The accompanying article is adapted from a chapter written by the authors and appearing in their new book “One in a Billion: The Story of Nic Volker and the Dawn of Genomic Medicine, published this month by Simon & Schuster.
A teaspoonful of blood. That’s where the search for a new disease begins.
It is the late summer of 2009, and within a few weeks, scientists hope to drill deep inside the blood to the place where 4-year-old Nic Volker’s story lies; not just a story, an entire encyclopedia. Inside millions of pages they hope to find a paragraph, maybe just a word, that explains the dragon Nic has been battling — a mysterious immune system disorder that is ravaging his intestines and threatening his life.
To get there, the blood will be reduced to DNA, the DNA to exons, and the exons to the individual letters of the genetic script: A, C, G, and T.
In an era when the mining of our genes has turned increasingly to high-speed machinery, some tasks still call for a human touch. So the teaspoon of Nic’s blood does not proceed straight to the next-generation equipment. The sample contains material— red blood cells, platelets, and plasma—that must be removed in order to capture Nic’s DNA. Then, to reach what Francis Crick called “the secret of life,” scientists must pierce the nuclei of what remains, the white blood cells.
There is a machine designed to extract DNA from blood, but Mike Tschannen, who runs the sequencing lab, finds that the individual strands emerge in better shape when the job is done by hand. He knows right away that the best hands for the job belong to Gwen Shadley. A research technologist at the Medical College, Shadley has been processing DNA for more than ten years. She is meticulous, and Tschannen has a deep trust in her. Early in his career, she gave him a tour of the lab, impressing him with her knowledge and her commitment.
Shadley regards her work as a special calling.
The oldest of four girls, she grew up on an eighty-acre farm in the small city of Bryan, Ohio. The family raised a few beef cattle, dairy cows, and some sheep, and there was endless work for the girls. Shadley cultivated and harvested wheat, corn, and soybeans. She milked cows, drove a tractor, made hay, and fed the animals at night. The work was hard, often exhausting, but it was a good life. When the day’s chores were done, the sisters would go down to the pond and swim.
Shadley’s father was an amateur naturalist who used farm life and landscape to teach his children. He would take his eldest daughter to the woods to cut logs, and he’d point out the different trees. When he butchered cows, he cut out the heart and showed Shadley the different valves. He’d cut out pieces of the lungs and explain how air flowed through them.
Soon her own curiosity took over. One day, Shadley’s mother went to the freezer and let out a shriek.
“I don’t want to go to the freezer and find eyeballs staring out at me!” she cried. Shadley had cut out a cow’s eyeballs and placed them on ice to preserve them.
She was interested in science from an early age. Science explained how everything was put together and provided deep insight into nature’s contradictions. She often thought of a line from Scripture: “I am fearfully and wonderfully made.” For Shadley, there was no better proof than in the nature that surrounded her. “It was fun to cut things out and see that,” she would say.
Shadley got her undergraduate degree from Biola University, a private Christian school in Southern California, then returned to Ohio for a master’s degree in developmental genetics from the University of Toledo. She did much of her experimental work with fruit flies.
In 1998, she was divorced, living in Milwaukee, and looking for a job when she heard about a research associate position at the Medical College of Wisconsin. The majority of the work would be extracting DNA. Blood samples would come in from all over the state for a project launched by researchers at the school. They were investigating the role of genes in obesity.
Like the chores she’d grown up with on the farm, the tasks in the lab were not especially difficult and might have seemed boring to someone else, but Shadley found the work extremely interesting. There was a set of routine steps to follow, but there were also certain tricks that could be applied to coax the DNA from difficult samples.
In one of the final stages, the DNA is supposed to strand out, but frozen blood samples often proved challenging. She learned to put glycogen in the sample; the sugar would bind to the phosphorus backbone of the DNA and pull it out of solution. She would also place the tube on an electronic rocker to move the process along. Sometimes she would leave the solution for an hour or so, sometimes overnight. She learned to adapt her process to the sample at hand.
Samples are always anonymous, and the one that Tschannen now brings her is no different. Yet Shadley knows this is no ordinary vial of blood. For one thing, it reaches her bench less than an hour after it has been drawn from the subject. That tells her the job is urgent.
