for facts and have an awareness of the biases which might exert influence of them–for example the desire of the insurance industry to get as much as possible reclassified as a behavioral disorder, and the inevitable frustration in dealing with a chronically ill patient for whom there is little more to offer than supportive care.
Such an important article. Please cover this topic more!
Very difficult for ME/CFS patients to read this without getting teary – because we have lived it. Lived the ignorant and damaging GET treatment, the stigma, the loss, the void.
I conscientiously and diligently did GET in 2005 and it cost me my ability to work. I have never recovered that loss of function, and in fact continued to decline after ceasing, until by 2009 I was bedridden.
If nothing else, the ME/CFS debacle has highlighted all that is amiss with medicine and science today, and the ‘guilty until proven innocent’ psychologising of not-yet-understood illnesses. I just hope the lessons that are here to be learned create a much-needed paradigm change.
Wonderfully written article. Thank you for your hard work.
Thank you David. I was originally diagnosed in 1969, with Post Viral Fatigue (a disease not a transient state) Unfortunately the ramifications of that diagnosis were not explained to me. I bumbled and stumbled along until, after one spectacular exherbation in the early 80’s..to being diagnosed with depression. And told to exercise. Well, I did. It was loads of fun until my body gave out… in 1995. I seem to be getting worse, and I’m in bed most of the time. If I venture out too much, I relapse. This is not a disease you fight, it’s a disease you endure. That’s been known since the 90’s as well…but I hope that Mr Tuller’s excellent work will allow us to move a square forward.
Great writing, so easy to read. Thank you David.
I was harmed by GET at an NHS CFS clinic a few years back. I never recovered from the treatment. NICE are going to review the guidelines in 2017 but my guess is the same people who have vested interests in these treatments remaining will be involved in the review, and the same evidence will be said to be high quality even though it is absolute junk – all based on Oxford criteria and subjective measures – just like the last review. The treatments will continue to be offered and thousands more patients, including children, will be harmed by them. People not yet affected by this disease believe this disease happens to other people, not them, not their loved ones, not their own children, but that is not true. And this disease is very common.
Thank you for all your great reporting on our disease!
Thank you for bearing witness to both the struggles we face with this illness, AND the institutional abuse and societal stigma.
From a 10 year sufferer, thank for all you have done and are doing xx
David,
History, if there is any justice, will credit you as one of the key people to expose the systemic bias against ME and ME patients that pervades political, research and health care institutions around the world.
Similarly, Wessely et al will be noted infamously for the reasons you outlined.
Thank you David. As an ME patient, I hope to live long enough to witness this eventuality.
I wish you would research those who have successfully recovered from CFS. You would find out so much more about this disease. I was very sick with CFS and fully recovered my health. I’m available to talk about it any time
Rebecca Metro, I have had CFS/ME since 1969. When it was finally named in the mid 1990s I started trying everything that came along and still do. It’s an enormously long list but I don’t intend to stop trying. If you could please outline your thoughts about recovery I would be extremely grateful. I’m sure there are many commenting here who would dearly like that sort of information too. Thank you
I literally had a (kindly – his heart was in the right place) doctor recommend ‘perpetual motion’ as a treatment for me – on grass though, so when I collapsed/fainted, I wouldn’t be badly injured.
Thank you for this article. My first diagnosis was ME/CFS. I ignored the diagnosis and carried on; my health slowly deteriorated. Then I suddenly got really sick. Thyroid well out of whack, leg swollen up and wouldn’t fit in my pants, liver count low… all that righted itself within a month or two, but I was still severely unwell. Since then I was diagnosed with severe postural orthostatic tachycardia syndrome as part of generalised dysautonomia. There is objective testing for all this (same of my results – shocking). I am considered permanently disabled. The head neurologist at my country’s largest hospital (where I underwent investigations for almost 2 weeks a year and a half after becoming disabled) says he believes the POTS, dysautonomia, are all tied in with my original diagnosis of ME/CFS. He did not recommend exercise. He did not believe medical science had the answers for me and others like me, yet.
Getting to the truth about the flawed PACE trial will hopefully lead to further relevant and useful research being undertaken – instead of what has dominated the scene prior to now. People the world over are waiting to get better. We’re doing the best with our lot, but meaningful recovery just isn’t within our control. I for one am not afraid of exercise. I have ADHD and not moving is like torture. So I get around and do things… I suffer greatly for it. In the back of my head I live with concern that my overdoing it will mean I require hospitalisation again. As much as exercise and activity are sometimes pushed on patients with CFS/ME – doctors also don’t appreciate a patient who has overdone it around the house landing in hospital with severe polyuria (one of my body’s annoying ‘quirks’ in reaction to too much physical exertion) and requiring 3L of IV fluid in quick succession.
