A Mysterious Amnesia, Related to Opioid Overdose, Creeps Beyond New England
Just over five years ago, a man suffering from amnesia following a suspected drug overdose appeared at Lahey Hospital and Medical Center in Burlington, Massachusetts, a Boston suburb. He was 22, and had injected what he believed to be heroin. When he woke up the next morning, he was extremely confused, repeatedly asking the same questions and telling the same stories. Doctors at Lahey quickly diagnosed the man with anterograde amnesia — the inability to form new memories.
His brain scan revealed why. “I thought it was an extremely strange scan — it was almost hard to believe,” said Jed Barash, a neurologist working at Lahey at the time. In the scan, the twin, seahorse-shaped structures of the man’s hippocampi were lit up against the dark background of the rest of the brain — a clear sign of severe injury to just that one region.
“It was strange because that was all there was,” Barash said.
Memory researchers have known since the late 1950s that the hippocampi are responsible for turning short-term memories into lasting ones, so the amnesia was not surprising. Just how the damage occurred, however, remained a mystery. Lack of oxygen to the brain that would have occurred during the overdose could not be the only explanation. The number of survivors in the state that year could easily have numbered in the thousands, so why was there only one patient with this seemingly unique brain damage?
Along with his colleagues, Barash — now medical director at the Soldiers’ Home health care facility in Chelsea, Massachusetts — figured that the opioids must have played a role, and that hunch became only more acute as three more patients — each fitting the same pattern — appeared at Lahey over the next three years. All had the same unique destruction of the hippocampi, all had amnesia, and all were suspected to have overdosed. By that point, the doctors at Lahey faced two fundamental questions: What was causing the strange new syndrome? And precisely how rare was it?
Both questions remain unanswered, but a case report published today in the Annals of Internal Medicine adds to a growing body of evidence suggesting that the problem is far from isolated, and that a potent opioid variation could be involved. A total of 14 patients have now been identified in Massachusetts, one of whom was first admitted to a hospital in his home state of New Hampshire. The new case study reveals two more patients — one from Virginia, and one from Maryland. Both turned up at a medical facility in West Virginia.
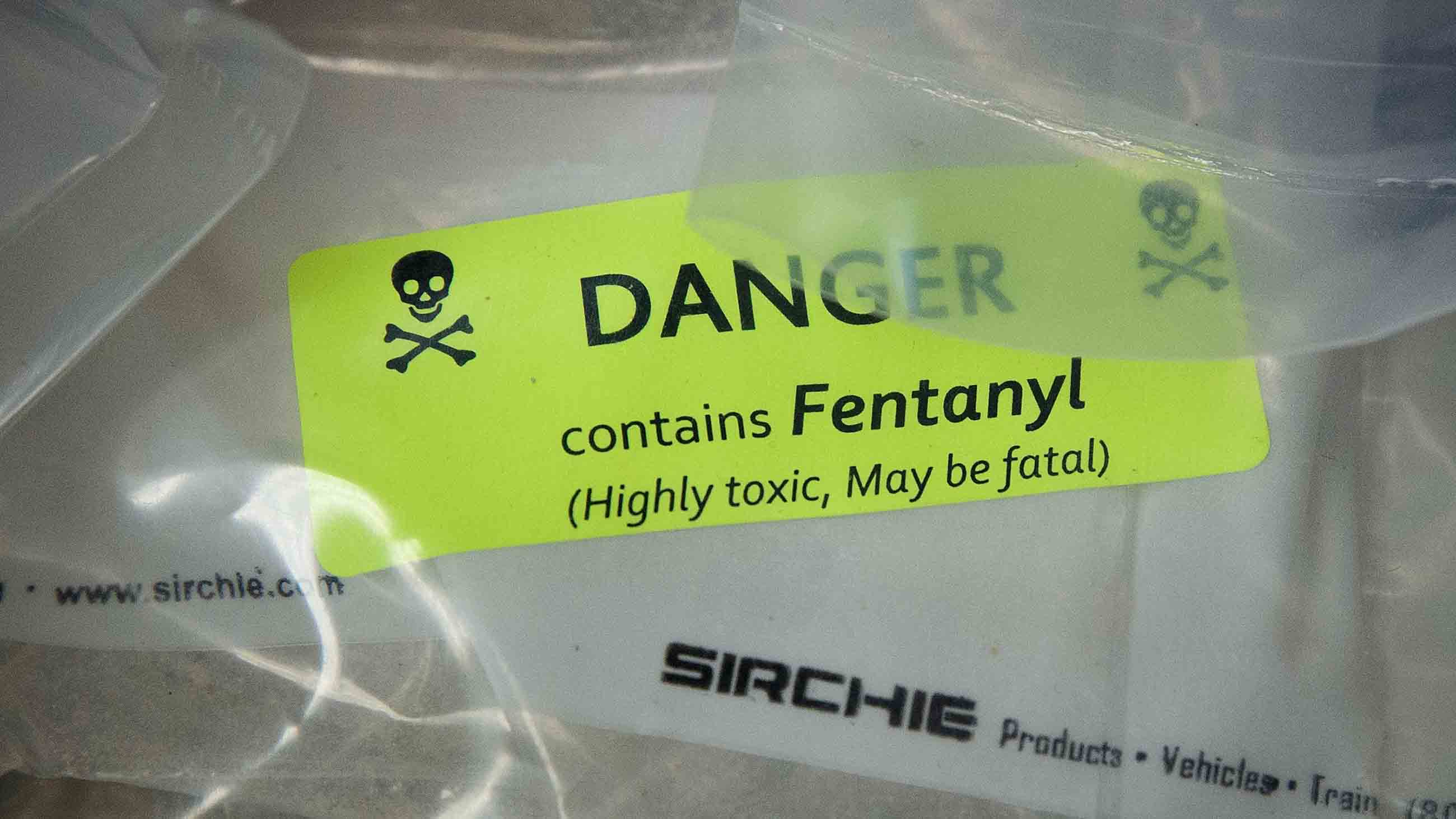
Although many of the patients had taken a variety of drugs, all but one either have a history of opioid use or tested positive for opioids. The most recent case, a 30-year-old man examined last year in West Virginia, is the first patient proven to have taken fentanyl, an extremely potent and dangerous opioid that is rarely tested for in toxicology screens.
