When Measles Arrives: Breaking Down the Anatomy of Containment
On an otherwise normal Thursday in November 2018, the doors to the Lowell Community Health Center in Massachusetts opened at 8 a.m., as they always do, and the first of 802 patients who would walk through those doors began trickling in. They each took a number and waited to register at the front desk. They pressed buttons for the elevators that would take them up to the floor they were directed to, and there they took a seat and waited again to see a doctor or nurse. They eventually completed their appointments and departed, minutes or hours later, perhaps with medicines, prescriptions, or diagnoses in hand.
This routine — a seemingly banal choreography repeated hundreds of times each day — continued until around 12:50 p.m., when a mother arrived with her two-year-old daughter. The child had measles, and suddenly, this was no longer an ordinary day. For virtually anyone not immune to the virus who crossed paths with the toddler, infection was almost certain, and so all of those places the child had been and the rooms where she may have coughed or sneezed became critical evidentiary artifacts in a crisis that had all the potential to spin quickly out of control.
Indeed, the arrival of mother and child set off a chain of events and triggered longstanding but rarely tested protocols aimed at containing a measles outbreak. It involved hundreds of staff not just at the Lowell Community Health Center, but also the Massachusetts Department of Public Health (DPH), the City of Lowell Health Department, and the local hospital — with thousands of emails and a weeklong flurry of activity that strained the center’s capacities to the limit. They would need to figure out exactly who had been in the lobby, in the pharmacy, and in the pediatrics department during the crucial time window when the child with measles was in the facility. They would have to get back in touch with the nearly 550 people who may have been exposed as they moved through the center’s spaces, and locate enough vaccine supplies to immunize anyone who needed it, all within 72 hours of the initial exposure.
That the center managed to contain the highly-contagious measles virus is a testament to its modernized records system, its staff’s military-style precision, and its location in a resource-rich region. But even here there were occasional missteps, bouts of confusion, and administrative second-guessing and finger-pointing. There were also 179 exposed people with no evidence of vaccination — even though the center tried to reach them — suggesting that the fallout at a less-prepared facility could be disastrous.