Tschannen does not tell her where the blood has come from, whether the person is alive or dead. Only this: “Handle it with tender loving care. It’s a very special sample, very likely the most important sample of our careers.”
He does add one more thing: they need the DNA as soon as possible.
In most cases, Shadley tells people it takes three weeks to get the best results. The longer she has the sample, the more DNA she can pull from it.
Knowing that time is a factor, she tells Tschannen, “Let me allow it to sit overnight so I can get you the most DNA.”
Shadley works in an old section of the building in a brightly lit, windowless lab the size of a small living room. There are several lab benches, including a low bench about five feet long where she begins processing the sample. Nearby sits a boom box that she and a colleague sometimes tune to easy-listening music to relax them as they work. Today it is silent. Shadley likes the room fairly quiet when she is processing a sample. When she has many samples, she must take care to ensure that one does not come into contact with another.
The work with Nic’s blood progresses smoothly. First Shadley uses a solution to burst the red blood cells. Then she moves to a centrifuge, which spins at great speed to separate out the plasma, platelets, and cell debris. At the bottom of the test tube lie the white blood cells. She adds detergents to break open those cells, releasing the DNA inside. Then she extracts the other cell contents— proteins, sugars, fats. What’s left gets poured into a test tube of alcohol solution.
She places the tube on a machine that rocks gently back and forth. Her work has taken about four hours.
Now comes the part that leaves her in awe no matter how many times she does it. Tiny strands of DNA, like fine white threads, drift through the solution and clump together, visible to the naked eye. Those delicate white threads remind her of the farm, of her childhood, of the times she helped ewes struggling to give birth. The strands are life reduced to its essence.
She lets Nic’s sample sit overnight. The next afternoon, about twenty-four hours after she began work on the blood, Shadley presents Tschannen with two tiny vials. They contain Nic’s DNA, his genetic secrets reduced to a clear liquid unrecognizable from water. She wonders what is in this sample, whom it belongs to, whether it will help in some way. She knows that the strict patient confidentiality laws prevent Tschannen from telling her those things—if he even knows them himself. So Shadley hands over her work, con- tent in the knowledge that she has done her job as best she can.
Although the Medical College has its own sequencing machine, although Tschannen will be using that machine extensively to analyze Nic’s sample, the first run is to be done by Roche, the Swiss biotech giant that has agreed to help.
Tschannen picks up one of the vials of Nic’s DNA, removes a large drop of the liquid, and places it into a container surrounded by dry ice. He sends the whole package by overnight mail to Roche.
Roche’s 454 Life Sciences division in Branford, Connecticut, performs the first sequencing of Nic’s genome. Technicians begin by breaking the long strands of DNA with their 3.2 billion chemical base pairs into shorter, readable stretches. Using pressurized nitrogen gas, they shear Nic’s DNA into segments of roughly five hundred to eight hundred bases. Each one of those segments is fitted with a short piece of synthetic DNA, a tag that will be used later in the process.
The segments are loaded onto a special chip the size of a microscope slide that captures only the exons, the portions of the genetic script that contain the recipes for proteins. The chip they use is one conceived of and built by scientists at Roche NimbleGen in Madison, just a few miles from Nic Volker’s home. It was introduced earlier in the year, about the time Nic’s disease kicked back into gear, forcing him back into the hospital.
Its inventor is Thomas Albert, Roche NimbleGen’s senior director of research. As DNA sequencing became faster and more affordable, Albert realized it would supplant many of the single-gene tests that were common at the time. That inspired him to come up with ideas that would “play nice” with DNA sequencing, rather than compete against it.
Companies were developing ways to read the genome more rapidly and less expensively, but the ability to sequence selected parts lagged behind. No one had yet figured out how to isolate the exons. There are some 200,000 to 300,000 exons, each an average of 150 bases long, scattered across the genome’s 3 billion or so chemical base pairs. Variations in exons cause proteins to malfunction, which can lead to major diseases. Sickle-cell anemia, Tay-Sachs disease, cystic fibrosis, and many others are caused by mutations in the exons.
