Modeling Zika’s Rise and, in Three Years, Its Fall
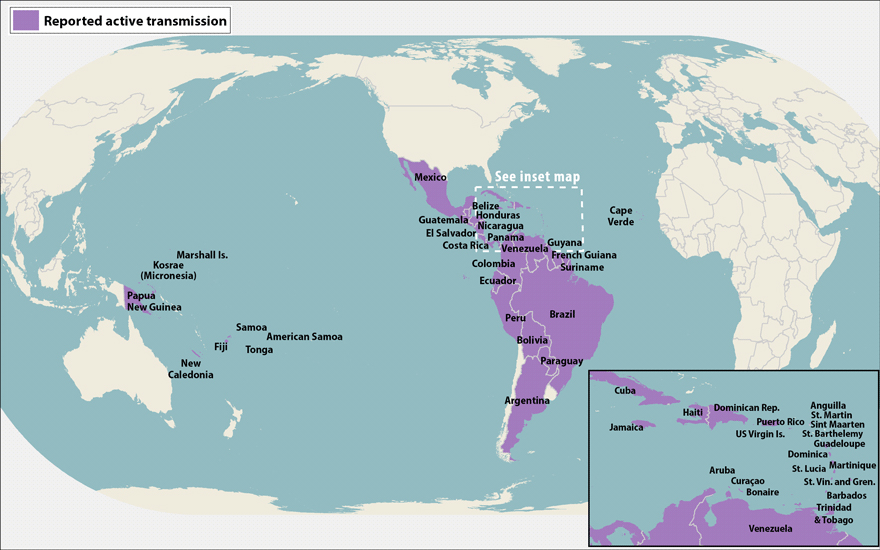
The mosquito-transmitted virus Zika has now been reported in 40 Latin American countries and territories, according to the U.S. Centers for Disease Control and Prevention, which has linked the virus definitively to microcephaly in newborns, and more loosely to Guillain-Barré syndrome and related paralysis in the wider population. Not surprisingly, concerns over the virus’s unrelenting spread — and the seemingly desperate efforts aimed at containing it — have dominated headlines for months.
According to a new study published this week in the journal Science, those containment efforts are likely to have “limited effectiveness” — and may even make matters worse. “The current epidemic is not containable,” the authors wrote. “At best, interventions can mitigate its health impacts. More optimistically, the natural dynamics of the epidemic are now likely to give a multiyear window to develop new interventions before further large-scale outbreaks occur.”
If the virus has peaked, as the authors suggest, the epidemic should be largely over in three years.
The study, led by Neil Ferguson, a professor of mathematical biology at the Imperial College London, attributed its findings to what’s known as “herd immunity,” whereby each new infection acts like a vaccine, giving the host immunity from subsequent Zika infections for years — maybe even a lifetime. If enough people become inoculated this way, it can stop a disease in its tracks — at least, for awhile. Once enough new people are born into the population who aren’t immune, the disease can come back — an oscillation that Ferguson and his team suggested would take a decade or so.
“Certainly we are not arguing that this is completely novel science – we are applying fairly tried and tested methods of epidemiological modeling which have been used in many other emerging infectious diseases to Zika, and highlighting our best guess as to how the epidemic might unfold,” Ferguson told Undark.
Among other things, the study’s authors — which included researchers from both Imperial College and the Bloomberg School of Public Health at Johns Hopkins University in Baltimore — suggested that traditional vector-control methods, like insecticides, have mostly proven ineffective at controlling other diseases, like dengue. Unless those control methods get markedly better, they’re also likely to have limited impact on the spread of Zika — and could even prolong the epidemic by interfering with the development of herd immunity. That, in turn, would make already-difficult public health policies — like recommending that women delay pregnancies to avoid microcephaly — even harder to sustain.
At least by relying on herd immunity, Ferguson suggested, such controversial policies would only have to be around for a short time. “We highlight the difficulties [of pregnancy delay policy], but there is very little else that can be done, frankly,” said Ferguson. “I certainly understand why policy makers have made that recommendation.
Alex Perkins, an infectious disease researcher at the University of Notre Dame who also uses mathematical models to understand viruses like Zika, said he had seen the new paper and that he wasn’t confident in the three-year burnout estimate that Ferguson and his team came up with, arguing that such numbers are simply too hard to know right now. But, he added, the study’s more general conclusions — that infection rates will slow due to herd immunity, and that they will likely spike again at certain points in the future — are probably accurate.
There is evidence, Perkins said, that infection rates are already easing up in Colombia.
Ferguson and his team conceded a number of potential caveats in their analysis, including a need for more granular look at geographic variations in herd immunity, among other variables. “A more precise assessment of long-term risks,” the study’s authors wrote, “requires key data gaps to be filled.”
This post has been updated to clarify that Alex Perkins had seen the new study, but was not a formal reviewer.