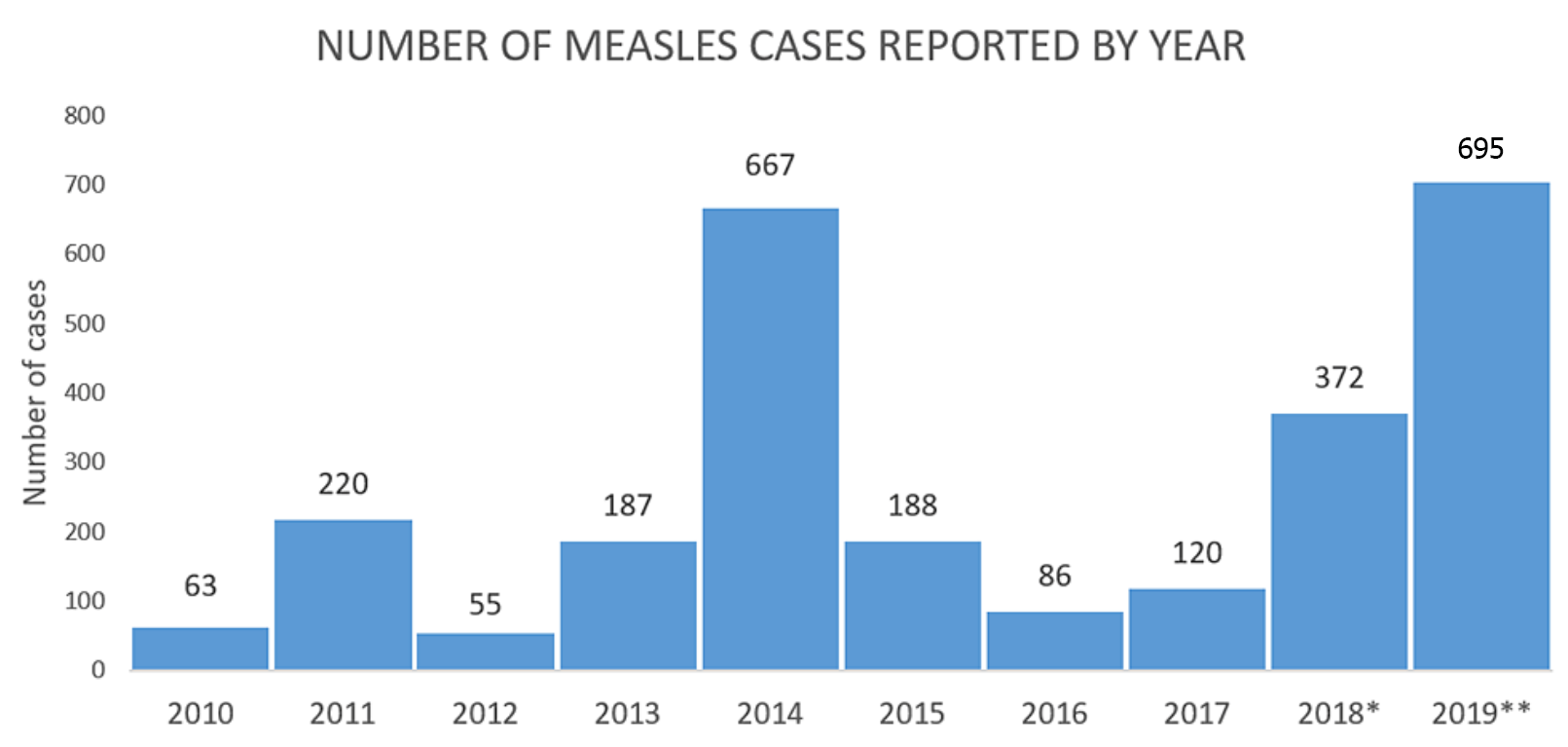
In some parts of the world, measles is still endemic, and among the leading causes of death in children. But it is easily preventable, requiring just two doses of a widely available vaccine. Because of unfounded fears of autism, however, rising public mistrust in vaccines has resulted in a resurgence of measles across Western countries. As of April 24, the Centers for Disease Control and Prevention (CDC) reported 695 measles cases in 22 states in the U.S. — the highest number of cases since measles was eliminated in 2000. In these places, health officials are learning firsthand how quickly and insidiously the measles virus can spread once it finds a foothold in a community.
At the Lowell center, the staff learned the hard way: Amid the daunting complexity of containment, minutes count, and every step matters.
Randi Berkowitz, the chief medical officer, was only on her fourth day of work at the center when the virus arrived. With a bushy mane of hair and eyes peering above dark glasses, she gives off the air of someone intensely engaged in the details. Still, the measles case was an emergency — and a shock.
“I had barely had my orientation,” Berkowitz recalled of the moment she first heard the news that measles had come to Lowell. She had spent much of her career focusing on improving care for the elderly and knew little about the virus.
“Holy moly,” she recalled thinking. “I’m a geriatrician.”
Then she and her colleagues went to work.



On November 7, the child’s mother called the center for an appointment. She said her daughter had a cough and a rash and some sores in her mouth, and asked if they could come in.
Here, the staffer on the phone made the first crucial mistake. Lowell is an old New England mill town with weathered red-brick buildings interconnected by canals, and as a large suburb of Boston, it is heavily populated these days by immigrants; nearly 40 percent of the center’s patients don’t speak English. Protocol would have dictated that center staff ask the mother about recent travel while she was still on the phone, but that didn’t happen. Had the question been asked, staff would have learned that the mother and child had just returned from a month-long trip to an African country where measles is endemic. Although the toddler had received one shot of the measles, mumps, and rubella (MMR) vaccine at the center when she was one, and a single dose is supposed to be 93 percent effective, it may have been no match for the heavy exposure.
