The Problem With Labeling Gut Troubles ‘Dysbiosis’
On the first page of Heinz Koop’s fecal analysis test results, a bar showed where he fell on a gradient from green to red. A label above said, in German: “Overall dysbiosis.” Koop was not in the green or even the yellow regions, but a worrisome orange. It was a bad result — but, he says, “I was kind of happy.”
Doctors hadn’t given him a satisfying answer about his recurring bloody diarrhea and other gut troubles. But Koop had learned on Facebook that he could test his gut microbiome — the community of bacteria and other organisms living in his gastrointestinal tract — to look for problems. Koop ordered a test from a German laboratory called Medivere. The results said his gut microbes were imbalanced, which was something he thought he could treat. Soon he would be attempting to correct this imbalance by chauffering a friend’s fresh stool samples home to implant up his own colon.
Trillions of microbes living on and in our bodies, especially our guts, make up our microbiome. The bugs in our bowel are not just there to slow down our poop, as one researcher speculated in 1970, but are intricately connected to our health. Gut microbes help us digest our food, make critical vitamins, and keep pathogens out. Over the past decade or so, research into the microbiome has exploded as researchers have tried to tease apart the complex connections between our diseases and our resident microbes.
Today, at least 10 percent of published microbiome papers use the term dysbiosis to describe changes in the microbiome, estimates Katarzyna Hooks, a computational biologist now at Evotec, a global biotechnology company headquartered in Germany. Some scientists say the term is useful for communicating a specific finding, though they acknowledge its limitations. Other scientists hate it.
The problem is that dys- means something negative: dysfunction, dyslexia, dystopia. Dysbiosis suggests not just a change, but a bad change. “They’re implying something imbalanced or wrong with our microbiome,” says Fergus Shanahan, a gastroenterologist and microbiome scientist at University College Cork in Ireland. But in the very new field of microbiome research, the links between our gut bacteria and disease have yet to be untangled. In most cases, researchers don’t know whether a change to the microbiome is bad. It may be a side effect of an illness. It may be an adaptation by our gut bugs to new circumstances. What seems abnormal might be normal.
Hooks, Shanahan, and others argue that use of the term dysbiosis is a failure not just of scientific communication, but of scientific thinking. “Words we use have inbuilt prejudices,” Shanahan says. Even if scientists don’t intend to mislead their readers, “they can actually mislead themselves.” As that confusion has reached the public — in part through direct-to-consumer testing kits — it has contributed to an untold number of people attempting to give themselves fecal transplants, which researchers say is a potentially dangerous action with little basis in science.
The Human Microbiome Project launched in 2007 with lofty goals. Researchers would use new technologies to minutely analyze a large number of microbial communities, and the resulting data would transform our understanding of the role our resident bugs play in health and disease. In samples from 300 healthy people, scientists studied bacterial species, genes, and gene products. The project’s second phase, which looked at the microbiome in three specific health conditions (pregnancy and preterm birth, inflammatory bowel disease, and the onset of type 2 diabetes), wrapped up earlier this year. In total, the project amassed 42 terabytes of data.
Yet it revealed that in our guts, we’re more different than we are alike. Among all that data, no universal or normal microbiome appeared. The results suggest that “there’s a tremendous number of ways to assemble microbiomes in people who are apparently healthy,” says Rob Knight, a microbiome researcher at the University of California San Diego, who worked on the Human Microbiome Project.
Further, when comparing groups of sick and healthy people, it can be difficult to determine whether any differences in the microbiome are a cause or an effect of illness. It’s possible that the microbiome difference caused the disease, scientists say. But it’s also possible that the disease changed the microbiome. “I think it’s far more exciting, and far more likely, that most of these changes are secondary to the disease,” Shanahan says. Those changes might even be appropriate ways for our bodies to respond to an illness.
There are other possible explanations, too. Knight cites the example of type 2 diabetes: some differences in the microbiomes of diabetic people turned out to be caused by metformin, a common diabetes drug. Or an illness and a microbiome change could mutually reinforce each other. In that case, treating the microbiome “might not be able to get you out of that loop,” Knight says. You’d still need to treat the underlying illness.
Some experiments have given tantalizing hints about times when microbes might truly be in the driver’s seat. In a 2013 paper, researchers implanted gut microbes from obese and non-obese humans into mice. The “germ-free” mice were raised in completely sterile environments so they had no microbiomes of their own. When mice received microbes from obese people, their own body fat increased by about 10 percent. The study made a splash in the news: “The microbes in your gut may be making you fat;” “Bacteria from slim people could help treat obesity;” “Gut bacteria ‘may be obesity weapon.’”