NimbleGen’s core technology, invented by three University of Wisconsin–Madison researchers, gave the company the ability to quickly design millions of strands of synthetic DNA on a computer. Albert realized that those strands could be used as probes that would recognize the exons and pull them out of the genome. That way, researchers could save time and money by focusing on the part of the genome most likely to be involved in disease.
The probes on Albert’s chip capture Nic’s exons by taking advantage of a basic feature of DNA: each chemical base has a counterpart that it attracts rather like the way two magnets couple.
Adenine always pairs with thymine; guanine always pairs with cytosine.
Albert’s probes are designed to attract and capture only the exons. Once they’ve done so, the rest of the DNA—the nonexon portion—is washed away. The exons are then transferred from the chip into a solution in a small plastic test tube.
The Roche technicians add tiny beads to the exon solution along with an oil-and-buffer liquid and shake the entire mixture. The shaking creates an emulsion, a little like an oil-and-vinegar salad dressing. Millions of tiny droplets form within the oil; the oil keeps each one separate. Each droplet traps a single bead and a single exon fragment.
Here’s where the synthetic DNA tags Roche attached to the segments of Nic’s exon come into play. Each tag is attracted to a matching chunk of synthetic DNA on one of the beads. This match allows every bead to grip onto a targeted segment of Nic’s exon.
The emulsion also contains an enzyme that makes droplets into ferocious copying machines that replicate Nic’s exons. As a result, each bead creates hundreds of thousands of copies of the same exon fragment. Many copies are needed to generate a signal that’s strong enough for the sequencing machine to detect.
The beads are spread over a sequencing plate the size of a standard Post-it note. The plate contains millions of tiny wells, each large enough for only one bead. Once all the wells are filled, the entire plate is loaded into the sequencing machine.
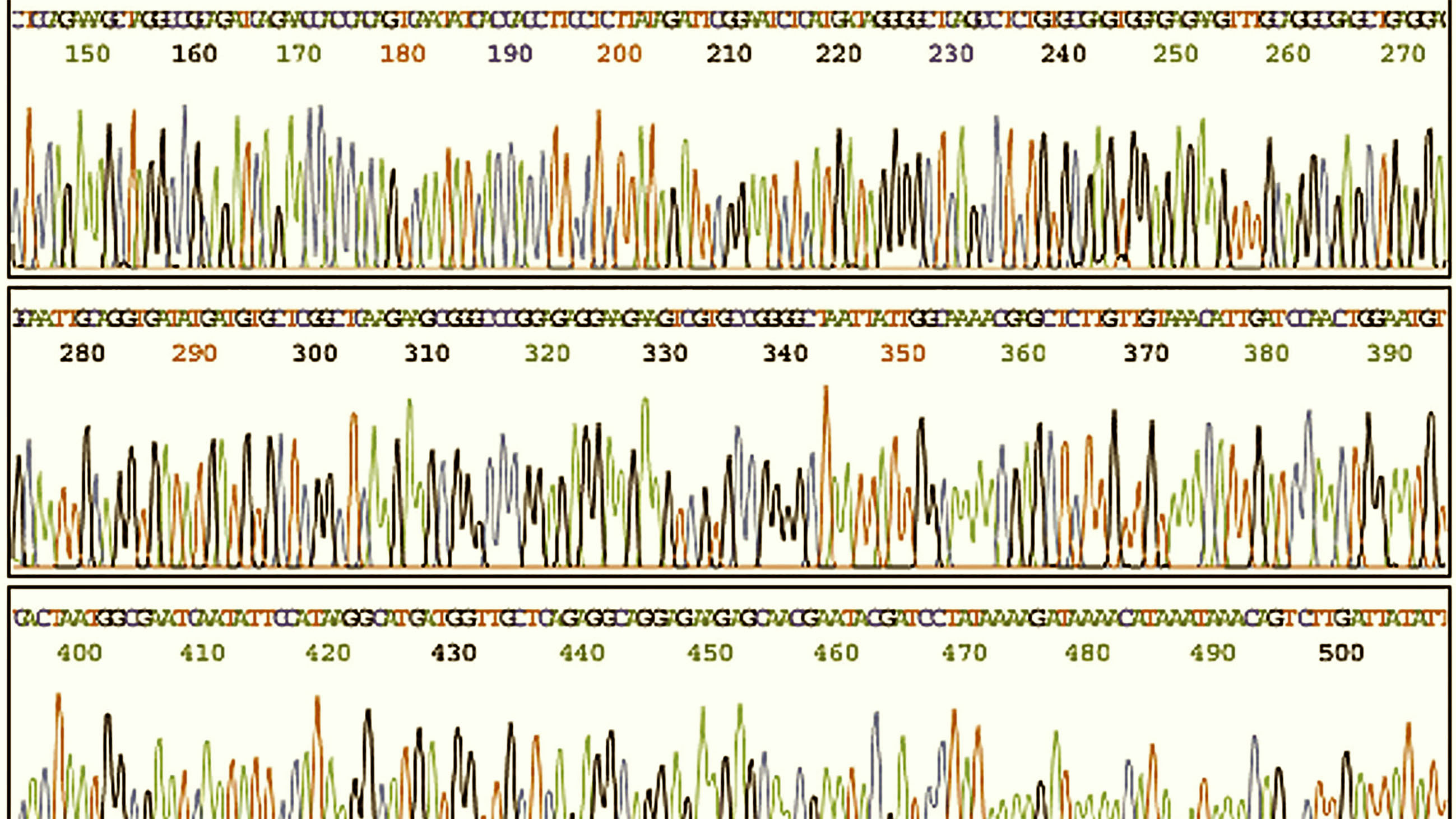
The machine reads each segment of Nic’s exon, letter by letter. The process takes place at high speed, with the machine reading about a million segments, or roughly 100 million bases, in a single twenty-four-hour run.
One at a time, the machine pumps a stream of each of the four bases. When A is pumped, all of the complementary Ts in Nic’s fragments light up. When G is pumped, all of the complementary Cs light up.
A camera photographs the pattern of light flashes, creating a map of the plate, where all the As are, all the Ts, all the Cs, and all of the Gs.