(The center’s staff would not disclose the identity of the family, nor their travel itinerary, citing health care privacy rules.)
Had the staffer asked, mother and daughter would likely have been directed straight to an isolation room, intended for anyone with a contagious illness, on the center’s ground floor. Instead, they came to the center and disclosed to a medical assistant upon arrival that the child had contracted measles abroad.
Patricia Dykstra, a pediatrician at the center — one of eight — was assigned the appointment.
Dykstra, who sees patients on fourth floor of the building, says her senses went on high alert as she read the child’s record on her laptop. This was the first measles case she had encountered in her 25 years at the center, though she had dealt with an outbreak earlier in her career, as an infectious disease fellow at the University of Maryland in Baltimore in 1989.
Dykstra immediately asked the receptionist on the fourth floor not to let anyone else into the exam room where mother and child waited. She secured a protective mask over her own mouth and nose, and slipped through the door. The child didn’t look sick or have a fever, and except for the spots in her mouth, she didn’t look at all like she had measles. The mother, however, disclosed that her daughter had developed a cough and runny nose on November 3 and a fever and a rash the following day. But the fever and most of the illness’ telltale spots were gone by November 7, when the family flew back to Logan Airport in Boston, so the mother assumed the child was no longer contagious. Still, a nurse in Africa had diagnosed the illness. “I put a lot of stock in that statement,” Dykstra says. “A nurse in Africa knows what measles looks like.”
For guidance, Dykstra promptly called an epidemiologist at the DPH, and put the mother on the phone. The epidemiologist had urgent questions: Which airline had the mother and child flown in on? Had they taken public transportation, a rideshare like Uber, or a taxi from the airport? Where else had they been since their return to Lowell the day before?
Based on the replies, the DPH would trace the child’s trail of exposure, alerting everyone along the way. The news would send airport authorities, airlines, and countless other companies and agencies across the greater Boston area — and beyond — down their own sometimes bumpy paths of emergency response and containment, but Dykstra knew the fate of the Lowell center’s outbreak odyssey now lay in her hands. As the phone interview went on, she left the room and set the next steps into motion.
Rather than send the child to get her blood drawn at the lab down the hall as she normally would, she had the phlebotomist come to the room. She also took a swab from the child’s nose. Then they posted a notice saying the room was off limits for use, had the mother and child put on masks, and escorted them down the elevator and out of the building.
Dykstra still had patients to see, but as soon as the child left, she contacted Colette McKenna, the center’s senior director of nursing, and McKenna’s boss, Elizabeth Hale, the chief of clinical services. By the time a courier from the DPH came to pick up the child’s samples in early evening, Hale had also called chief medical officer Berkowitz about the news.
Berkowitz recalls being grateful that the child had seen Dykstra. “We were so fortunate,” she says, “that she is a pediatrician who also has a specialty and [is] trained in infectious disease.”
Dykstra got the call from the DPH at around 1 p.m. the following day, a Friday: It was definitely measles. “Oh shit, oh crap, darn, can’t believe it,” she remembers thinking. “Because I knew, oh my goodness, there goes the weekend. We are all going to be working night and day to contain this.”
But Berkowitz and the others had already begun plotting the day before, and with the illness now confirmed, they sprang into action. “Immediately what we did was we called our colleagues at the state Department of Public Health to develop a game plan of what should happen — who, what, where, when, how,” says Berkowitz. “And there were a lot of people to speak with.”
Berkowitz informed the center’s chief executive officer Susan Levine, who realized this was bigger than the health center. Between them, they informed the center’s board of directors, Lowell General Hospital — which, with 33 isolation rooms, is much better equipped to deal with an outbreak — and the city’s department of health. Dykstra downloaded the measles chapter from the DPH website and distributed copies to the staff.
At approximately 2 p.m., they gathered in a conference room to strategize and to connect with other officials via conference call. Health care organizations are required to have an emergency plan in place, and the center’s chief information officer, Henry Och — an infantry officer in the National Guard, with stints in Kosovo and Afghanistan — would play the role of incident commander.