As well as objective testing measures – because I have used my own checks & balances all along this journey (‘Is there any correlation – negative or positive – between my physical symptoms and mood?’ etc) and my husband has done his own version – I am confident that this illness is of physiological aetiology. I know there are millions more out there suffering from physiological illness similar to my own. Research will eventually lead to targeted and effective treatment options. The challenge is in making sure the limited research funds available for ME/CFS are going to where we’ll get most bang for our buck. Not in the sense that governments and insurers view it (saving money) but in eventual improvements in quality of life for those with the disorder.
Having experienced disbelief, skepticism, and snarking from doctors and friends when I suffered from what was eventually diagnosed (16 years later) as Lyme disease, I believed my husband when he spoke of the unrefreshing sleep, fatigue, cognitive fog, and other symptoms that plagued him. I wish he could find a therapy or combination of therapies that would resolve his illness. We are guardedly hopeful about some of the biomarkers and metabolites research recently reported, but we recognize the depth of misunderstanding and disbelief that still exists in the medical community, much less the general population. Thank you for your continued, thorough, compassionate focus on this disease.
Excellent article. Would you consider looking at the mitochondrial theory of chronic fatigue? I think it has some merit. Also I find many with apparent CFS have actually got POTS, Ehlers Danlos Syndrome or both. Also the emerging work on Mast Cell Activation Syndrome promises potentially useful options for treatments- see Dr Lawrence Afrin’s book.
Keep up the good work!
i was diagnosed with both CFS and POTS at the mayo clinic. my impression is that lots of CFS patients have comorbidities like that, though i would much prefer not to have this alphabet soup of diagnoses!
David Tuller’s compassion, empathy and understanding is a balm to the soul of this ME/CFS sufferer.
What a fantastic article. I wish this article was required reading for all medical professionals, including government health agencies. Thank you for writing this.
Thank you, David Tuller, for writing this vital article.
There currently exists so little we can show doctors when they recommend exercise therapy for ME/CFS. This article helps fill that void.
Many (I would suggest most) doctors still see ME/CFS patients as noncompliant and uncooperative when we insist graded exercise therapy causes longterm harms.
Just this month, a doctor prescribed for me “30 to 45 minutes of vigorous exercise a day”. This just after we discussed how graded exercise therapy had left me mostly homebound and unable to work for the past 3 years. Unbelievable.
In response to Jeff,I relate to his position.Having been persuaded to try GET in 2005 I went from moderate ME to severe and housebound barring medical appointments.Then in 2014 my GP actually suggested that “I give it another go”!……if I had had a similar reaction to a drug,I doubt she even would have thought about”having another go”The situation here in the U.K. Is the stuff of nightmares.Thank you David Tuller for your determination to end this fiasco which is literally killing people.
Thank you for writing this article. I am so glad we were warned and stayed away from the biopsyhosocial doctors 6 years ago when my children got sick. They were 8 and 12. Now we are waiting eagerly for new research that might save them from spending young adulthood as patients. They already lost years from their childhood and teens
The illness wrecked my health.
NIH, CDC, the Wessely School, ignorant uncaring doctors, and society’s reaction to my illness wrecked my life.
Thank you so much for helping to raise awareness about ME/CFS. We patients live a never ending nightmare, in which we are told our life-ruining sickness is not real. We rarely get treatment, and only now, after decades of neglect and mistreatment, is real research beginning.
As a person suffering with Myalgic Encephalomyelitis for more than a decade, I can’t begin to express my gratitude to David Tuller for helping to bring awareness to the plight of all PwME (people with ME).
I look forward to reading more in the near future. How does this happen in the 21st century?
Worse than he disease is the disdain encountered in health care. As soon as the doctors take a look at ‘up to date’ or Cochrane Reviews. There is no care for you. The specialists want you out of their door, and suddenly the pain you have been experiencing must be all in your head. Our community has been at it for 30 years, we have experienced this over and over. Patients have committed suicide over it. Some have died because other diseases have been discounted because it must not be serious since they have this disease called ‘chronic fatigue syndrome’.
Socialized health care system do not approve access to deeper testing other than the usual CBC, thyroid, liver and kidney check. If these are fine, you are deemed in excellent health. Being from Canada, north of the border, I am in good health, south of the border at my specialist office, I am a very sick patient.
Thank you David Tuller for investigating. It is time that the disdain stops.
David,
Thank you. From the bottom of my heart, thank you. Thank you for being a voice and for being willing to tackle this horrible study and to shed light on its disastrous effects. Thank you for not giving in to the easy or popular stories. Thank you for giving millions of people with this disease a voice. And most of all, thank you for so eloquently sharing my mother’s story and for not portraying her as a victim. For recognizing the vibrant and amazing person that she still continues to be in spite of this horrid disease.
