Rise of the Cancer Avatars
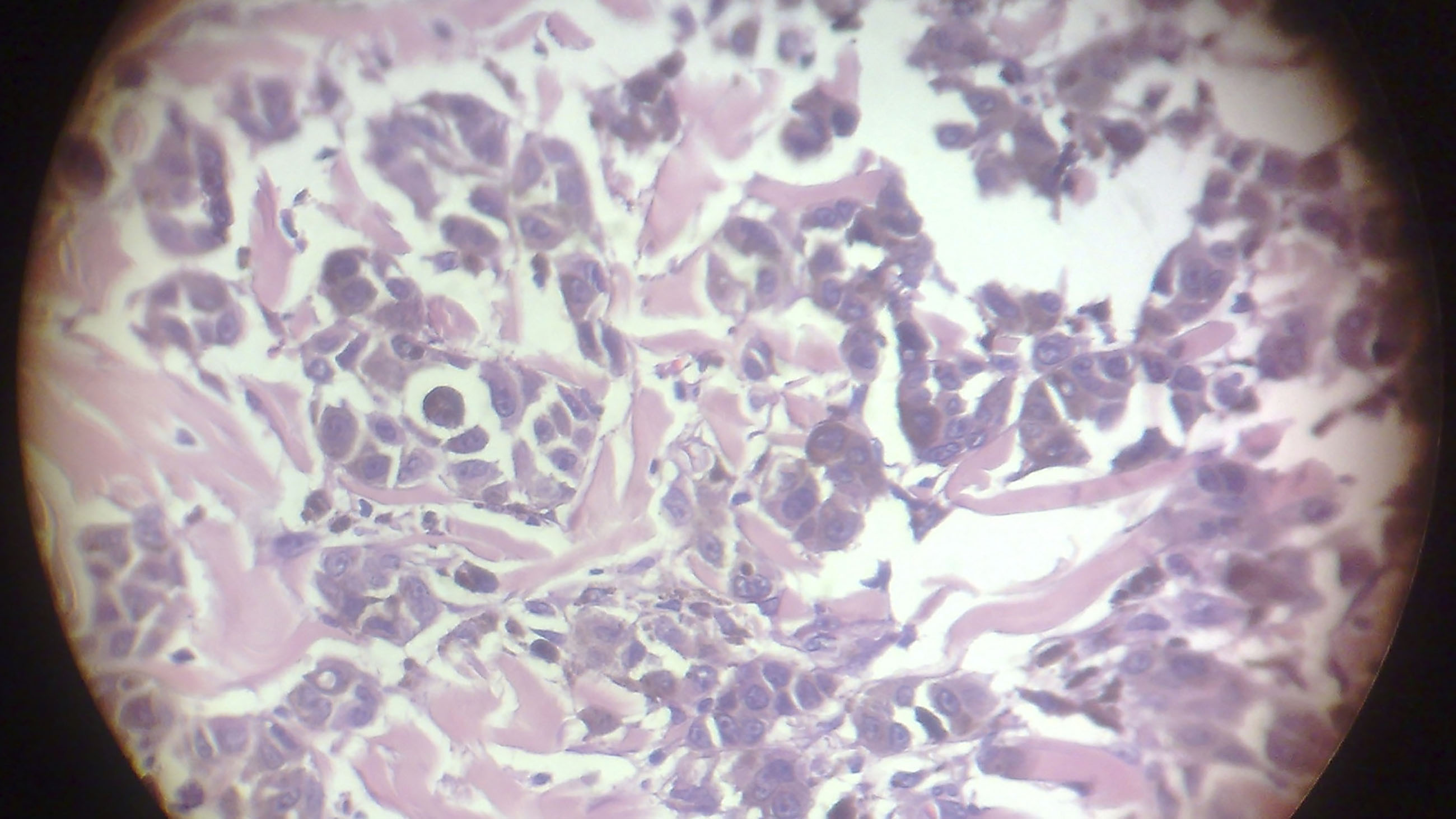
Behind several sets of doors at The Jackson Laboratory, a sprawling genetic research and lab mouse rearing facility in the shadow of Maine’s Acadia National Park, specialized mice — engineered with suppressed immune systems — are raised in near aseptic conditions. In time, they are shipped off to cancer research facilities around the world, where they drink purified water, eat sterilized food pellets, and incubate grotesque tumors — culled from human cancer patients — beneath their skin.
These mice are avatars. Each carries a very specific type of cancer taken from a very specific patient, and each receives an assortment of trial-and-error treatments on behalf of that patient. The goal is to find and develop an individualized chemical cocktail that just might bring hope — and remission — to the mouse’s human analog.
These patient-derived xenografts, or PDX models, represent “a kind of in vivo testing system that really you can’t do with cells in a dish in a way that is directly relevant to the patient,” said Carol Bult, a professor and scientific director of the PDX program at Jackson Lab. “We’ll treat mice to suggest therapies to the clinician that might be effective. He or she can use that information, or not, in guiding the treatment.”
The efficacy of using the laboratory mouse as a stand-in for humans in the development of drugs has been hotly debated for years, but PDX models take things to the extreme — and they represent one of the most audacious frontiers of precision cancer medicine. The technique was recently used in an unsuccessful attempt to save Toronto’s embattled former mayor, Rob Ford. And just this month, Boston’s Dana-Farber Cancer Institute and an international group of researchers unveiled a public repository of PDX tissue to expedite drug screening for leukemia and lymphoma.