A computer attached to the sequencing machine translates the photos into Nic’s sequence. Then, using algorithms based on the reference genome that recognize where the segments are most likely to fit, the machine reassembles all of the fragments into the complete string.
Back at the Wisconsin medical college, Elizabeth Worthey – the director of genomic informatics – has not been content to wait for the opening deluge of data. If the scientists are not prepared, they will drown in all the clues, the variations between Nic’s script and the model developed by the Human Genome Project. Since the second week in July, she and research scientist Stan Laulederkind have been poring over the medical literature, noting every time a gene has been linked to one of Nic’s key symptoms. Often papers connect an entire pathway—a group of interacting genes— to a symptom. In those cases, Worthey and Laulederkind include all of the genes mentioned. By August, their master list of potential suspects has grown to more than two thousand. The list includes genes linked to inflammation, such as NOD2, and others that play a role in gut development, such as the GATA genes. The scientists are hoping that one of those two thousand genes is the one they’re hunting.
As they construct the master list, two assumptions guide them. The first is that the difference in Nic’s genetic script, the one causing the holes in his intestine and the poor healing of his surgical wound, must cripple an important process in the body; otherwise his illness would not be so severe. The second assumption is that the difference they’re looking for is extremely rare, likely undiscovered until now. Although the gene may be on their master list, the specific error in it must be new. The scientists know that because Nic’s disease appears nowhere in the medical literature. If they were looking for a mutation that had been found before, another child somewhere in the world would have turned up in a hospital with Nic’s symptoms. The presumed rarity of Nic’s mutation has given some of the boy’s doctors the feeling – or the hope – that when they go through Nic’s script they will know the right variation when they see it. It will jump out at them.
The master list of suspect genes is only one part of Worthey’s preparation for the sequencing results. Facing thousands of possible mutations all over the genome, she knows they need a tool to guide them. For the first time in her career, the task she has been asked to perform is so complex that the crucial tool to accomplish it has yet to be made.
She must make it herself.
Mark Johnson is a health and science reporter at the Milwaukee Journal Sentinel, where he has worked since 2000. Kathleen Gallagher is a business reporter at the newspaper, where she has worked since 1993. Both writers were members of the Journal Sentinel team that won the Pulitzer Prize for explanatory reporting on the Nic Volker story in 2011.