Chronic Wasting Disease: Real Risk or Irrational Hype?
This winter was a little quieter than usual for the folks at Silver Creek Specialty Meats in Oshkosh, Wisconsin. For generations, winter was when hunters would make regular visits to the low-rise white brick facility near the shore of Lake Winnebago, carrying the odds and ends of the deer they had killed the previous fall so it could be turned into venison sausages. This year, though, no hunters came.
In August, Silver Creek Specialty Meats sent out a letter notifying customers that it would no longer accept venison for processing. “As you are probably aware,” the letter said, “chronic wasting disease in the wild deer population of the State of Wisconsin has been steadily spreading. The disease has now been found in wild deer in 19 counties throughout the state. Due to the spread of the disease it has become extremely difficult to screen out any venison coming from CWD infected areas.”
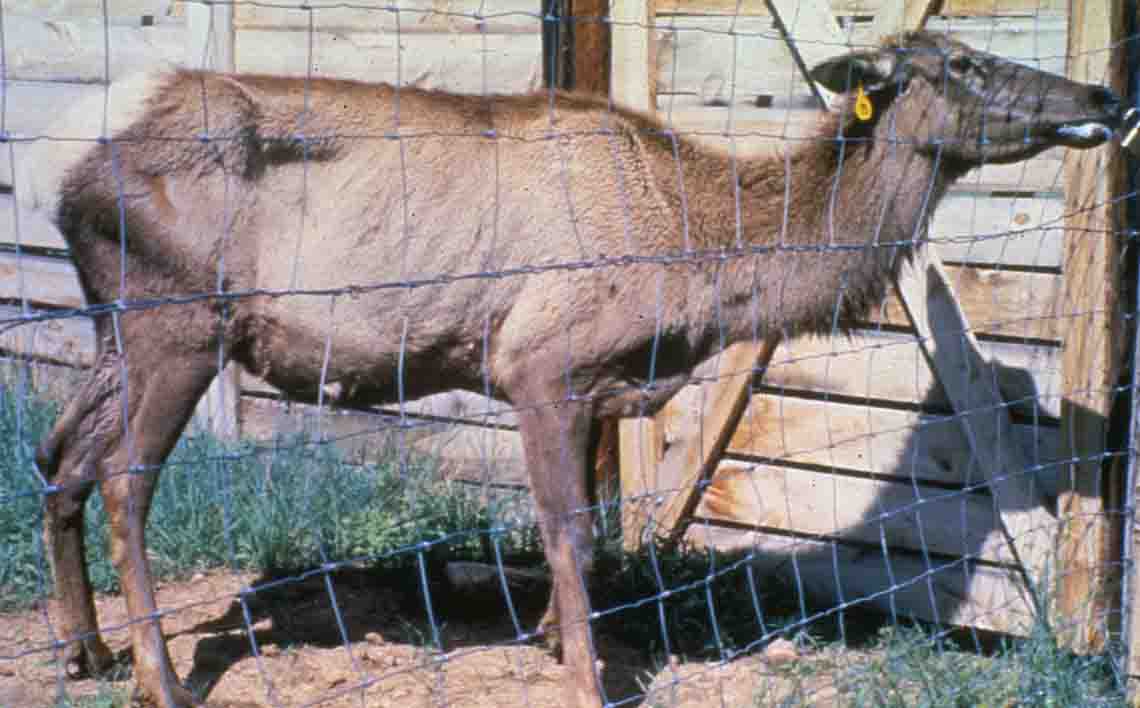
Deer with chronic wasting disease, or CWD, tremble and drool. They often cannot hold their heads up. Eventually, they lose so much weight that they are little more than hide and bone. The disease arises from a particular prion — single-protein infectious agents linked to various neurodegenerative diseases in mammals. And prion diseases are always fatal.
Even though chronic wasting disease hasn’t been shown to be a risk to human health, its similarity to other prion diseases that are — including “mad cow disease” and Creutzfeldt-Jakob disease, which has symptoms resembling Alzheimer’s disease — has been cause for concern for years. News last summer about an ongoing Canadian study in which two macaque monkeys contracted the disease after eating meat from a CWD-infected deer — the first time an animal so closely related to humans developed CWD — only exacerbated the worries.
