A Yelp for Psychiatric Facilities
Last year, Kit Mead, who has been diagnosed with autism and bipolar disorder, spent time in two different psychiatric wards in Washington, D.C., including a stint at George Washington University Hospital. Instead of offering treatment, Mead says, staff members there simply provided sedatives — an experience that left Mead feeling “degraded.”
At MedStar Georgetown University Hospital, on the other hand, Mead reports feeling listened to, and receiving medication that helped with anxiety. Sara Luterman, a friend and editor at NOS Magazine, a mental health publication, visited Mead at Georgetown and the two talked about how different hospitals offered widely varying care. “There needs to be a Yelp for psych wards,” Luterman said, invoking the popular website where participants review everything from local hairdressers and mechanics to restaurants and bars.
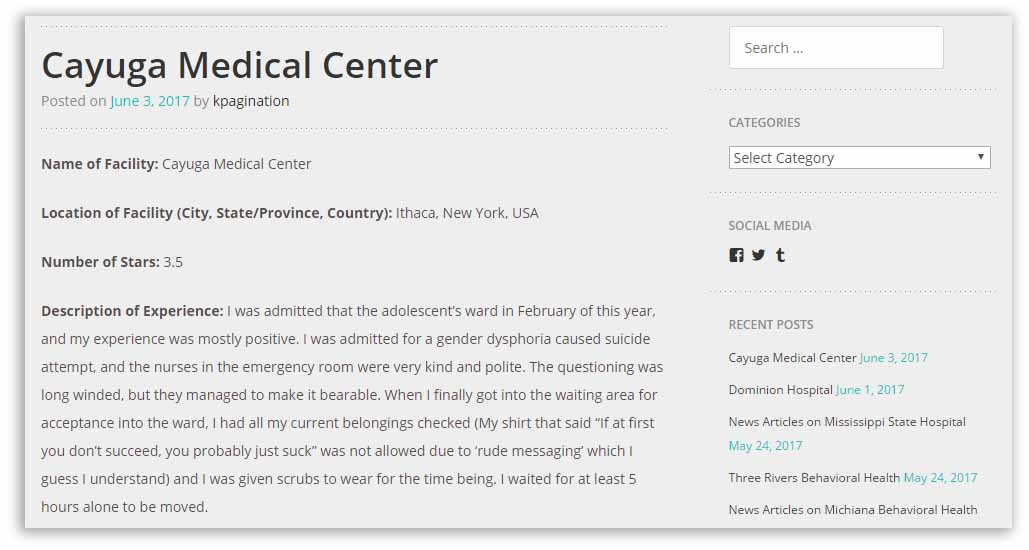
The idea stuck with Mead, and last July, the 24-year-old launched Psych Ward Reviews. As of mid-June, the website had gathered anonymous reviews of 195 public and private psychiatric and general hospitals offering 24-hour inpatient care — about 10 percent of the U.S. total, according to Mead. Reviews have also come in from Australia, Belgium, Canada, Finland, and Hong Kong.
Some advocates and researchers see the online project as filling a range of unmet needs, from empowering the people who submit reviews to potentially helping families of mental health patients inform themselves about care for their loved ones or offering clues for future research and policy. Representatives at the American Hospital Association and the National Association of Psychiatric Health Systems said they hadn’t seen anything like the project, and that it could be particularly useful for people seeking care and their families — though they were also careful to point out that other standardized systems of quality control and patient surveys already exist.
Meanwhile, the reviews keep coming in.
“I was treated frustratingly upon my intake,” one anonymous reviewer wrote about an experience at St. Elizabeth’s Medical Center in Boston. “I was required to strip fully naked and submit to a physical exam, which occurred about 15-20 minutes after my very emotional transfer to the ward. They wanted to take my sweatpants away, for having a drawstring, leaving me in itchy scrubs for the duration of my stay, but acquiesced when I suggested just cutting the string out. That was not a reassuring moment for my confidence in their common sense.”
They gave the hospital a score of three out of five stars.
Another anonymous three-star review said that San Antonio Behavioral Healthcare Hospital in San Antonio, Texas “keep[s] family away from the patients … withholding visitation when behaviors don’t meet their idea of compliance.”
Norwalk Hospital in Norwalk, Connecticut, received four stars for its “quality therapy,” though the reviewer also noted that patients can’t go outside or even crack open a window. “The food is so-so,” the reviewer added.
None of the three hospitals responded to repeated requests for comment on these reviews, but mental health advocates have been quick to embrace the project. “This site is absolutely needed, and there’s nothing like it,” said Leah Harris, who lived through similar experiences when she was hospitalized in San Diego more than two decades ago. She is now a patient advocate and trains public and private healthcare staffs across the nation.
“People who go into this system don’t have much of a voice,” said Harris, referring to the mental health system. “It’s important for people using these facilities to be heard.”
Mead’s project comes on the heels of several decades of growing interest from healthcare and insurance providers in the experience of patients, said Meredith Rosenthal, professor of health economics and policy at the Harvard T.H. Chan School of Public Health. The patient experience, said Rosenthal, produces “outcomes in and of themselves, and we should pay more attention to them.”