There are many barriers to determining the true scope of the problem, from lack of proper testing to the fact that many patients never come to attention in the first place. And amid a larger opioid crisis that some experts say could claim as many as 500,000 lives over the next decade, pinning down the cause of a dozen or so amnesia cases can seem trifling. “It’s sort of like the Titanic going down and you’re worried about some details,” said Alfred DeMaria, the state epidemiologist for Massachusetts.
At the same time, DeMaria suggests that, at the very least, these patients may offer a different route for understanding a disorder, as was the case with a small cluster of patients in the early 1980s who developed Parkinson’s disease after taking contaminated drugs — a misfortune that turned out to be limited to a few people, but which nonetheless gave Parkinson’s researchers a new tool for studying the disease. More worryingly, he also points to several examples of medical investigations that began with a small number of mysterious cases and turned out to have significant public health implications, such as the appearance of West Nile Virus, or the AIDS epidemic.
Bertha Madras, a psychobiologist at McLean Hospital in Belmont, Massachusetts and a member of President Donald Trump’s Commission on Combating Drug Addiction and the Opioid Crisis, agreed that getting to the bottom of these amnesia cases is crucial — particularly given that many cases may be going undetected since the type of cognitive testing needed to diagnose amnesia may not be routinely done in overdose survivors. She also suspects that with overdose antidote drugs like naloxone becoming more widely available, it is possible that more patients, rather than turning up dead, will show up at hospitals.
And with more survivors, Madras said in an email message, “there conceivably will be more cases of brain damage, especially in the very oxygen-sensitive hippocampus, the ‘epicenter’ of initial learning and memory.”
After encountering more patients following that first one in 2012, Barash contacted the Massachusetts Department of Public Health in 2015, which put out a request to emergency room physicians, neurologists, and radiologists statewide for information that might identify additional cases. By the end of 2016, a total of 14 people who matched the pattern had been identified. Then, in May of 2017, the DPH made what they called “an unusual amnestic syndrome” with “acute, bilateral hippocampal” damage a reportable disease syndrome — a status that requires any doctor who sees such a case to forward patients’ medical records for review.
As of today, however, DeMaria believes there is no such mechanism in place in other states, and that’s one of the barriers to getting a handle on the prevalence of the amnestic syndrome. Marc Haut, the neuropsychologist who examined the man from Virginia in 2015, and one of the authors on the new Annals paper, had no way of knowing about the investigation in Massachusetts and initially chalked up the damage to cocaine use. At the time, he saw no reason to consider opioids, in part because of the information the patient shared with him. “Patient reports about substance use [are] not always accurate for a couple of reasons, one being the patients themselves,” he said. “And the other being that patients often don’t know what they’re buying and using.”
So it was not until he received an email from Barash that Haut, the chair of the behavioral medicine and psychiatry department at West Virginia University, reconsidered whether opioids could have played a role. To date, only eight of the 16 patients reported in the cluster had cocaine in their system, making opioids a more consistent link than any other drug. Barash, who is also an author on the Annals paper, wonders if fentanyl — considered to be 50 times more potent than heroin — is a key component, in part because the timing and location of the appearance of these amnestic cases parallels the rise of fentanyl overdoses in two of the hardest hit regions in the country. Teasing this out is complicated with the ever-changing landscape of drugs that people are taking, often in combination. “Cocaine overdose deaths are escalating,” said Madras, “along with evidence of combined use of fentanyl, heroin, and cocaine in some deaths.”
And despite the fact that fentanyl abuse has become so common, routine toxicology screens don’t test for the presence of the drug. It was only because Haut had been tipped off that he requested the advanced toxicology screen for the 2017 patient, which found evidence that he had taken fentanyl in addition to cocaine. His MRI scan also revealed the signature hippocampal damage: “bright, big, and intense,” according to Haut.