“That sealed the deal for us,” says Katy Lehman, Silver Creek Specialty Meats’ president of operations. The letter went out soon afterward.
And yet, a short drive from Wisconsin’s CWD hotspot, another venison sausage processor continues — as do dozens of commercial venison processers in the state — to make venison sausage from the meat brought in by hunters. The butcher, who asked that his name and the name of his shop not be used for fear of losing business, rankles at Silver Creek Specialty Meats’ decision to stop processing wild deer meat, because it creates unnecessary fear and worry.
The media sensationalizes the disease, he says, “every time there’s a scare with a monkey.”
The owner says that out of an abundance of caution, he and his employees follow careful procedures, including butchering the venison in a separate location reserved only for deer meat, and that employees don’t touch the deer’s brain or spinal column. This is more than enough to ensure safety, he suggested — not least because there is no evidence that chronic wasting disease is a threat to humans.
It’s a near perfect encapsulation of the chronic wasting disease conundrum: Two meat processing companies, less than 100 miles apart, that only want the best for their customers — and each animated by a very different assessment of the risk posed by CWD.
Both say that science is the basis for their conclusion. And both are correct.
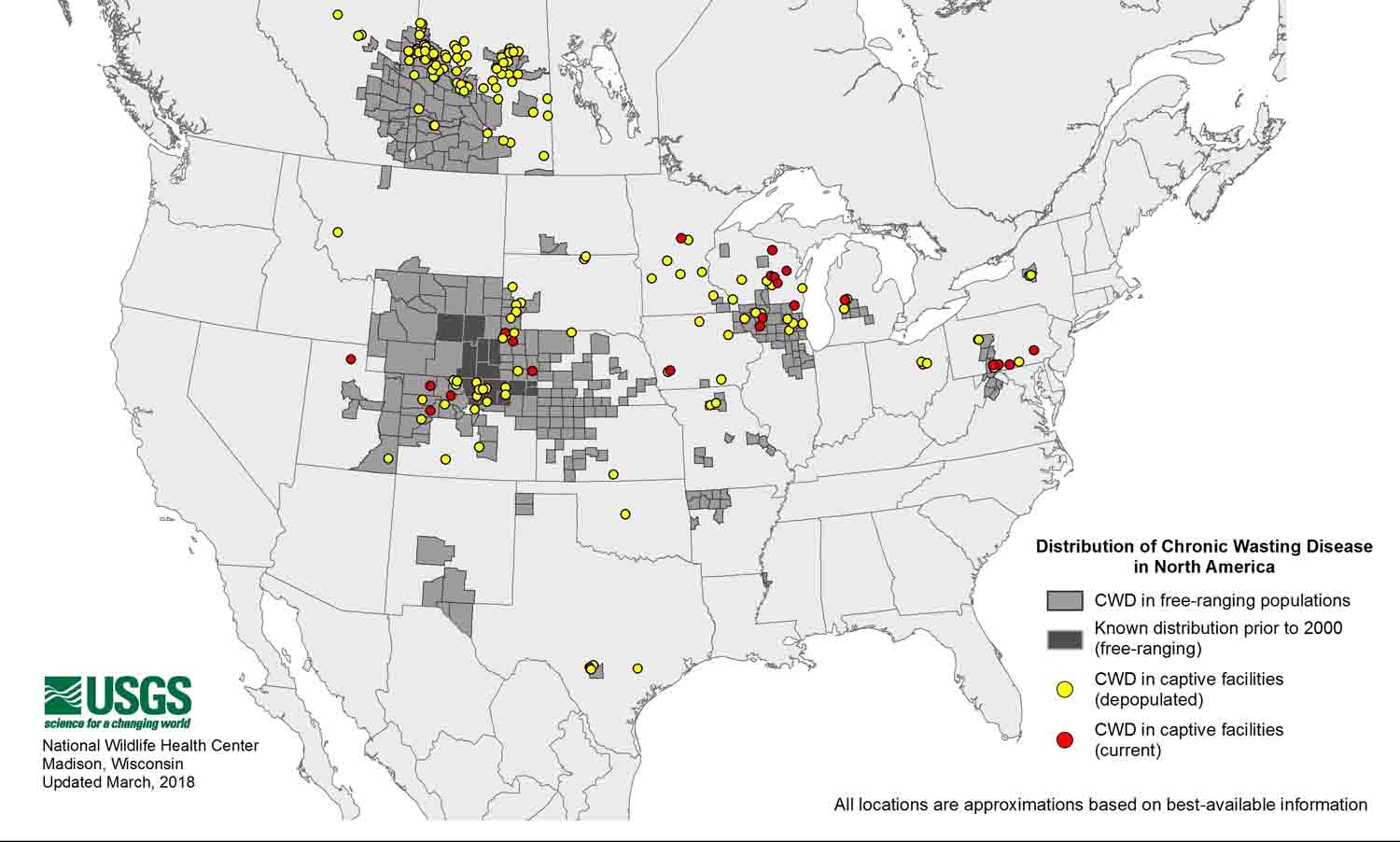
To date, CWD has been detected in captive and free-ranging deer, elk, and moose in at least 24 states and two Canadian provinces, but it is not exactly a new disease. CWD was first discovered in captive mule deer at the Colorado Division of Wildlife Foothills Wildlife Research Facility in 1967, but it would be years before it was understood to be what’s now called a transmissible spongiform encephalopathy, or TSE. At the time, these diseases, which turn brains spongy, were a mystery, and only three were known: scrapie, a disease of sheep, known for over 250 years; Creutzfeldt-Jakob, a disease of humans; and kuru, also a disease of humans, that was only found among the natives of Papua New Guinea who ritually ate human brains.
Scientists had already discovered that the infectious agent behind TSEs could not be killed by boiling or exposure to acids, radiation, or antibiotics. But it wasn’t until 1982 that Stanley Prusiner, an American medical researcher, discovered the prion, and pegged it as the cause of TSEs. (He later won the Nobel Prize for his work.)