This interest led the federal Agency for Healthcare Research and Quality to launch the Consumer Assessment of Healthcare Providers and Systems, or CAHPS, in 1997. Almost a decade later, the agency launched an additional survey to gather information on the patient experience in hospitals, but it doesn’t focus on psychiatric patients in any way, and only added a question to the most recent version on “overall mental or emotional health,” Rosenthal noted.
“In mental healthcare, there’s a lag” when it comes to capturing and acting on the sort of information Mead’s reviewers are supplying, she said. Even the Experience of Care and Health Outcomes, or ECHO survey, which is aimed at mental health patients, doesn’t ask questions about inpatient treatment.
“Unfortunately, inpatient psychiatric units appear to be faltering in both safety and developing a patient-centered orientation of care,” wrote Kathleen R. Delaney, professor at the department of community, systems and mental health nursing at Rush University, in a research paper on measuring patient and staff satisfaction.
One reason for this lag may be that some medical professionals are hesitant to trust the opinions of patients with mental illness. “There’s the idea that patients don’t have insight, or don’t know what they need,” said Morgan Shields, who has researched quality of care at psychiatric inpatient facilities with Rosenthal and is a Rappaport Public Policy Fellow at the Harvard Kennedy School of Government. “Because of the nature of their condition, there’s a distrust in their opinions,” she added.
Mead hopes the site helps not only those people who write the reviews, but also others who have been at inpatient psychiatric facilities, along with individuals and families seeking care.
“Being hospitalized on an inpatient ward can be disempowering, so being able to have an outlet is important,” Delaney said.
Though Mead would like the site to provide signposts for future research and policy, the reviews currently don’t provide crucial data on trends. This might include, for example, whether “restraint rates” — the percentage of time that patients are physically restrained — are going up or down. Mead plans to assess the reviews for so-called core quality indicators, like varying types of abuse, restraint and seclusion, staff and psychiatrist issues with medication, patient-staff communication, [and] inadequate therapy provided. “While the reviews do not contain data on every indicator, I believe this is a start to quantifying a good portion of them,” Mead wrote in an email message.
The self-styled activist also wants to create a “toolkit of recommendations” based on the reviews.
Harvard’s Rosenthal suggested that even if the website’s reviews don’t provide such information as trend data, the project still “begins to give us an outline of what we would want to look for” when planning research.
As for policy, Harris said she saw common themes in the reviews to date, including “lack of awareness about gender issues, not a whole lot of therapy happening, comparisons to prison, very restricted visiting hours — and for someone in extreme distress, access to friends, family and community is important.”
These sorts of themes can be vital in the policy discussion of whether the decades-old trend of closing down psychiatric institutions and offering community-based mental health services needs to be reversed, she noted. “If on the one hand, the policy direction is leaning to, ‘Community services have failed,’ and ‘We need more inpatient services,’ then let’s take a look at the quality of those services.”
“This information, if it is gathered, is rarely acted on — it is another leverage point to apply pressure on these systems,” she said.
Shields pointed out that current oversight by the Joint Commission, the hospital accreditation agency, is based on seven core quality measures for inpatient psychiatric facilities, including whether patients leave with a plan of care — but none of the measures sample patient experiences directly. Similarly, the Centers for Medicare and Medicaid Services (CMS) collects answers to 16 questions from inpatient psychiatric facilities that the federal agency funds, but the only one referring to the patient’s experience asks, “did you assess [it]?” Shields said. In other words, there’s no information gathered from the experience itself.
“The stories [on Psych Ward Reviews] make the case that we should be paying attention to patient experience — and could get agencies to do something more systematic, with more oversight,” she added.
Mark J. Covall, president and CEO of the National Association of Psychiatric Health Systems, an organization representing more than 800 psychiatric hospitals and other facilities, said that the site could be useful to patients and their families seeking information, as well as “to an individual hospital — it may be information that may be important to look at.”
At the same time, Covall said, Psych Ward Reviews is “probably not all that valuable” to him, and said he had not looked at the site before an interview on the subject. He also noted that “people’s individual perceptions of their experiences are not scientific, or comparable,” like the CMS measures, which “are evidence-based quality measures that have gone through rigorous review.”
Nancy Foster, vice president of quality and patient safety policy at the American Hospital Association, pointed to the CAHPS survey, which she said provides “standardized information” on patient experience, while Psych Ward Reviews provides comments that, together, may help patients and their families make more informed decisions about treatment. She compared this to looking at a hotel review online and seeing what rating it gets in different categories. “Data helps you understand comments and comments help you understand data,” she said.
Of course, supporters of the project point out that this description doesn’t account for the fact that the survey in question doesn’t ask about inpatient treatment, while Mead’s, which Foster says could also be useful to hospital staffs charged with overseeing quality of care, does. “This kind of information from patients, telling them what didn’t go right, as well as what did go right, is extremely valuable in helping to identify opportunities to improve care for patients,” she said.