Och and the others outlined what they needed to do: Count exactly how many people might have been exposed to the virus; determine how many of those people had had at least one shot of the measles vaccine, verified either with immunization records or by the presence of an antibody ‘titer’ in their blood (a low titer can mean weakened immunity to the virus even if someone was previously vaccinated); and document how many doses of vaccine were available to immunize anyone who needed it. The team also needed to know how many of those exposed were infants under 12 months, pregnant women, and people who were severely immunocompromised, possibly due to cancer or HIV infection. These groups would need a therapy called immunoglobulin G, given intravenously and monitored carefully for adverse reactions — something that could only be done at the local hospital.
Everyone knew they would only have 72 hours from the time of first exposure — until Sunday afternoon — to contain the situation. Beyond that window, anyone exposed might develop symptoms and become infectious themselves, requiring isolation for 21 days. To focus on getting vaccinations to those who needed them, Levine decided to cancel all non-urgent appointments scheduled for the weekend. They would also open on Sunday, when the facility is normally closed. Och, meanwhile, called the state’s medical emergency center and asked for nurses and medical reserve corps to support their plan.

As that first meeting was wrapping up, Frank Namukangula, director of quality and analytics at the center, was sitting down to a late lunch at a Brazilian restaurant close by. Minutes after his food arrived, his phone started buzzing. It was Och with the news. Namukangula, an ex-military police officer, packed up his lunch and rushed back, calling his associate, health care analyst Mark Godin, who was working from his home that day.
The measles virus can survive for two hours in the air and on surfaces, so the DPH had advised the center’s staff to add two hours after the mother and child left to define the exposure window: 12:53 p.m. to 5:22 p.m. Och tasked Namukangula and Godin with tracking down the names, addresses, phone numbers, and immune status of any patient who had been at the center during that period — and this is where the center’s modernization paid off. In 2006, it had invested in an electronic medical records system that logs the time when a patient registers on the first floor, as well as when they arrive at the floor their appointment is on, how long they wait in each place, and what time they check out.
“My phone was pinging every half an hour with Frank saying, ‘What’s the update? What’s the update? What’s the update?’” Godin recalls. He understood the urgency: “People were anxious to know what we were dealing with.”
Working into the evening, Godin and another colleague pulled together a list of about 300 people who had registered for appointments within that window, and then attempted to distinguish people with known and unknown immunity to measles. They could get some of this information by cross-checking names in the Massachusetts Immunization Information System, though at some point, Namukangula realized that their list had to include not just patients, but also people who had only come to the center’s pharmacy on the ground floor to pick up a prescription. The pharmacy’s handwritten visitor log is not part of the electronic system, so Namukangula fed the 91 names from that day’s log into a spreadsheet, all the while trying to decipher some people’s handwriting.
By that evening, Berkowitz and Och used their call center to cancel the non-urgent appointments scheduled for Saturday, and to reach people who might have been exposed. Their top priority: reaching the parents of exposed infants — a number that eventually ballooned to 22 — who needed immunoglobulin. The center also needed to tell the parents that even after immunization, the babies would be contagious and would need to stay isolated at home for 28 days.
On Friday evening, about three callers worked their way through the patients on the list. The DPH couriered over 100 doses of the vaccine in preparation for the weekend. The center had another 200, and had requests out to local pediatricians for more.
Namukangula and Godin, meanwhile, continued to crunch numbers, refining the list as they checked people’s immunization and titer status. At 10:21 p.m., Friday evening, Och sent out an email with the updated numbers: Of the 350 people in the exposure window identified by then, roughly 105 had evidence of at least one dose of MMR, and about 50 had a titer in the record that needed to be reviewed. That still left about 200 people of unknown immune status.
“That is all I have for now,” he wrote. “I am expecting the final report from the informatics team within the hour.”
Compared with the frenetic rush of the evening before, Saturday morning started out slow. The center opened at 8 a.m., but only a few people ambled in.