Then came mad cow. Properly called bovine spongiform encephalopathy (BSE), it was identified in the United Kingdom in 1986. The British government initially claimed that beef from mad cow-infected cattle was safe to eat, but more than 200 people across Europe would later die from it. The first case of BSE in humans, known as variant Creutzfeldt-Jakob disease, was diagnosed in 1996. That 10-year gap between discovery of a disease in cows, and the recognition, despite all assurances to the contrary, that it was a threat to people who ate contaminated meat, is the cause of nearly all the worry about chronic wasting disease today.
While nobody knows exactly how CWD is transmitted from deer to deer, saliva is highly suspect. Nose mucus, urine, and feces are also possibilities. However, its leaps across the country and the world are best explained by live animals transported as part of the captive deer and elk industry. While typically called “deer farms,” in the United States, these businesses are predominantly captive hunt facilities and their suppliers. Farm-raised venison is mostly imported from New Zealand, which is CWD-free. Hunters dumping carcasses or parts in places far away from the kill site may also contribute to CWD’s spread, experts say.
The most recent scare with monkeys started last year. Stefanie Czub, a prion researcher based in Alberta, Canada and head of a reference lab for mad cow disease for the Canadian Food Inspection Agency and the World Organization for Animal Health, flew 2,000 miles to Ottawa, Canada’s capital, to deliver the results of her monkey research to representatives of various federal agencies in person. It was that important.
Her news was that five cynomolgus macaque monkeys had contracted CWD in a years-long study where 18 macaques had been infected with CWD through various means. The results from three of the macaques would have been news enough: Two had contracted CWD after its prions had been applied directly to their brains. This was new. And another macaque in Czub’s study had contracted CWD after eating brain tissue from an infected white-tailed deer.
“The two remaining animals may be, from a human health point of view, the most important ones,” says Czub. They were fed meat from CWD-infected white-tailed deer that didn’t look sick. These were the kind of deer that any hunter might eat without a second thought. But 5.4 and 6.2 years after first being fed this deer meat, the macaques, previously thought to be immune, showed subtle symptoms. They were killed and CWD prions were found in their spinal cords.