“It’s very intriguing,” says Knight, who was one of the paper’s authors, “but it doesn’t establish causality in humans.” Mice are not just miniature people. That was illustrated well by an earlier strand of obesity research that focused on the hormone leptin. When scientists injected leptin into obese mice, they slimmed down dramatically. But clinical trials in humans were a bust, because the molecule doesn’t work the same way in our bodies.
In their 2017 paper, Hooks and coauthor Maureen O’Malley analyzed more than 500 journal articles about the microbiome that used the word dysbiosis. They found that more than half of the papers defined dysbiosis as an imbalance. Other common definitions were either a general change, or a change in a specific bacterial type.
“I came to think ‘dysbiosis’ is a placeholder,” Hooks says. “But unfortunately it is also a lazy choice.”
Shanahan and a coauthor made a similar argument in a 2019 paper. So did the Massachusetts Institute of Technology’s Scott Olesen and Eric Alm in 2016, calling the idea of balance in the microbiome “a holdover from prescientific thought,” akin to balancing the humors. Olesen is now the scientific director at OpenBiome, a nonprofit stool bank that collects and processes donor feces for use by doctors and researchers. He says he and Alm felt frustrated by how other researchers were talking about dysbiosis.
“It’s not a thing,” Olesen says.
Yet some researchers say dysbiosis is a perfectly good word that’s been used too broadly. They have no problem with using the term in their papers, under certain conditions. For example, Andreas Bäumler, a microbiologist at the University of California Davis, doesn’t shy away from the word. He considers the gut microbiome to be an arm of the immune system whose job is to keep invading pathogens out. He defines dysbiosis functionally as the failure of that immune arm to protect the host, regardless of which bacterial species are present.
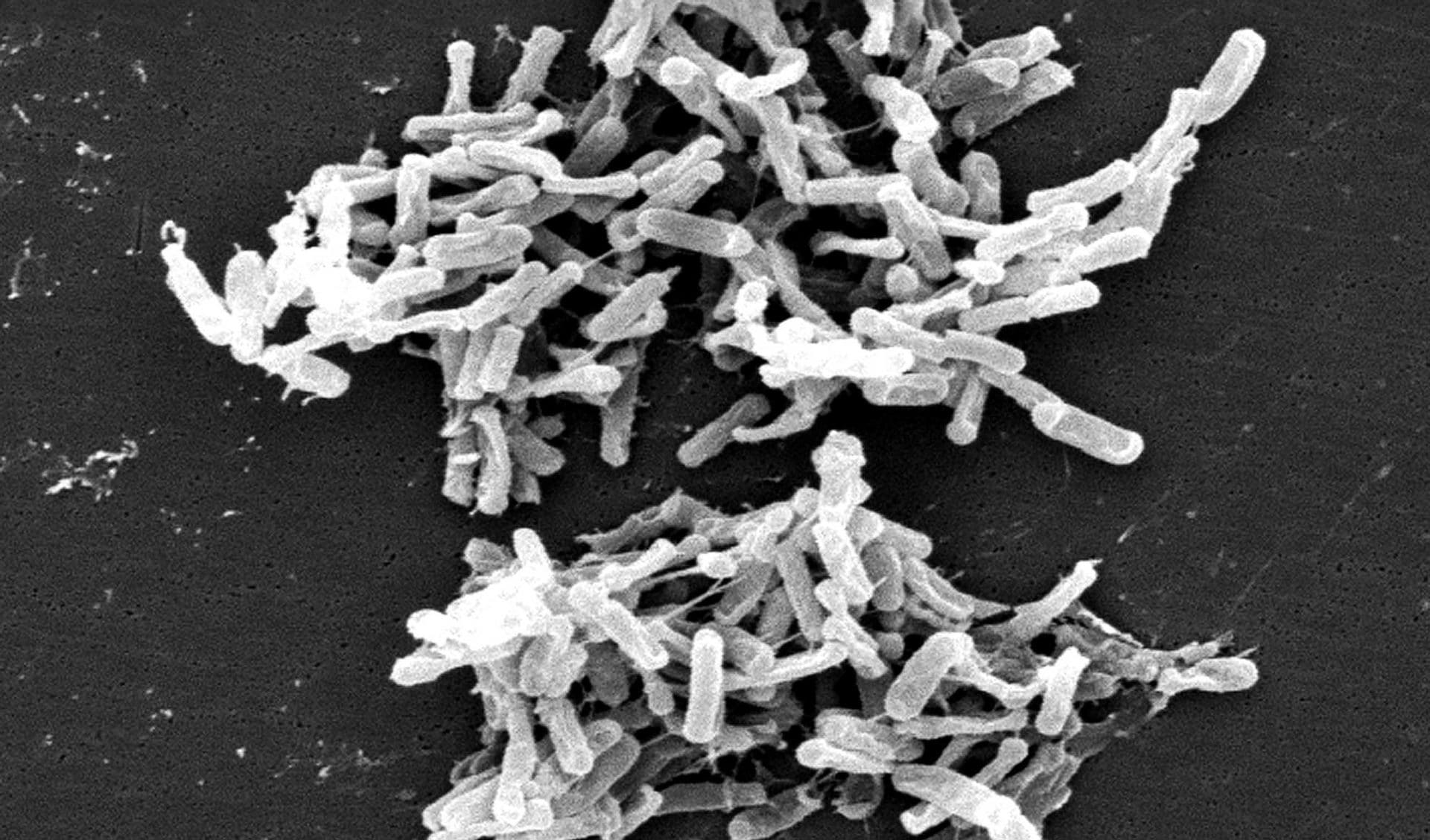