Berkowitz knew they needed to overcome the language barriers they had grappled with the previous day, so she worked on a script for the calls and ran it by the DPH. By late morning, she and others circulated a finalized script translated into Spanish and Swahili, beginning with “Hola” or “Jambo,” and then going on to ask the person on the other end to come in for a measles vaccination. They called more interpreters into work and reached out to local newspapers and television stations to get the word out: Anyone who had been in the center between 12:53 and 5:22 p.m. on November 8 should call their doctor. This would include not just the center’s own patients, but family members who accompanied them, members of an after-school program at the center, and even UPS and FedEx delivery people.
Things picked up after that, and the DPH allowed medical corps volunteers to vaccinate anyone who was not a patient at the center. Berkowitz says she was surprised by the response of the people they reached. She had expected them to be angry that they had been exposed to the virus, but “patients were so nice,” she recalls. She talked with one Uber driver who had two jobs and was “living on the edge economically.” He was reluctant to come in, because it would mean time, and wages, lost. But she managed to convince him that if he didn’t get immunized, he would be putting his family and his passengers at risk.
Despite some snags, things seemed to be falling into place, and Berkowitz provided the team with regular email updates as the containment effort unfolded. “I would just collect the questions during the day and then sit down and write answers to them all,” she says. “It really got people feeling like they were in the loop.”
By Sunday morning, though, the mood began to shift. The center had five medical interpreters to communicate with families that spoke Khmer, Portuguese, or Swahili. But energy levels of staff were waning, even as new medical reserve corps volunteers arrived in need of instruction. Each new set of personnel had to be shown where to go and what to do, which ate up valuable time and energy, and in retrospect, says Kerran Vigroux, director of health and human services for the City of Lowell Health Department, the volunteers who worked four hours at a time — were far too short. “That was really frustrating,” she says. If a similar incident were to happen now, she says, she would insist on a manager to train the volunteers and have them work longer shifts.

After a grueling weekend of containment efforts, Elizabeth Hale, chief of clinical services, was worried about staff stamina. “By redeploying the same staff to work … for 10, 12 days in a row,” she says, “that’s not the best decision in that type of circumstance.”
Visual: Scott Eisen for Undark
It wasn’t the only wrinkle: One of Vigroux’s nurses had to sit out the weekend’s activity because she was immunocompromised, and another had to have her blood drawn first to confirm her immune status. Some members of the center’s own staff — they would not disclose how many — also did not have updated immunization records of their own. “That hampered our response,” Vigroux says, adding that it would have been helpful for both the community center and her organization to maintain updated immunization records for all of its employees: “Maybe a lesson moving forward for those of us in health care.”
As it got closer to 5 p.m., when the center was supposed to close, Levine, the center’s chief executive, was getting nervous. This was the last day to catch people in the 72-hour window of exposure; anyone who came to the center Monday might be symptomatic and could infect others. And because Levine wanted care to be available and accessible to her community, she “thought maybe we need to stay open later,” perhaps till 8 p.m., she says.
But her suggestion met with hard resistance. There were 908 regular appointments scheduled for the following day, a typical busy Monday, and Hale, the chief of clinical services, was worried about her nurses. “By redeploying the same staff to work… for 10, 12 days in a row,” she says, “that’s not the best decision in that type of circumstance.”
Hale’s concerns won out, and the center stopped seeing patients at 5 p.m. — just as the team was learning from the 882 calls made by then that nearly 280 patients might still need to be vaccinated. The problem: They only had 70 doses left.
At 8:00 a.m. Monday, calls were going out to the Department of Public Health, Lowell General Hospital, and even to local pediatricians, for help in locating more supplies. By 11:00 a.m., more than 500 doses had been made available, and the city health department and DPH staff considered making home visits for people who might already be symptomatic. They quickly realized, however, that they couldn’t maintain the cold temperatures needed to transport the vaccine into homes — “one thing [that] we didn’t take into account,” says Berkowitz.