With billions of dollars spent on preclinical studies that fail to offer specific treatments for cancers (fewer than 8 percent of animal model studies are translated into clinical cancer trials), researchers are desperate for a model that can help them to quickly and inexpensively discard therapies that don’t work – and statistically justify those that might. By screening a host of cancer drugs in different permutations on a collection of personalized lab mice, PDX advocates say the technique can offer desperate patients treatment options that their oncologist might never have devised.
Combined with genetic sequencing of tumors, PDX can also help suggest which cancers will respond to which treatments. That’s information that enthusiasts say is already improving scientific understanding of tumor biology — though other researchers caution that PDX remains an expensive and largely unproven cancer modeling system.
“Those who are claiming that this is going to be personalized therapy and it’s going to change the game, there’s really no data to support it,” said Mohamed Abazeed, a radiation oncologist at the Cleveland Clinic. “We’re in the process of validating these models. We’re really not trying to make significant claims about them, although I do think they have a lot of promise.”
To date, very few oncology clinics offer PDX, not least owing to the expense, which hovers at an estimated $10,000 to $30,000 per patient — none of which is covered by insurance. Further complicating matters: A positive response in a mouse might not translate to remission in a cancer patient, in part because of slight epigenetic and microenvironmental changes that happen to a human tumor once it starts growing in a mouse. Perhaps most frustratingly, relying on PDX to suggest a personalized cancer treatment is a gamble in which patients and doctors are in a race against time. Because it takes between one and 10 months to grow a tumor in a panel of mice, in many cases the process yields answers only after the patient has died.

But for certain cancers and under specific scenarios, researchers say, PDX – combined with genetic screening and proven therapies like chemotherapy – is already helping scientists to discover new targets for old cancer drugs and, in very few cases, suggesting treatment options that have extended the lives of patients.
Sarcomas, a relatively rare group of cancers that develop in bone and soft tissue like muscles, nerves and tendons, appear to be one promising area. These cancers tend to develop relatively slowly and, in younger patients like teenagers with Ewing’s sarcoma, they are an appropriate target for PDX trials, said David Sidransky, director of head and neck cancer research at Johns Hopkins and chairman of Champions Oncology, a company that develops PDX models for patients and academic institutions.
“There are very valid criticisms about using this model if you use the wrong example,” said Sidransky. If a tumor is growing much too slowly or much too quickly, he explained, “it’s a terrible use of the technology. It’s a waste of money. The question is: ‘What’s in between?’”
A cancer like sarcoma, he said, is increasingly looking like the most suitable application for PDX models.
“It’s a perfect cancer for us,” he said, pointing to a 2014 study he published in the journal Cancer that showed PDX-directed therapies showed clinical benefits in six of the 29 sarcoma patients enrolled in the trial. Those results aren’t stellar, but compared to the vast majority of the literature published on PDX models, which draw correlations between what scientists see in a mouse and what might work in a human, statistically speaking, he said his work is strong enough to translate to the clinic.
“[Other researchers are] not treating patients with any of that,” said Sidransky, who is currently running a larger clinical trial on sarcoma patients in Toronto. “We’re actually treating patients.”
For his part, Abazeed spent years in Boston researching PDX models at Brigham and Women’s Hospital and the Broad Institute in Cambridge before moving to the Cleveland Clinic, where he has developed close to 200 PDX lines in the laboratory, mostly using tissue from lung cancer patients. When he enrolls patients in his PDX trials, Abazeed’s consent forms make his intentions clear.
“We say: ‘This is exclusively for research purposes, it’s not going to guide your clinical management,’” Abazeed explained.
Instead of guiding treatment, Abazeed sees PDX as a tool that complements the genetics, imaging and diagnostics he already uses to better understand the biology of tumors, why cancers evolve, and how they develop resistance to therapies. PDX cannot fully address these questions, Abazeed said, and therefore it can’t be relied upon to suggest personalized therapies.
The value of PDX, at least today, remains in the research lab, Abazeed added. With the unpredictability of cancer and a patient’s response to treatment, categorizing tumors by their genetic biomarkers and using PDX to screen different treatments might provide answers that could apply beyond just one patient.
Carol Bult, at Jackson Lab, agrees. “The biggest value of these models is not ‘n-of-one,’ one patient care decision,” she said. “It’s terrific when they can be used in that context and we don’t ever want to walk away from that opportunity. But the real impact of these models, long term, is the fact that they are perturbable models of human cancers where we can test different therapies and different ideas for overcoming resistance in a repeatable fashion.”
And with different cancers behaving in wholly different ways, unique protocols will need to be devised to prove each PDX model’s suitability.
“There’s a lot of studies that we need to do to validate these models,” said Abazeed. “We need to take different sections of the tumor, measure its degree of heterogeneity, and we need to measure the degree of response in a human compared to the mouse.”
Once that’s nailed down, scientists will have to convince doctors, patients and the FDA that PDX is a viable alternative to current standards of care, which differ for an aggressive small-cell lung cancer versus a slower-to-develop sarcoma. To do that, researchers will need to conduct randomized trials comparing a physician’s treatment choice versus treatment directed by PDX models.
So far, that seems a long way off, but Sidransky, for his part, is convinced PDX will get there.
“I think we may come to a point,” he said, “where immuno-oncology drugs can be tested in these models for less money than testing directly on patients.”