Purna Kashyap, a gastroenterologist and microbiome scientist at the Mayo Clinic in Minnesota, also publishes papers on dysbiosis, although he says he doesn’t like when the word is “used to describe any change in the microbiome.” Kashyap argues that anyone who’s healthy has a healthy microbiome. His own definition of dysbiosis is slightly different from Bäumler’s: it’s when “the microbial community is disrupted in a way that is having a harmful influence on the host,” he says. For example, in a recent paper Kashyap and others found that some diarrhea patients had distinctive gut microbial communities. When those patients’ feces were transplanted into germ-free mice, the mice were more vulnerable to infection by Clostridioides difficile, a pathogen commonly known as C. diff that causes half a million illnesses a year in the U.S. alone.
“There are very few diseases where any causative link has been established in terms of the microbiome,” Kashyap says. But when research papers or news articles proclaim links between diseases and dysbiosis, he says, “patients want to test their microbiome and see if they have dysbiosis.”
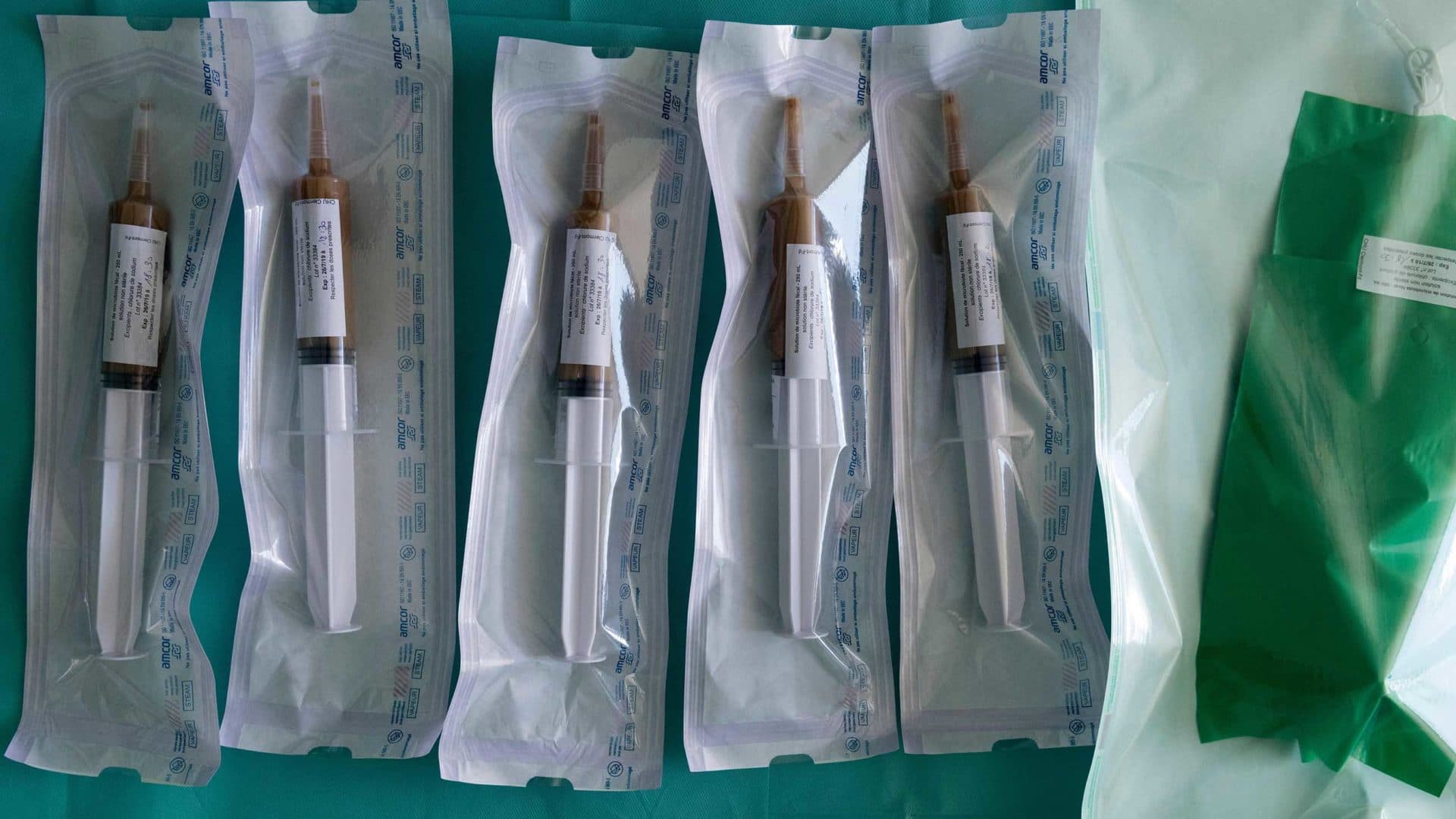
Because the potential effects of fecal microbiota transplantation (FMT) are so poorly understood, the only way to receive one from a doctor in the United States is if you have recurrent C. diff. — for which fecal transplants are nearly miraculous — or are part of a clinical trial. That means patients in the U.S. who want doctors to test or treat their microbiomes may be disappointed.
For years, Lindsay Calverley, a 34-year-old in California, had been plagued by digestive troubles that affected every aspect of her life. Doctors couldn’t give her an explanation. But she suspected something was wrong with her microbiome, and the genetic tests of her stool that she ordered from multiple companies seemed to confirm her worry. (Several companies offer stool sequencing; they include Viome, Thryve, and Diagnostic Solutions Laboratory, which sells a test called GI-MAP. Costs range from under $100 to more than $400.)
“I’ve had probably five or six different fecal tests done that have identified some level of dysbiosis one way or another,” Calverley says. “Sometimes it’s an overgrowth, sometimes it’s an undergrowth, sometimes it’s just the wrong balance.” Eventually, she decided to try re-balancing her microbiome herself. She contacted a private seller in Florida who charges $80 for six ounces of filtered feces. Twelve hundred dollars later, a package of poop arrived for Calverley, frozen and on dry ice. It was 14 treatments, the most she felt she could afford at the time.