The results were a surprise, given that an earlier study had found that this species of macaque appeared immune to chronic wasting disease. After flying to Ottawa, Czub presented the findings at the Prion 2017 conference in Edinburgh, Scotland last May. Over the summer, more than 1,000 people, mostly veterinarians from federal agencies, dialed into a webinar organized by the U.S. Centers for Disease Control and Prevention, Czub says. She and her fellow investigators still haven’t written a scientific paper, and while Czub says she intends to write up these intermediary findings, the study is only at its halfway point. Ten of the original 21 animals (three are controls) are still alive.
Czub would like to keep the remaining macaques alive as long as possible. She wants the disease to have the chance to develop, since prion diseases are known to take years to show symptoms. That might also give her a better idea of what the disease might look like in humans.
And yet, that kind of research is expensive — $7.9 million Canadian, so far, she says — and she’s currently in the process of securing funding for another two years. Meanwhile, the macaques are housed in Germany, in one of the few facilities in the world certified to work with both primates and prions. Because of the difficulty of working with primates and prions, Czub says, “This experiment is never going to be repeated.”
The World Health Organization, the CDC, Health Canada, and the departments of health and natural resources in Wisconsin and other states including Minnesota, Colorado, Mississippi, Illinois, North Dakota, and South Dakota aren’t waiting for more studies: All recommend that no one eat the meat of any prion-infected deer.
Some hunters feel these recommendations don’t go far enough. “This is one of the most outrageous human susceptibility experiments in history,” says Dave Clausen, a retired veterinarian, former chairman of the Wisconsin Natural Resources Board, and avid deer hunter.
Other hunters defy the recommendations — and sometimes that defiance has a scientific basis. “I harvested an elk several years ago, and the adult turned out to be positive for chronic wasting disease,” Walt Cook, a clinical associate professor at Texas A&M University’s College of Veterinary Medicine, said at a Texas Parks and Wildlife Commission hearing. “Well, I ate it. That was my choice; and I don’t think I look like I’m wasting away, do I?”
Later, Cook admitted that he would not let his wife or daughter eat meat from CWD-positive animals, and explained that he had worked with deer and elk in a CWD-infected area of Wyoming for 23 years. The infected elk he knowingly ate, he said, was unlikely his first CWD exposure, and he’s confident of his chances. CWD most resembles scrapie of sheep, Cook says. “This disease [scrapie] has been around for hundreds, possibly thousands of years. Literally millions of people have been exposed to scrapie with no evidence of transmission.” He also points to research that shows that CWD prions are simply the wrong shape to interact with human prions.
Timothy Kurt did that research at the University of California, San Diego. Kurt looked at the role played by the 210 amino acids in the prion protein to figure out why CWD is transmitted to some species and not others. He found that when a species had a different amino acid in a key location, the diseased prion wouldn’t fit neatly into the healthy prion, like a zipper with teeth that don’t fit together. This, Kurt believes, is CWD’s species barrier. The amino acid sequence differed between humans and deer at a key location. A different study showed that a macaque’s amino acids matched the deer sequence in the same spot, but not the human one.
It’s evidence like this that prompts James Kroll, also known as “Dr. Deer” on the television show “North American Whitetail,” to dismiss concerns over chronic wasting disease as absurd. Kroll said he does not normally test deer where he hunts. “And why would I want to?” he asked. “I am not concerned about eating ‘infected deer!’” He adds that he’s proud of the special report his program did on chronic wasting disease, in which his colleague ate CWD-infected meat on camera.
Kroll has never studied CWD in the lab or in the field, but what he says counts more with hunters, especially in Wisconsin, and not only because he’s on TV. In 2011, he was selected as a deer trustee by Wisconsin Governor Scott Walker to straighten out the mess CWD had made of that state’s deer herd. Kroll believes that CWD is widespread, “has been out there for a long, long time,” and that what appears to be an uptick in cases of CWD are simply an artifact of looking for it. “If you test for it, you’ll find it,” he says.