Her unflagging good cheer was not enough to keep exhausted staff from wondering why they were still running a vaccine clinic — on top of their routine appointments — on Monday afternoon at all, given that the 72-hour window had closed. “I think that the organization became increasingly strained,” says McKenna, the center’s senior director of nursing. “There were a lot of calls we were fielding; it was really surprising how many unique situations there were.”
McKenna and others say they could have closed their clinic sooner if the DPH had been clearer on when it was okay for them to do so. “The state was really dragging on closing the operations for vaccinations,” says Vigroux. “We stayed in emergency mode I think longer than we should have.”
By Tuesday, other notes of discord were surfacing. Levine had mostly deferred to Och and Berkowitz as leaders of the response, and an email from Berkowitz that morning instructed anyone seeking a vaccine to be “masked, vaccinated on the first floor, and discharged.”
But that afternoon, Levine suddenly became nervous about people who were infectious coming in and exposing others. “This is the only part of the story that is uncomfortable for me to share,” Levine says. Feeling frantic with this new worry, she and a few others scrambled to set up tables outside the center’s front doors to screen people before they entered the building.

This being Massachusetts in November, it was cold and rainy, and the staff didn’t have much luck stopping anyone — and may even have done harm, Levine now says. “I think we scared patients,” she says. After about an hour, she and the others came back inside, chastened.
Some staff did not take to this impulsive decision-making kindly. The incident command structure is set up precisely to prevent people in an emergency situation from making such “emotional, reactive” decisions, says Hale, though she says she didn’t speak up at the time: “It wasn’t my priority to say, ‘No, that’s stupid,’” she says. Instead, she recalls, she was on the phone with the DPH asking for clear directions on their next steps — something she did not get.
“What was also challenging is that it wasn’t clear from the DPH what we should or shouldn’t be doing related to exposure,” she says. “It was evolving and there wasn’t a lot of clarity.”
By Wednesday, it was clear the center staff needed to make decisions on their own, and so they did: Six days into their response and with flagging energy, they began winding down their vaccine clinic. By late that afternoon, Berkowitz alerted the staff that they still had 600 doses of vaccine available, but that anyone who came in “should be masked on arrival and seen in the walk-in clinic.”
It seemed that the worst was behind them when on Thursday, one full week after that fateful appointment, another child arrived at the center with worrying symptoms, and initial tests — later proved wrong — suggested it was measles.
“What does this mean for us now?” Berkowitz wrote to her team in an email. “Answer: We will repeat the similar procedure as we did on [last] Thursday with the first case.”
Months later, looking back on the frenetic activity of that week, the staff at Lowell are justifiably proud of their response. “It certainly made me feel good that we stopped it at one case,” says Dykstra. Of the 545 people possibly exposed to the virus, the staff managed to either confirm immune status for, or immunize, 366. That still left 179 people who never responded to their calls, but is still an impressive return, says Steve Fleming, an epidemiologist with the DPH. “Talk about getting through to people — when we’re cold-calling people, 1 in 40 answer the phone,” he says. He credits the trust the center has built up in the community for its success in the situation.
Berkowitz, too, refers to the center’s deep ties to other health care providers in the area, and its role serving up primary health care for most of Lowell’s residents. If the child had gone to a private physician’s office, it would have been much more difficult to contain the case, she says: “The whole community responded.”
For herself, too, Berkowitz sees only happy endings from the situation. The week cemented her relationships with her staff and helped her earn their respect. It also taught her more about measles than she ever thought she would know, she says. “I can safely say that I am the most knowledgeable geriatrician in the entire United States about measles.”
But there were practical lessons to be learned, too. One was that pediatricians should give children heading abroad their second dose of MMR before the trip. Another: Divvying up call lists by language from the start makes for shorter work — a lesson that came in handy when responding to the second suspected case.
Many staff also expressed surprise — even disappointment — that the government did not help them more. “I would have thought that the state department of public health or the city health department would have been leading the effort,” says Levine. Realizing that the center would have to do the bulk of the work, she says, “that for me was like this ‘oh my gosh’ moment.”