Shanahan notes that although bacterial overgrowth, as in Calverley’s tests, is a recognized medical entity, it happens in the small intestine, not the colon, and can’t be diagnosed from feces. Like Kashyap, he has also received patient requests for fecal transplants to treat their microbiomes. For people like Calverley who are desperate for relief and frustrated by a lack of answers from their doctors, a stranger’s feces can seem full of promise.
This January, Kashyap joined the advisory board of uBiome, one of the companies offering microbiome sequencing. He joined “exactly for this reason,” he says, “to advise them on how to make their approach to reporting more scientific and more transparent.” The company’s reports tell users every bacterial type in their stool that’s outside of a “normal” range, and the diseases those bacteria are associated with. A sample report from uBiome, for example, says a patient is at increased risk of cardiovascular disease because of “low” Alloprevotella.
“This creates anxiety among patients,” says Kashyap, adding that he has expressed his concerns to uBiome on multiple occasions. It may be a moot point now. The FBI raided uBiome’s office this spring, investigating practices such as billing patients multiple times without their consent. The company has since filed for bankruptcy and plans to shut down.
American Gut, a crowdfunded spinoff of an effort to catalog global microbial diversity called the Earth Microbiome Project, also sequences the microbial DNA in stool and offers data about how participants compare to others. “We try very hard to explain to them that variation is expected, and to explain to them that it’s not a clinical test,” says Knight, who cofounded American Gut. He sees it as a citizen science project; findings were published last year from more than 10,000 participants. But Knight acknowledges that many people sign up because they think they’re getting medically useful information.
The only test that can really tell you whether you should get a fecal transplant, Knight says, is a test for C. diff. If people are looking for other answers from a microbiome test, “that’s not where the science is right now, unless you’re a mouse.”