This, of course, ignores the opinions of his colleagues who study CWD, and states like New Jersey, Oregon, Maine, and California, which have tested extensively for chronic wasting disease for years, and have never had a positive result. It also ignores the states, such as Illinois and New York, where CWD has only been found in a small area although deer throughout the state have been tested. And while Kroll argues that “CWD has been a great cash cow for a lot of states and scientists,” federal funding for CWD research and monitoring was actually cut back in 2012.
In November, two Wisconsin congressmen introduced a bill to restore federal funding for chronic wasting disease surveillance and research. A similar bill was introduced by Senator Jon Tester, a Democrat representing Montana. The bills are still in committee.
“Following basic, required protocols of separating venison from other meat, and removing the central nervous system and disposing of it properly, are the primary way of addressing processing concerns,” says Jeff Sindelar, an associate professor of meat science at the University of Wisconsin-Madison.
When consumers are worried about the risk of CWD, he says, these are socially-based concerns, not concerns based on science. “There has never been a link between eating venison and CWD,” he says. “The risk is not zero, but it’s pretty close to zero.”
Whether “pretty close to zero” is a comfort or concern is a matter of perspective, of course, and when asked, Sindelar said that he doesn’t make any recommendations to processors about removing a deer’s lymph nodes, even though those are what Wisconsin’s Department of Natural Resources, and others around the country, test to diagnose the disease.
“There are lymph nodes throughout the body,” Sindelar says. “It would be unreasonable to remove them all.”
As it stands, hunters in Wisconsin are not required to have their deer tested for chronic wasting disease, but many still do. (CWD tests are mandatory for all hunter-killed deer in some areas of Michigan, Minnesota, Missouri, Texas, Virginia, and Alberta, Canada. All 50 states do some kind of CWD testing on wild deer, either random, voluntary, or of sick deer.) In Wisconsin, if a kill tests positive, hunters can expect a phone call from state wildlife officials. If those hunters, like Kroll, say they plan to eat the meat anyway or share it with others, they’ll be asked to provide a list of names so the state’s Department of Health Services can confirm who consumed it and add those individuals to the department’s long-term disease surveillance program.
That’s when some hunters simply hang up, says Jim Kazmierczak, the public health veterinarian for the State of Wisconsin. Some say they don’t trust the government, Kazmierczak says. Some have other reasons not to participate. But many say yes, and so far about 1,000 people in Wisconsin are helping the state learn more about any potential human health risk posed by chronic wasting disease.
Joni Scheftel, the state public health veterinarian next door in Minnesota, says that any hunter who said he or she was going to eat venison from a CWD-infected deer in her state would get a phone call directly from her. “I would be showing up at their house if they didn’t want to talk to me by phone,” Scheftel says. “There is no evidence at this point that CWD has ever been transmitted to a person, but we still feel very strongly that people should not eat meat from any prion-infected animal.”
That surely sounds overwrought to some hunters who believe that, with millions of people eating venison each year, a human infection would have shown itself in the 50 years since CWD was first discovered. Or, that the CDC or other health researchers, ever on the lookout, would have pegged a human prion disease cluster to CWD, if it were indeed the cause.
But sentiments like Scheftel’s are enough for the team back at Silver Creek Specialty Meats in Oshkosh. “Consumer safety is our number one concern,” the company’s August letter stated, “and no matter how small the risk (if any) of humans being infected by the disease we are not, and never will be, willing to put profit before the safety and well-being of our customers.”
Still, Katy Lehman allows that Silver Creek’s decision is not necessarily the right one for everyone. “It’s not quite black and white,” she says. Silver Creek considered the size of its processing facility, its location and their product mix in its decision, Lehman notes, and those factors may add up differently for other companies. With no answer yet on whether or not CWD is a human health risk, Lehman says, the only question can be, “What do we do in the meantime?”
Madeline Bodin is a Vermont-based freelance writer specializing in wildlife conservation science. Her work has appeared in Scientific American, Popular Mechanics, National Wildlife, and many other publications.











Comments are automatically closed one year after article publication. Archived comments are below.