I’m pretty sure the PACE ‘study’ was designed to make it seem as if the victims were lazy and unmotivated, and could get well if they just got motivated and made an effort. It would save money now spent on treating symptoms (however pathetic that quantity is – ME/CFS is severely underfunded in the US, too) if the ‘doctors’ and ‘scientists’ can merely blame the victims.
As a former research physicist at the Princeton Plasma Physics Lab who lost my ability to do the job I trained for 27 years ago to this horrible thing, I can tell you that we, as a group, would follow ANYTHING with a proven record. And waste a lot of our tiny bit of energy trying an amazing array of supplements and medicines and treatments (none approved for CFS) because we are so desperate.
Excellent article – I just wish the right people would read it!
PS Wish I could also get people to read my novel Pride’s Children, one of whose three main characters is a physician who has had her life destroyed by CFS (review copies available).
Thank you, David Tuller, for all you’ve done and continue to do to bring attention to this appalling medical scandal. If patients could award a Pullitzer, you’d have one!
Unfortunately in the UK the overriding guideline authority NICE are refusing to revise their guidelines until 2017 (and probably late part of that year) and in the meantime MAGENTA (GET for Children with ME/CFS) and MEGA are about to start – and MEGA has several major people who are Psychs and heavily invested in GET and CBT so is very likely money down the drain for nothing. They won’t even amend to say that GET can be harmful and should be considered very carefully if not avoided all together!
Doctors in the UK and specialists have eaten up the “self belief of restriction” that PACE and the “Yuppie flu” era birthed and therefore refer to a fatigue management course and push “small increases in daily activity” as the solution. Asking for any other symptom to be investigated (heart issues, persistent pain and weakness in certain areas of the body etc) gets a *shrug* and “we aren’t allowed to look into those, it just complicates things”. I had to fight hard to even get a referral for an issue that I have had for over 10 years prior to my diagnosis because their impression is if I just manage my life better I’ll beat the fatigue and I’ll be healthy again.
The fatigue course is worse than that – a few pretty charts pulled from the internet to show you “normal” human being systems and reactions and to urge you to go to bed at the right time to work with the body’s “natural rhythm” (yeah, with an illness that includes insomnia as a symptom?), meditation (helpful but not a cure), Mindfulness (for those in pain being made fully aware of every part of your body that hurts and repeating “and this is ok” doesn’t work) and of course urging to increase your activity in a by-any-other-name version of GET. That’s the second half of each of the 7 sessions.
The first half was a “how have the last two weeks been since we last saw each other” and encouragement to say we feel better already. Failing to say something that is better results in probing and pushing and urging that you could have changed something and if only you had done so you would. I once had enough of this and having already suffered from Bells Palsy during the course – cause unknown, the medical reaction was largely a *shrug* – I retorted that actually making my way to the course being a 2 hour trip each way and the energy it used had actually pushed me backwards and I was having to restrict my other activities more. This of course got a hugely unhappy response and what can only be called a “cat-butt face” from one of the course runners because she’d failed to make me say something happy and wonderful. That face got even worse when one of the other group members replied they felt the same as me and were struggling due to the extra they were doing due to the course as well and several others made agreeable noises. Every session we all walked out and said “well maybe next time will be of some use…”!
It took me over a year to get back to a level of health I had pre the course and pre-diagnosis and frankly I often refer to the diagnosis as a DNR mark on my medical file (nothing to do with my health will ever be taken seriously again) and being worse than not knowing. And yet when I go to the GP I still get told “well the fatigue course is effective so those who are researching drugs that allege it isn’t I don’t think much of their research and won’t even consider their trial findings to be relevant” (paraphrased but that was the gist). This was just after we discussed that the course didn’t help me at all and made me worse!
30 but feeling 80… and hoping that the treatment situation actually changes before I reach 80!
Thank you! Im not able to read it all but I have sent it off to my new neurologist who wanted to start me on exercise therapy. So dangerous when data is false and people suffer. I was convinced to try a very mild exercise therapy a year and half ago and I have never recuperated.
Fantastic article David Tuller.
Thank you David Tuller for this in depth article. You give all people with ME huge hope for the future.
You’ve nailed it David! The whole history of the treatment of this illness reeks of self-served promotion, status and financial interests. When I first started to look at the psychosocial studies on ME/CFS I just couldn’t believe how terrible they were from a logical, scientific, methological or statistical point of view. One day people will look back on it in the same way that they now look back on the attempts to prove that smoking was not harmful, and look at how many doctors were involved in that!
Thanks.