Heinz Koop posted a photo of a fresh turd balanced on a paper liner over a toilet bowl on Facebook, asking: “This is his stool, what do you guys think?” In this Facebook group for FMT enthusiasts and in other groups like it, people share their experiences with fecal transplants for conditions like anxiety and acne, or for their children with autism — or even for their dogs.
The stool in Koop’s photo belonged to a friend, “like the healthiest person I knew, and very athletic,” Koop says. He thought this friend might be a good donor, though commenters on Facebook were mixed about whether the specimen was well-formed enough. Nevertheless, Koop gave himself four enema treatments with his friend’s feces.
It was simple: “He lives like 10 minutes away from me,” Koop says. “He put it in a small box and put it in the fridge. Then he was messaging me like, ‘OK I have a new sample.’” But after the friend’s own microbiome sequencing results came back with some data Koop didn’t like, they put the experiment on hold. Koop thinks the transplants helped him a little.
Lindsay Calverley also moved ahead with her home FMT. Since she had already been giving herself daily coffee enemas, adding a bucketful of a stranger’s stool barely changed her daily routine, she says. But after using up the donations, she didn’t feel better. If anything, she had new symptoms.
Calverley wrote to her donor and got a refund.
“We have good evidence that [FMT] is very good for one thing,” says Olesen, “and beyond that it’s such an open question.” His organization, OpenBiome, has shipped more than 50,000 treatments to medical facilities for C. diff infection. Outside of C. diff, the stool bank only works with doctors who are conducting clinical trials.
Despite the huggable, blowup poop emoji propped in the center of the OpenBiome office, Olseson doesn’t take FMT lightly. “We here think of it as a serious medicine,” he says. He wonders whether all-natural stool, and the widespread language around microbiome “balance,” make FMT appealing as a kind of holistic treatment. “If you think anything is wrong with your body, there’s some kind of literature to say that it could be related to the gut microbiome,” he says. Fecal transplants may seem like a cure for whatever ails you.
Beyond not always curing people, though, fecal transplants can kill. Earlier this year, the Food and Drug Administration announced that two immunocompromised adults receiving experimental FMT from a doctor had contracted drug-resistant E. coli infections. One of them died. In response, the agency advised additional protections, including screening donors and their stool. (A statement from OpenBiome says the company was already doing this type of screening, and did not provide the tainted treatment.)
Another reason FMT is risky is the same reason the science around it is so exciting: Researchers have found links between the microbiome and conditions like Parkinson’s disease, multiple sclerosis, and cancer. If any of those links turns out to be causative, a fecal transplant from a seemingly healthy person could carry hidden risks down the road.
“What’s been established is that the microbiome is associated with a lot of aspects of health that no one had any idea it was involved in 20 years ago,” Knight says. Figuring out when the microbiome causes a disease, and when it’s merely a side effect, is a work in progress. Scientists aren’t even sure how fecal transplants cure recurrent C. diff.
While they work toward answers, scientists will probably continue to use the term dysbiosis. “I think it’s already a lost battle,” Hooks says. But she argues that “asking people to explain what they mean by it” is still important. Does an experiment show that an illness causes a microbial difference, or vice versa? That the whole community of microbes has shifted, or that certain bugs have appeared or disappeared? Or simply: something’s different?
“We have a responsibility to get the language right,” Shanahan says, adding that science is the pursuit of the truth. “Why would you use a word that’s one step removed from the truth?”
Elizabeth Preston is a freelance writer whose work can be found in New Scientist, Discover, Quanta, The Atlantic, and STAT News, among other publications.











Comments are automatically closed one year after article publication. Archived comments are below.
Socialism’s primary weapon is designating normalcy as thoughtcrime, madness as sanity, and stupidity as leadership. If the borderless New World Order had a motto, it would be “up yours.” OTOH, they do supply a syringe.
This article is missing information about resistant starch and other prebiotics for improving the intestinal microbiome and microbial balance. With more than 220 published human clinical studies on natural sources of resistant starch alone, there is certainly sufficient evidence that it should be included in these types of articles. For instance, Stephen O’Keefe from the University published a diet swap between black South Africans and black African-Americans which showed that resistant corn starch and removal of dietary fat shifted the entire microbiome, lowered the inflammation biomarkers and reduced risk of colon cancer. https://www.nature.com/articles/ncomms7342. For all the clinicals on resistant starch, visit http://www.ResistantStarchResearch.com. This approach matches historical dietary consumption and is significantly less risky than fecal transplants.