CHRONIC WASTING DISEASE CWD TSE PRION END OF YEAR REPORT
TEXAS CWD
Commission Agenda Item No. 5 Exhibit B
DISEASE DETECTION AND RESPONSE RULES
PROPOSAL PREAMBLE
1. Introduction.
snip…
A third issue is the accuracy of mortality reporting. Department records indicate that for each of the last five years an average of 26 deer breeders have reported a shared total of 159 escapes. Department records for the same time period indicate an average of 31 breeding facilities reported a shared total of 825 missing deer (deer that department records indicate should be present in the facility, but cannot be located or verified).
https://tpwd.texas.gov/business/feedback/meetings/2022/1104/agenda/item.phtml?item=5
Listen here;
Nov 3, 2021
https://tpwd.texas.gov/publications/multimedia/media/commission_20211103/20211103_com_00_work_session.mp3
Nov 4, 2021
https://tpwd.texas.gov/publications/multimedia/media/commission_20211104/20211104_com_00_commission.mp3
Counties where CWD Exposed Deer were Released, September 2021
https://tpwd.texas.gov/documents/257/CWD-Trace-OutReleaseSites.pdf
Number of CWD Exposed Deer Released by County, September 2021
https://tpwd.texas.gov/documents/258/CWD-Trace-OutReleaseSites-NbrDeer.pdf
SATURDAY, DECEMBER 04, 2021
TPWD CWD TSE PRION TRACKER UPDATE TEXAS 270 CONFIRMED TO DATE POSTIVE CAPTIVE AND WILD
https://tpwd.texas.gov/huntwild/wild/diseases/cwd/tracking/
Why is nobody, especially fish and game agencies, promoting the usage of hypochlorous acid (HCOl) as a way to deactivate prions to mitigate exposure and their spread?
All that we seem to hear is that they are indestructible except by bleach or super high temperatures…. but this NIH study from > 3 years ago shows otherwise.
https://www.niaid.nih.gov/news-events/immune-system-oxidant-could-be-key-inactivating-prions
https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1005914
https://www.heraldnet.com/business/scientist-woodinville-companys-breakthrough-is-surprising/
https://www.uwb.edu/news/september-2016/dementia-disease-breakthrough
Seems to be an effective way to get rid of these prions without destroying what it is you are trying to decontaminate!
Hi – this is interesting and it looks like hypochlorous acid is available to the average consumer? Is this something you can treat items that come into contact with an infected animal’s fluids etc and it would de-activate the prions?
Seems odd this is not widely being touted by fish and game agencies as a way to get rid of prions?
Thanks for the good article and a special thanks to all the researchers out there trying to make sense of all this!
Here is a question for researchers. It seems that for scientists; and not to mention the average person/hunter out there, CWD prions are impossible to stop spreading given how prions bind to things?
Given the nature of CWD prions, how some studies show they can remain in soils, plants, bind to steel and/or other surfaces, and can only be “destroyed” via extremely destructive procedures that are not available to the average person (outside of bleach on steel surfaces only, see latest 10/19 study https://www.nih.gov/news-events/news-releases/household-bleach-inactivates-chronic-wasting-disease-prions) it appears they *bind* to absolutely anything they come in contact with.
People can wear rubber gloves, minimize handling of brain and spinal cord tissues etc. get animals tested and make a personal choice on whether or not to consume the meat…. but at the end of the day aren’t the prions already spread over everything that any part of an infected animal come into contact with?
Lets say I wear rubber gloves, and completely process an animal properly following all recommended procedures as published by most fish and game agencies….. I bag the meat up and throw it in a frame pack to haul out of the field. Anyone who has ever hunted knows this is not a clean room laboratory environment. Blood gets on things, pants, backpack, clothes etc. Maybe a drop of spinal column fluid ends up on a glove, that then touches my pack etc. Prions on are now on my game bags and potentially on my frame pack, and eventually in my truck bed etc.
They are also likely on boots if we get any blood/fluids on them, and with every step they being spread everywhere someone walks?