Still, one feature of Psych Ward Reviews could blunt its impact, Foster added: the anonymity of the reviews. “Oftentimes, the quality improvement function is inhibited when reviews are anonymous, because quality improvement people need to ask further questions — they need to reach out and learn more,” she said.
“I know that sometimes people choose leave their names off this kind of thing because they’re fearful of retaliation — but that is not the case,” Foster added.
Shields, who supports the project, conceded that anonymity could open the site up to questions of accuracy. “There’s no litmus test for ensuring accuracy,” she said. “But there would be a lot of concern if you didn’t at least provide the option of anonymity. Perhaps it would increase confidence in the site if you made it optional.”
Mead defended this feature of the site. “People who are known to have been in psych facilities can face discrimination and judgment in a lot of areas,” Mead wrote. “So, speaking up about this stuff can be hard, even if a stay was okay or helpful rather than traumatizing or unhelpful.”
“We cannot always trust regulatory systems to ensure safety and the protection of our rights,” Mead added, noting that anonymity “is probably the only option that centralizes and values our experiences while showing the insides of facilities.”
Timothy Pratt is a reporter based outside Atlanta. He writes about subjects ranging from soccer to science to higher education, in English and Spanish, for a range of outlets that includes The New York Times, The Guardian, and the Columbia Journalism Review.











Comments are automatically closed one year after article publication. Archived comments are below.
Hey. A very sad story at the same time very interesting. I absolutely agree with your opinion. Remember the story of Universal Health Services? As a result, accusations of numerous abuses and neglect of patients’ health led to a reduction in state funding for the entire network of mental hospitals. Unauthorized access of journalists to UHS documents is a violation of trade secret legislation. In addition to the correction of the information agenda, UHS took up a personnel issue. Employees suspected of communicating with journalists were dismissed, and those who were accused of video from cameras were sued. The rest warned against such rash actions at meetings.
Thank you fir this
The Psych Ward Reviews site seems to have disappeared. So I’m posting an archive of it:
https://web.archive.org/web/20181130045319/https://psychwardreviews.com
for most closed facilities a large percentage of patients are currently in forensics like 75% + for mine. it is the hearing system that is killing them. if u want to do something for them implement the right to be forgotten. what happens when 600k + people die due to religious prosecutions in these facilities after they close look were there assets are after death they go right into the hands of others who violate their privacy metaphisicaly and contributed to more of there deaths. this is religious prosecution at its height. look at 911 millions of civilians died due to suicide just for trying to help them via hearings get out of that state education bankruptcy hearings even 500k veterans committed suicide. and that was just a few mental hospitals in middle east and a few here closeing and look how big that conflict was. what happens when u close 750 large facilities in this nation. its a real bad scenario and look at youth because they got away with that many closeing and many deaths in the closed facilities look what they are doing to youth 30% autistic why is that any different we have a huge conflict going on plz be respectful and put your citizens and your population first not your elected. let the news shield these individuals and don’t let any politician get in the way of that. plz you are only as strong as your weakest citizen plz be respectful and come up with positive solutions that respect privacy many helpless people’s lives depend on it. plz do your part and do your research.
Chicago Behavioral Hospital in Desplaines Illinois is a horrible place. It should not even be called a hospital. My son was forced to go there because Advocate Lutheran General Hospital had no beds. My son was brought to the hospital to get help with his sudden unprovoked violent outbursts of anger. While he was there, he was told that he had an extremely high white blood count and very low Potassium level.He was never treated for this in 7 days. He only saw his Psychiatrist twice. The first time for 5 minutes, and the second time about 6 minutes. This DR. has no office or telephone number, except the receptionist’s desk. He cannot be paged, and his phone number cannot be given out.No family meetings with the Social Worker DR, Nurses, and staff can be set up during their no treatment phase or before discharge. Everyone who works there from housekeeping to intake is all extremely rude and sound very disgusted that they have to answer questions or deal with patient families. I never received any phone call from his DR. or Nurse, or Mental Case Worker for any of his past Psychiatric, medical, family, medicine, present symptoms etc. My son was not in his 100% mental capacity to be able to cooperate or make correct medical decisions for himself. He was heavily addicted to Kush a super strong strain of pot that he used daily 24 hours a day.He was very paranoid and having anxiety attacks.When we went to visit him, everyone had to sit in the cafeteria. We could not see the unit he was on. or meet and talk with his nurses and Mental Health Workers. While visiting him he had a very angry sudden outburst and wanted to leave the cafeteria. I do not know if this incident was noted on his chart. When he calls me on the phone he becomes very easily upset when he hears something he doesn’t like and hangs up on me.He told me he is being discharged tomorrow on Tuesday, February 20th, 2018. He has not had any treatment for his angry violent behavior. He remains a very real threat of causing severe abuse and harm to other people around him. especially his mother. and twin brother with whom he lives. We remain very fearful of him and scared for our lives.