But Fleming, the epidemiologist with the DPH, suggests that this is unrealistic. “I think that people do imagine we have something like [a SWAT team],” he says, “and we do not.” Fleming had been on vacation, but showed up at the center on Sunday morning after seeing the news on television. He offered suggestions on what to do about missing or vague vaccination histories, or when titer testing might be useful — and the staff say they were grateful for his presence. But his help rarely went beyond advice.
Want more Undark? Subscribe to our weekly newsletter!
The city department, meanwhile, has exactly two public health nurses available to help with emergencies, says Vigroux. “There are emergency plans that talk about mass vaccinations, but there’s no staff to implement them,” she says. “We receive enough funding to pay for two cell phones for my public health nurses every year. That’s it.”
Indeed, many community centers are not as organized or well-managed as the Lowell center, and few can afford to compete with salaries offered at hospitals and private practices. If Lowell’s staff had not gone “above and beyond” as Fleming says, the situation could quickly have flared out of control.
But what would have happened had a child with measles shown up at a day care center, say, or a library? These are fair questions, Vigroux suggests — and with outbreaks now simmering in New York and Connecticut, she says, Massachusetts faces further tests. Indeed, on April 1, state officials announced that a person with measles had visited several locations over the preceding week, and they encouraged anyone drifting through the same establishments during the critical window — at a burger restaurant Tuesday afternoon, a Starbucks on Wednesday morning, and other locales — to contact their doctors.
“If this happened in a school and not a health center — who’s responding, and how is it being managed?” Vigroux asked. “I think our community is not ready for that.”
Apoorva Mandavilli is the founding editor and editor-in-chief of Spectrum, the leading source of autism research news. Her work has also appeared in The New York Times, The New Yorker online, The Atlantic, Slate, and Nature among other publications.










Comments are automatically closed one year after article publication. Archived comments are below.
I admit to being old (84), but I had a brother who died from the measles when he was 18 months old, and my mother never got over his death. I had the measles as a child and it left me with a compromised immune system which has dogged me for the rest of my life. I would urge all parents to have their children immunised.
As a person with a couple of advanced degrees, it is interesting to me to see what people call science that is no more than their disguised beliefs. This is an excessive reaction for something that did not merit it. If warranted, it would be statistically impossible that only the reached people actually were infected, but none of the 179 people who were not reached were. If this disease was as contagious as this article makes it to be, millions would become infected.
Another one, the child was immunized with one dose that supposedly provides immunity in 93% of the cases. But the article seems to suggest that the heavy exposure overruled the immune system. What is light and what is heavy exposure? It is supposed to be the same virus and if the body has immunity to it, heavy exposure has no additional effect.
Omar, re your second point I would suggest you read the article in Nature that is hyperlinked (also linked below). Also linked below are data from the WHO that shows the variability in the burden of measles. Re your first point the very reason millions aren’t infected is because of vaccination.
https://www.nature.com/articles/s41598-019-39698-x
https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/measles_monthlydata/en/
It’s the measles. It’s not ebola. It’s really not that big of a deal.
It’s a long article, so you may have missed this line: “In some parts of the world, measles is still endemic, and among the leading causes of death in children.”
I do think it would have been helpful if the article had listed some of the more serious consequences of measles: blindness, encephalitis, continued immune suppression leading to infection from other causes, extreme dehydration, ear infections, and pneumonia (causing respiratory complications, probably the main cause of death.)
Those rumors that tried to connect autism to vaccines came at a time (1970’s) when they didn’t know what caused autism and blaming the vaccines was just one theory that proved over the years proved to be wrong. . The anti-vaccines movement activists are intelligent people who should understand that prevention is better than relying on a belief that measles is not a problem disease and they are not infectious to others. I have read too many stories recently and people who have either been exposed or showing symptoms going out to public places exposing others both young and old because they feel that being quarantined is an invasion of their rights. No one has the right to expose others to an infectious disease.