What about the head I handle w/ gloves in the field? Well it ends up in the back of people’s trucks, on to a taxidermist etc. Even after the brains and spinal cord/column is properly removed, aren’t prions still bound in the skulls? even after boiling or European mount procedures (using borax, whitening etc)?
What about when those clothes that had contact w/ an infected deer during processing, go into someones washer/dryer… those prions are now bound to that equipment as well?
It just seems to me that these prions are likely already spread all of the place by anyone who happens to even come into casual contact with any part of handling game animals. From reading about CWD prions wouldn’t one venture to guess they are already in hundreds of thousands of hunters trucks, clothing and houses w/ taxidermy etc?
Thoughts? Would like some clarity on what prions bind and don’t bind to.
Just because this hasn’t been 100% proven to affect humans YET means nothing. Every other TSE can jump the species barrier with impunity so it’s but a matter of time before CWD does too. This isn’t about spreading fear or panic; it’s about preventing a disaster so it doesn’t come to a point where we NEED to panic. Prion diseases are nothing to mess with.
Maybe you’ve heard of the Kentucky cluster of CJD caused by hunters eating squirrel brains–long considered a safe local delicacy? I understand outdoorsmen/women can be traditional & slow to embrace change, but better safe than sorry with something like this. The incubation period for CWD is long & deer or elk may not show symptoms for many months or years before falling ill. Meanwhile they can transmit the infectious prion to other cervids or various animals they come in contact with. (Possibly humans eventually).
Thank you to the hunters & processing companies that have taken a stand & changed their behavior in light of this disease. Some things are more important than hobbies or profits.
Thank you, Waste Not. I don’t think I came across a mention of a TSE of squirrels in my research (I did find mentions of TSEs in sheep, goats, minks and cats), but now that I’ve looked, there is plenty of documentation out there on vCJD in people who ate squirrel brains in Kentucky. I appreciate the info.
Ticks (Lyme’s) won’t keep me from the woods, and dying from a possible disease isn’t going to stop me from eating deer…
Death; we all have it coming…& dying from doing what you love is not the worst thing I can think of…
https://www.nih.gov/news-events/news-releases/nih-study-finds-no-chronic-wasting-disease-transmissibility-macaques
This was published April 25, 2018. Let us not create hysteria, find the truth, go through peer review, then release the findings.
It’s hard to come by knowledgeable people about this subject, but you sound
like you know what you’re talking about!
Re inactivation of CWD, in 2016 we published with collaborators at US NIH on the inactivation of scrapie, CJD , BSE and CWD using a preparation of pure and stable hypochlorous acid (PLOS Pathogens. DOI:10.1371/journal.ppat.1005914. Sept 2016.) This solution inactivates prions quickly and to a high level, proven by inoculation of treated scrapie prions intracerebrally in Tg mice. The product is about as benign as you could wish for, you can spray it in your eyes, and yet the myth persists that nothing works to inactivate these proteins. Our findings have been confirmed at the FDA research labs in Silver Spring, and we are getting ready to publish a couple more papers on inactivating prions with solutions that have been stored for long periods, and exposed to high temperatures (70C). This is a real and reproducible effect, needs to be taken notice of in discussions about decontamination, and there may be useful ways to deploy it in handling contaminated equipment, tools, and even carcases.
This map shows to be current 2018 but based on what I know they are not including a lot of places that I know about. There were 2 captive breeders (at least that were shut down in East Texas (border of Oklahoma) not to mention all the hoops tpwd are jumping through for 2018/2019 https://tpwd.texas.gov/huntwild/wild/diseases/cwd/
I have a couple of issues with this information as a whole, not because I do not believe it but because the optics on it are bad. I do not see anyway you can have a CWD positive animal that was killed in the field and not end up with prions in the meat. Even if you took a clean heat shot your going to end up with spinal matter everywhere and if you can not kill it with a,b,c,d, or e then there appears to be no way to kill it once you have gotten it on something, you can not just wash it off. So now you have prions everywhere what difference does it make that you separate venison from everything else. One guy brings in a CWD animal and the facility need to be burned to the ground. Which brings me to my final point. If you have a facility that is trying to do CWD research how do they isolate those monkeys from each other and everything else especially over 5+ years. The protocols would have to go beyond DNA testing protocols and probably something that should only be done at a super max facility dealing with the deadliest of pathogens. This just densest all make sense to me.