Like Barash, Haut is concerned about the possibility that what they’ve seen so far could be just the tip of the iceberg. “We don’t know if this is a rare occurrence, or if this has occurred more, and people have not noticed,” he said, “because some of the folks who have these events are pretty marginalized in society. If they don’t have family to notice, it may not be noticed even though it’s pretty dense amnesia.”
Several other doctors who contributed cases to the Massachusetts cluster have also raised the question of whether more patients are going undetected. They point to the fact that many illegal drug users don’t go to a hospital after an overdose. If they do, their confusion is likely to be chalked up to a temporary symptom of the overdose. If they don’t get to a hospital within a narrow window of approximately one week, the telltale signal may have faded from the brain and all evidence of drugs will likely have cleared the system.
Even if all those conditions are met, doctors across the country don’t know where or how to share the information. DeMaria, the state epidemiologist for Massachusetts, believes his is the only state that has notified physicians and is collecting cases. If doctors in other states are seeing cases that fit the pattern, they may assume that it’s a one-off phenomenon, just as Barash and others did when they first saw the cases.
Michael Lev, an emergency room neuroradiologist at Massachusetts General Hospital who contributed cases to the Massachusetts cluster, thinks it’s possible that the appearance of this amnestic syndrome may date back far earlier than 2012. He recalls seeing similar brain images in a few sporadic cases between 1986 and 1989 when he was working at Boston City Hospital. The patient history was always the same, he said. “The history was ‘heroin found down,’ — emergency room shorthand for an overdose victim.
For now, doctors can only go on the well-documented data that they have — the 16 patients identified between October 2012 and May 2017 — and one key question is whether they represent just one narrow band along a spectrum of damage, which would have ramifications for the ability of addicts to get the treatment they need. “Getting a sense of the severity and scope of this is important,” Haut said. “If we find that these dense amnesias are really rare, that’s good. But if we find in the interim that they have significant memory problems even though they’re not amnestic as a result of these events, that have gone under the radar, then we have to take that into account when we’re trying to get people into treatment and staying in treatment.”
Barash agreed, pointing out that understanding the amnestic syndrome may give medical professionals insight into some of the larger problems that can accompany overdoses. “These cases are a very particular subset of brain damage that can occur from use of opioids,” he noted. “But I think more likely there are probably cases of patients who may not necessarily have this particular syndrome but suffer cognitive difficulties from longer term use of opioids and it’s important to know the scope of that.” It’s also plausible that there are more extreme cases on the other end of the spectrum — people who have taken sub-lethal doses but are too far gone to have their memory tested.
Barash, Haut, and others involved in the investigation are quick to point out that the only way to test this hypothesis is to gather more well-documented cases.
In order to get an initial assessment on the prevalence of the syndrome, at least in West Virginia and nearby states, Haut is developing a study that would put a procedure in place to collect all the relevant information from any person who comes in with an overdose: advanced toxicology screens that would detect fentanyl; MRI scans; cognitive testing; and a detailed clinical history.
But for now, there are far more questions than answers, which is why Barash and Haut are hoping that the new Annals paper, which now clearly documents two patients in locations well beyond Massachusetts — with one of them proven to have taken fentanyl — will expose a wider audience of physicians and researchers to this worrying syndrome, and in turn help to quantify its true scope and potential impact.
“Maybe they’ll see the MRI on the paper and say ‘Oh I recognize this,’” Barash said. “Our hope is that the work that we’re doing triggers recall of a patient they’ve seen in the past or gets a bug in their ear moving forward so that when they’re taking care of patients they know what to look out for.”
Lauren Aguirre is a freelance science journalist based in Boston and a former staff editor, writer, and producer for the PBS series NOVA. She is currently writing a book about memory.
CORRECTION: This article has been updated to correct the credentials of Bertha Madras. She is a psychobiologist, not a psychiatrist.










Comments are automatically closed one year after article publication. Archived comments are below.
I’m right in middle of drug Corredor in Arizona my son has been smoking these fake Fentanyl pills and it’s bad he is 21 years old so I can’t make him go get treatment but it’s crazy how fast and hard he is going down hill he has only been using for 6 months and he isn’t the same kid I know he is slow and not cognitive mental state is gone I need help to help him or he will never be the same
Millions of chronic pain patients have been taken off of opioids and place on Gabapentin or Lyrica – both of these are KNOWN to cause memory loss yet you are more worried about 15 people who are breaking the law and illegally taking fentanyl-laced heroin. Just do a quick search on google for “gabapentin memory loss” and you will be stunned by what you see by this common replacement for opioids.
Thank you! This is pretty much exactly what I was going to post, but you said it for me. Everyone cares about the addicts that choose to abuse these medicines, no one cares about chronic pain patients. Doctors prescribe us any number of toxic, harmful substances like Gabapentin with no thought to the side effects. As long as we’re not taking opiates, right? I’s total BS. Anyways, thank you for saying this Paul. It needed to be said and I appreciate your comment.