I think the epidemic of all childhood autism is caused by all the chemicals that this Society uses in their everyday life, for instance fabric softeners, laundry detergent perfumes plug-ins every kind of scent made with chemicals that are affecting all our children and adults the same. Look back when we first heard autism and how it’s developed over the years. I certainly don’t blame the vaccinations that we’ve gotten to help everyone look to the chemicals
I have my doubts about a single vaccine causing autism. But doctors don’t give a single vaccination anymore. They order a handful of vaccines to be given at once. My suspicion is that the autism issue relates more to the quantity of vaccines given than to the quality of a single vaccine given.
Vaccines do not cause autism. Not one vaccine and not multiple vaccines. The study that originally tried to prove a link has been thoroughly disproved and discredited. The supposed results of that study have never been able to be reproduced.
https://www.vox.com/2018/2/27/17057990/andrew-wakefield-vaccines-autism-study
We have spent countless years and money studying vaccines as a possible cause of autism. If there is one thing we know doesn’t cause autism, it’s vaccines. Not only is there no causation, there isn’t even a correlation. At this point, continuing to put the blame for autism on vaccines is stealing valuable funding studies that May help use both understand the roots of the disorder as well as effective treatments.
I don’t know when Barbara first leaned of autism, but it was way later than scientists. Do you recall when the mothers of children with autism were blamed for causing it by lack of love and attention? They were called “refrigerator mothers” because they were supposedly cold and indifferent to their child. We have a wonderful scientist named Uta Frith to thank for ending that cruel movement. Look her up, read about her, listen to some if her interviews, she’s an threading woman, and her students have gone on to also develop some great therapies for autistic children.
Also, are you familiar with the term diagnostic substitution? A lot of autistic children used to just be called something else. It’s hard to show that the “epidemic” of autism is even a recent thing.
But please, for the sake of the suffering that children with autism and their families endure, can we please stop blaming things for which their is no evidence and fund these wonderful researchers who are actually helping them?
The shy butcher born in the latter 1800’s and his bi-lingual daughter born in 1900 and “Gentleman Farmer” son born a couple years later were NOT vaccinated and were called by “other titles” than Aspergers or Autistic, yet the next two generations had the same “symptoms” and the “newest” DSM diagnosed that shy butcher’s great-great-granddaughters with autistic spectrum. Oh, yeah, and measles is why my Mom and her sister almost DIED in the 1920s, and my Aunt is still DEAF- from having measles.
I think you may be forgetting that Autism diagnosis wasn’t done or tested the way it is now. In the last 20-30 years alone diagnosis and testing has moved to the point that we can now identify the symptoms of autism in toddlers and start them on a path to a productive and fulfilling life.
That didn’t happen in the 50’s or even the 80’s because as a disease autism was still lumped into a number “disabilities” that presented similarly. Hell you could say the same about allergens and allergies and if you forget that childhood mortality has dropped so precipitously you might have a point.
With the exception of the last few years (Thanks to people not believing in doctors or getting medical care.) childhood mortality has been on a downtrend. So it is the major exception that someone dies due to an allergic reaction, or a family member is remitted to a “home” or “asylum” for mental disabilities.
Those filtered many of the cases and suppressed the reporting because we didn’t properly categorize the deaths. You don’t have to look far into the past to see poorly adjudicated death certificates which state cause of death as “unknown” to find hundreds of cases that now would have been typed and reported.
Its a function of incidence rates climbing (previously if you had died to a disease you couldn’t pass on the genes that predisposed you to infection) and also better diagnosis.
That doesn’t mean our chemical world is safe, but does mean that the answer is more complicated than simply “chemicals.”
However please also consider you are putting that “autism vaccination” connection into this comments section by raising it. Not helping the many people who still wrongly believe that a connection exists. Not helping on that.
No-one can say if household chemicals are a contributory factor in autism, but I am absolutely certain that it has a very strong genetic component.