There is also the question of whether infected or suspected carcasses of elk or deer or cows are properly disposed of. The easies and cheapest manner is not enough to ensure killing off those pesky prions.
I’m a Wyoming based biologist and cartographer that has been following chronic wasting disease closely for the past several years. This article does a commendable job of summarizing many of the challenging scientific, political, and social aspects of the topic. Head and shoulders above 95% of articles popping up on Google Alerts. Nice work.
In line with the “it’s all about how you look at it” vein of the article, how about “controversial” scientists claiming that the causal agents of CWD are actually bacterial or viral, rather than prion?
https://en.wikipedia.org/wiki/Frank_O._Bastian
http://www.deeranddeerhunting.com/deer-scouting/deer-behavior/controversial-research-bacteria-not-prions-cause-cwd
Although the study in Canada indicated that it was possible that CWD could transmit to monkeys, this result was obtained using an assay that is not considered to be conclusive for diagnosing CWD. False positives are problematic using this assay. Furthermore, the animals did not display symptoms consistent with the clinical stage of CWD. Symptoms of CWD can mimic symptoms of other diseases and disorders, particularly in aged animals. The gold standard is this field is an animal bioassay where brain material from infected animals is fed to or injected into the brain of recipient animals. This experiment was done by NIH researchers, and a research paper was written in 2014 that showed macaques were NOT susceptible to CWD (Race et. al., 2014). In my opinion, the Canadian study is not conclusive since it does not use the most sensitive method available to detect prion diseases and instead uses a diagnostic test that still is not validated for diagnosis. Furthermore, the epidemiological data do not support the theory that CWD passes to humans.
Does anybody remember BSE or Mad Cow disease? This was thought to be impossible to transmit to humans. Some weasel words were used “there is no evidence that BSE can be transmitted from cattle to humans.”
The disease was eventually linked to CJD in humans which takes years to develop.
“No evidence for” is not the same as “evidence against”, and we should always prick our ears up when we hear it.
To All hunters,
Prions are amyloid proteins that build up in the tissues of the CWD-affected deer. Amyloid proteins do not proliferate but can increase in amount biochemically. Bacteria can induce formation of these amyloid proteins. These amyloid proteins (prions) are not infectious.
Research shows that the cause of CWD is a tiny bacterium. We have now grown this bacterium in broth culture and on agar plates so we now can develop a diagnostic test. This will be very important since the deer shows at least a 10 month incubation period where the deer is infectious yet shows no clinical signs. There is no way to recognize an infected deer until the last stages of the disease.
Vaccines are common in controlling bacterial diseases. Brucella is controlled by a vaccine. You all know about pneumococcal vaccine. There are no antibiiotics that kill spiroplasma. There is no workable diagnostic serological test for the transmissible spongiform encephalopathies. CWD has been experimentally transferred to cattle so I wouldn’t be secure in any natural barrier to infection. The incubation period for CWD may last months. The animals appear normal during the first 10 months of the incubation period.
Spiroplasma can be cultured and studied. A diagnostic test is now possible so that the CWD-affected animals can be culled. The diseased animals will be recognized by a simple serological test.
The source of the organism in nature can now be determined. Since the spiroplasma forms colonies on agar plates, we can now determine sensitivity to new antibiotics. A preventive vaccine is now possible.
We need more laboratories working on this problem from this perspective and that is why I published the method of isolation so any researchers with access to CWD materials can contribute.
Dr. Frank Bastian
tseresearchcenter.org
TUESDAY, APRIL 17, 2018
Chronic wasting disease: Bambi vs. the prion
Research Project: Immunodiagnostics to Detect Prions and Other Important Animal Pathogens
Location: Produce Safety and Microbiology Research
http://chronic-wasting-disease.blogspot.com/2018/04/chronic-wasting-disease-bambi-vs-prion.html